Health
Four Texas residents forever connected by two kidney donations in different cities: 'Superbly timed'

Two hard-to-match transplant patients 250 miles apart started the year of 2024 with shining new hope for long, healthy lives — thanks to the collaboration of two Texas hospitals.
UT Southwestern Medical Center’s Solid Organ Transplant Program in Dallas, Texas, and University Health Transplant Institute in San Antonio worked together to find compatible living kidney donors for their failing patients.
In Dallas, Jorge Mendez, 50, an automotive shop foreman, was in need of a life-saving transplant.
BLOOD TEST MAY PREDICT THE ORGANS IN THE BODY THAT ARE AGING FASTER THAN NORMAL, SAYS STANFORD STUDY
Mendez was on dialysis — which has a significant impact on not only a person’s quality of life on a daily basis, but also long-term health.
It was important for him to find a transplant before he became too sick for the procedure, according to his doctor.
Rebecca Warden, second from left, volunteered to give a kidney to her mother, 71-year-old Ann Winer of San Antonio, far left. And Svetlana Balmeo Stockdale, 28 (far right), volunteered to give a kidney to her co-worker, Jorge Mendez, 50, standing beside her. (University Health/UT Southwestern)
Mendez’s coworker, Svetlana Balmeo Stockdale, 28, offered to donate a kidney to her friend — but unfortunately she was not a match.
Meanwhile, 250 miles away in San Antonio, 71-year-old Ann Winer was also in dire need of a kidney transplant.
She was on dialysis after waiting almost two years for a kidney donor.
Winer’s biggest obstacle was that she had unusual antibodies that made it very difficult for her to match with a donor, her doctors said.
“A patient’s access to a lifesaving transplant shouldn’t be limited by geographic or organizational boundaries.”
Winer’s daughter, Rebecca Warden, wanted to donate a kidney — but it was not a compatible match.
“Winer would likely have become weaker over time and her condition would have grown worse,” Parsia Vagefi, M.D., the transplant surgeon at UT Southwestern who led the surgical team in Dallas, told Fox News Digital.
“She said she had almost given up hope of receiving a transplant.”

Rebecca Warden, left, volunteered to give a kidney to her mother, 71-year-old Ann Winer of San Antonio, right. Warden was not a match, though, so Winer’s medical team in San Antonio collaborated with another team in Dallas to find a donor swap for their respective patients. (University Health)
The leaders at both institutions began working together to find matches outside their local transplant networks.
After learning that she wasn’t a match for her friend, Stockdale — the intended donor for Mendez — got a surprising phone call.
ONE FAMILY DONATES FOUR KIDNEYS TO SAVE A NEW YORK MAN’S LIFE: ‘DEFIED ALL ODDS’
“A little while after I was told my kidney wasn’t a match, UT Southwestern called me and they said, ‘You couldn’t donate to Jorge, but we could do a swap with somebody else,’” she said in a statement to Fox News Digital.
As it turned out, Stockdale was a match for Winer, the grandmother in San Diego — and Warden, who had intended to donate to her mother, was a match for Mendez.
Setting the stunning plan into motion
The medical teams in Dallas and San Antonio began plans for a donor swap for their respective patients.
“[After finding the matches], we began discussing, ‘When would we start the surgeries? How would we transport the organs? How would the organs be tracked?’” said Dr. Elizabeth Thomas, transplant surgeon with University Health who led the transplant team in San Antonio, in a comment sent to Fox News Digital.

Jorge Mendez, 50, left, received a replacement for his failing kidney after medical teams in San Antonio and Dallas searched beyond their own networks for compatible living donors for their patients. Shown at right with him and wearing a matching yellow gown, Svetlana Balmeo Stockdale, 28, walks with Mendez after the two underwent surgery at UT Southwestern in Dallas. (UT Southwestern)
Through “carefully choreographed surgical schedules and chartered flights,” the transplant teams ensured that the donated organs would be safely transported and transplanted as quickly as possible, according to a statement from the hospitals.
“[The transport] could be tracked minute by minute in the plane via a tag that was on the box that was used to transport [the kidneys],” Thomas said.
ARKANSAS MILITARY VETERAN RECEIVES WORLD’S FIRST WHOLE-EYE AND PARTIAL-FACE TRANSPLANT
“It is important because we want to keep the time that the organ is out of the body without blood to a minimum.”
On Aug. 31, 2023, after a day of “superbly timed surgeries and close coordination,” according to the hospitals, Winer and Mendez received the new, functioning kidneys they needed to save their lives.

On Aug. 31, 2023, after a day of “superbly timed surgeries and close coordination,” according to the hospitals, Winer and Mendez received the new, functioning kidneys they needed to save their lives. (UT Southwestern/University Health)
“There are various ways you can do the swaps and various reasons to do them … It never gets old,” Dr. Vagefi told Fox News Digital.
Only a quarter of the transplants performed at UT Southwestern are from living donors, but Vagefi said he is hoping to expand that number, as living kidney donations last longer for the recipients.
“It’s really great to participate in it and form a collaboration with others who are working toward the same mission but in a different city,” he said. “We crossed geographic boundaries to help these families.”
Grateful for new hope
Because of the life-saving transplant, Mendez was able to hold his new granddaughter when the baby was born in January.
“It brought tears to my eyes to hold her,” he said in a statement. “Now I can live a little bit longer to spend time with her.”
He later wrote to his donor: “Thank you very much. I owe you the world.”
“I don’t think of it as me saving somebody’s life — I think of it as me giving Jorge’s family members more time with him.”
“I felt like they’d never find a donor for me, but they did,” Winer said.
On a card she sent to her Dallas donor, she wrote: “I will never be able to repay you.”
Stockdale, who had intended to donate to her friend Mendez, shared what being a donor means to her in a statement to Fox News Digital.
PIG HEART RECIPIENT’S ‘LAST WISH’ WAS TO HELP DOCTORS LEARN FROM PROCEDURE, DYING MAN SAID: ‘WE WILL MISS HIM’
“I don’t think of it as me saving somebody’s life,” she said. “I think of it as me giving Jorge’s family members more time with him.”
“[For Winer], whatever she hasn’t accomplished in life yet that she ultimately wanted to do, I hope she gets to do it. Life’s too short to not live out your wildest dreams.”
Winer, the retired nurse anesthesiologist, later wrote a letter to Stockdale thanking her for the kidney.
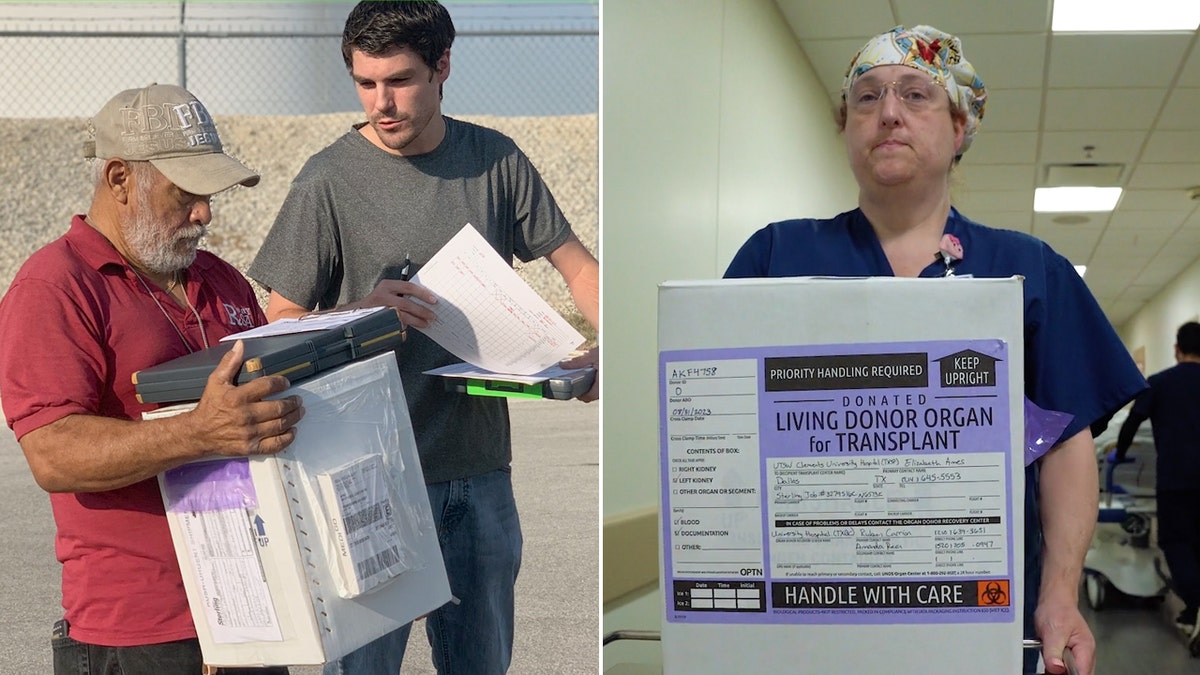
Through “carefully choreographed surgical schedules and chartered flights,” the transplant teams ensured that the donated organs would be safely transported and transplanted as quickly as possible, according to the hospitals. (UT Southwestern/University Health)
“Thank you for giving me back my life,” she wrote.
“I thought I would never get a transplant with my weird antibodies, and then you came along. Bless you.”
Warden — Winer’s daughter who had intended to donate to her mother but agreed to donate to Mendez in exchange for her mother receiving a transplant — also expressed her gratitude.

Parsia Vagefi, M.D., is the transplant surgeon at UT Southwestern who led the surgical team in Dallas. (UT Southwestern)
“At the end of the day, I’m happy that I’ve been able to help two people and not just one,” she said in a statement.
Today, both transplant recipients are doing well.
Winer is back at work part-time as a nurse anesthesiologist and is planning to retire at the end of July.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Mendez has also returned to work. “I feel great,” he said.
Scott Bennett, associate vice president of the Solid Organ Transplant Program at UT Southwestern, said in a press release that “a patient’s access to a lifesaving transplant shouldn’t be limited by geographic or organizational boundaries.”

Dr. Parsia Vagefi of UT Southwestern led the surgical team in Dallas that collaborated with University Health in San Antonio to save two patients with failing kidneys. (UT Southwestern)
“It was rewarding to see the collective can-do spirit of two highly regarded programs collaborate to make it happen,” he added.
A kidney is the organ in the greatest demand for transplant.
A healthy person can live a full life after donating one of their two kidneys, according to experts.
The average life expectancy for someone on dialysis is five to 10 years, according to the National Kidney Foundation.
For more Health articles, visit www.foxnews.com/health.

Health
'Unsung Hero' Movie Tells the Inspiring True Story of the Smallbone Family — Rebecca St. James and for King + Country’s Joel and Luke

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Amid bird flu spread, experts reveal if it's safe to drink milk: 'Indirect concern'

CDC issues alert over bird flu case
Fox News medical contributor Dr. Marc Siegel on what to know about bird flu and why it is important to not look directly at the solar eclipse without proper glasses
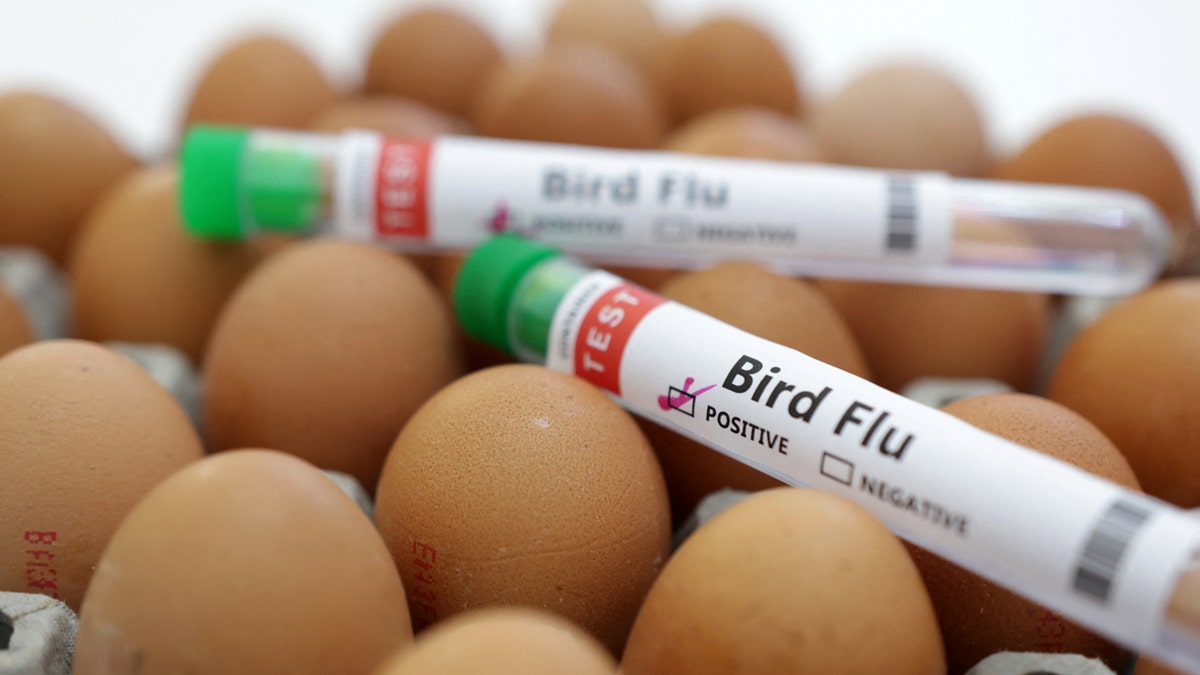
Traces of bird flu have been detected in pasteurized milk — leaving many people wondering if it’s safe to drink.
The U.S. Food and Drug Administration (FDA) released a notice on Thursday stating that one in five retail samples of commercial milk tested positive for fragments of highly pathogenic avian influenza (HPAI), more commonly known as bird flu or avian flu.
The share of milk with viral remnants was higher in areas where herds of cattle had been infected.
BIRD FLU PANDEMIC IN FUTURE? EU WARNS OF POTENTIAL SPREAD TO HUMANS DUE TO ‘LACK OF IMMUNE DEFENSE’
The presence of the virus in the milk doesn’t necessarily mean there is a risk to consumers, however, the FDA noted.
“Additional testing is required to determine whether an intact pathogen is still present and if it remains infectious, which would help inform a determination of whether there is any risk of illness associated with consuming the product,” the agency stated.
Traces of bird flu have been detected in pasteurized milk, leaving many people wondering if it’s safe to drink. (iStock)
“Although bird flu viruses do not normally infect humans, sporadic human infections have occurred,” the FDA stated in the alert.
Pasteurization eliminates risk, experts say
Before milk can be sold commercially, government regulations require that it is pasteurized.
During the pasteurization process, raw milk is heated to a certain temperature for a brief period of time and is then chilled again, according to the International Dairy Foods Association (IDFA) website.
This process kills any pathogens and ensures that milk is safe to drink.
BIRD FLU VIRUS FOUND IN GROCERY STORE MILK, BUT NO RISK TO CUSTOMERS, FDA SAYS
Dr. Scott Pegan, professor of biomedical sciences at the University of California, Riverside and a biochemist for the United States Medical Research Institute of Chemical Defense, said the FDA’s finding does not mean there is any direct risks to consumers.
“In the U.S., commercial intrastate sold milk is required to be pasteurized,” he told Fox News Digital. “This process is geared to kill viruses like H5N1 and other bacteria that can pose a threat to human health.”

A milk pasteurization system is shown at a food and drink exhibition. Pasteurization is a process that kills microbes in food and drink, such as milk, juice, canned food and others. (iStock)
“Milk that has been pasteurized is safe and there is no current reason to avoid it or other pasteurized milk products based on the FDA’s findings,” Pegan went on.
“However, there is a substantial risk of consuming unpasteurized milk and products of that milk.”
Even after viruses and bacteria have been killed in pasteurized milk, remnants can remain in the milk, he said — but they are not dangerous.
RARE HUMAN CASE OF HIGHLY CONTAGIOUS BIRD FLU CONFIRMED IN TEXAS
Edward Liu, M.D., chief of infectious diseases at Hackensack Meridian Jersey Shore University Medical Center in New Jersey, agreed that there is not a risk associated with drinking pasteurized milk.
“The pasteurization is the key — the heat treatment kills off the viruses,” he told Fox News Digital. “Although the FDA’s testing picked up fragments [of the virus], the heating process destroyed it, so it’s not able to infect people.”

The share of milk with viral remnants was higher in areas where herds of cattle had been infected. (iStock)
The fragments alone are not enough to cause any kind of infection, he confirmed.
“I think the key word is ‘fragments.’ Just like with COVID, if you do a PCR test a month later, we’ll detect little fragments of the virus, but it’s not active anymore,” Liu said.
“So if the virus isn’t entirely intact, it shouldn’t be able to infect you.”
Any sporadic cases of human infection would likely occur when a farmer is handling birds directly, Liu said.
Consumers should avoid drinking raw milk that has not been pasteurized, the FDA said.
“There are some people who like to go all natural, but pasteurization has been used for decades for safety,” he said. “Some degree of processing is actually better and safer for us.”
Animals pose greater concern, experts say
The “indirect concern” within the scientific and medical community involves the increased risk of “spillover” to humans from animals with the H5N1 virus, said Pegan.
“Prior to the outbreak in dairy cattle, this concern principally revolved around the risk of transmission to humans from wild birds or poultry,” he told Fox News Digital.
The “indirect concern” within the scientific and medical community involves the increased risk of “spillover” to humans from animals with the H5N1 virus, one expert said. (REUTERS/Dado Ruvic/Illustration/File Photo)
“The presence of H5N1 avian flu in the milk of these cattle shows that cattle may be able to provide a new reservoir for this virus, increasing the odds of exposure to those in direct contact with the infected cattle.”
The more animals that are infected, the higher chance that humans may come in direct contact with the virus — which likely would lead to a greater number of human cases, said Pegan.
SOCIAL MEDIA USERS UPSET AS SHETLAND PONY IS STUCK IN CATTLE GRID FOR 4 HOURS WITH CREWS TOILING TO FREE HIM
“The case of cattle-to-human transmission seen in Texas is in line with this concern,” he noted.
“Also, the more mammals infected increases the chances that the virus will adapt to other mammals, such as humans.”
FDA’s recommendations
The FDA restated its “long-standing recommendation” that consumers avoid drinking raw milk that has not been pasteurized.
The agency also recommends that companies refrain from manufacturing or selling raw milk or raw milk products made with milk from cows that tested positive for bird flu, were exposed to the virus or showed symptoms of illness.
“Over the past few years, there has been an increased consumer demand for these unpasteurized products,” Pegan said.

The FDA restated its “long-standing recommendation” that consumers avoid drinking raw milk that has not been pasteurized. (iStock)
“While not allowed to be sold via interstate brands, some states have relaxed local sales of these products at farmer’s markets and similar outlets,” he said.
“Individuals may want to avoid those unpasteurized products until more information is obtained about this H5N1 avian flu outbreak in dairy cattle.”
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The FDA also urged producers to “take precautions” when discarding milk from affected cows, “so that the discarded milk does not become a source of further spread.”
So far, only one person has been confirmed to have contracted the virus after exposure to infected cows, the FDA stated.
“The CDC says the risk to the general public remains low,” the agency said.
“The FDA and USDA continue to indicate that, based on the information we currently have, our commercial milk supply is safe.”
Fox News Digital reached out to the National Milk Producers Federation, the American Dairy Association and the International Dairy Foods Association for comment.
For more Health articles, visit www.foxnews.com/health.
Health
New Jersey woman recovering after receiving successful pig kidney transplant

- Lisa Pisano faced heart and kidney failure, rendering her ineligible for traditional transplants, but a pioneering procedure at NYU Langone Health offered hope.
- Doctors implanted a mechanical heart pump to stabilize Pisano’s failing heart, followed by a kidney transplant from a genetically modified pig.
- Pisano’s recovery is progressing well, marking a significant advancement in animal-to-human transplantation.
Doctors have transplanted a pig kidney into a New Jersey woman who was near death, part of a dramatic pair of surgeries that also stabilized her failing heart.
Lisa Pisano’s combination of heart and kidney failure left her too sick to qualify for a traditional transplant, and out of options. Then doctors at NYU Langone Health devised a novel one-two punch: Implant a mechanical pump to keep her heart beating and days later transplant a kidney from a genetically modified pig.
Pisano is recovering well, the NYU team announced Wednesday. She’s only the second patient ever to receive a pig kidney — following a landmark transplant last month at Massachusetts General Hospital – and the latest in a string of attempts to make animal-to-human transplantation a reality.
MASSACHUSETTS MAN, RECIPIENT OF FIRST SUCCESSFUL PIG KIDNEY TRANSPLANT, IS DISCHARGED FROM HOSPITAL
This week, the 54-year-old grasped a walker and took her first few steps.
Lisa Pisano looks at photos of her dog after her surgeries at NYU Langone Health in New York on April 22, 2024. Doctors transplanted a pig kidney into Pisano, who was near death, part of a dramatic pair of surgeries that also included a fix for her failing heart. (AP Photo/Shelby Lum)
“I was at the end of my rope,” Pisano told The Associated Press. “I just took a chance. And you know, worst case scenario, if it didn’t work for me, it might have worked for someone else and it could have helped the next person.”
Dr. Robert Montgomery, director of NYU Langone Transplant Institute, recounted cheers in the operating room as the organ immediately started making urine.
“It’s been transformative,” Montgomery said of the experiment’s early results.
But “we’re not off the hook yet,” cautioned Dr. Nader Moazami, the NYU cardiac surgeon who implanted the heart pump.
“With this surgery I get to see my wife smile again,” Pisano’s husband Todd said Wednesday.
FEDS INVESTIGATE TEXAS SURGEON ACCUSED OF DENYING PATIENTS LIFE-SAVING LIVER TRANSPLANTS
Other transplant experts are closely watching how the patient fares.
“I have to congratulate them,” said Dr. Tatsuo Kawai of Mass General, who noted that his own pig kidney patient was healthier overall going into his operation than NYU’s patient. “When the heart function is bad, it’s really difficult to do a kidney transplant.”
THE PIG ORGAN QUEST
More than 100,000 people are on the U.S. transplant waiting list, most who need a kidney, and thousands die waiting. In hopes of filling the shortage of donated organs, several biotech companies are genetically modifying pigs so their organs are more humanlike, less likely to be destroyed by people’s immune system.
NYU and other research teams have temporarily transplanted pig kidneys and hearts into brain-dead bodies, with promising results. Then the University of Maryland transplanted pig hearts into two men who were out of other options, and both died within months.
Mass General’s pig kidney transplant last month raised new hopes. Kawai said Richard “Rick” Slayman experienced an early rejection scare but bounced back enough to go home earlier this month and still is faring well five weeks post-transplant. A recent biopsy showed no further problems.
A COMPLEX CASE AT NYU
Pisano is the first woman to receive a pig organ — and unlike with prior xenotransplant experiments, both her heart and kidneys had failed. She went into cardiac arrest and had to be resuscitated before the experimental surgeries. She’d gotten too weak to even play with her grandchildren. “I was miserable,” the Cookstown, New Jersey, woman said.
A failed heart made her ineligible for a traditional kidney transplant. But while on dialysis, she didn’t qualify for a heart pump, called a left ventricular assist device or LVAD, either.
“It’s like being in a maze and you can’t find a way out,” Montgomery explained — until the surgeons decided to pair a heart pump with a pig kidney.
TWO SURGERIES IN EIGHT DAYS
With emergency permission from the Food and Drug Administration, Montgomery chose an organ from a pig genetically engineered by United Therapeutics Corp. so its cells don’t produce a particular sugar that’s foreign to the human body and triggers immediate organ rejection.
Plus a tweak: The donor pig’s thymus gland, which trains the immune system, was attached to the donated kidney in hopes that it would help Pisano’s body tolerate the new organ.
Surgeons implanted the LVAD to power Pisano’s heart on April 4, and transplanted the pig kidney on April 12. There’s no way to predict her long-term outcome but she’s shown no sign of organ rejection so far, Montgomery said. And in adjusting the LVAD to work with her new kidney, Moazami said doctors already have learned lessons that could help future care of heart-and-kidney patients.
Special “compassionate use” experiments teach doctors a lot but it will take rigorous studies to prove if xenotransplants really work. What happens with Pisano and Mass General’s kidney recipient will undoubtedly influence FDA’s decision to allow such trials. United Therapeutics said it hopes to begin one next year.
-
 Movie Reviews1 week ago
Movie Reviews1 week agoMovie Review: The American Society of Magical Negroes
-

 World1 week ago
World1 week agoIf not Ursula, then who? Seven in the wings for Commission top job
-
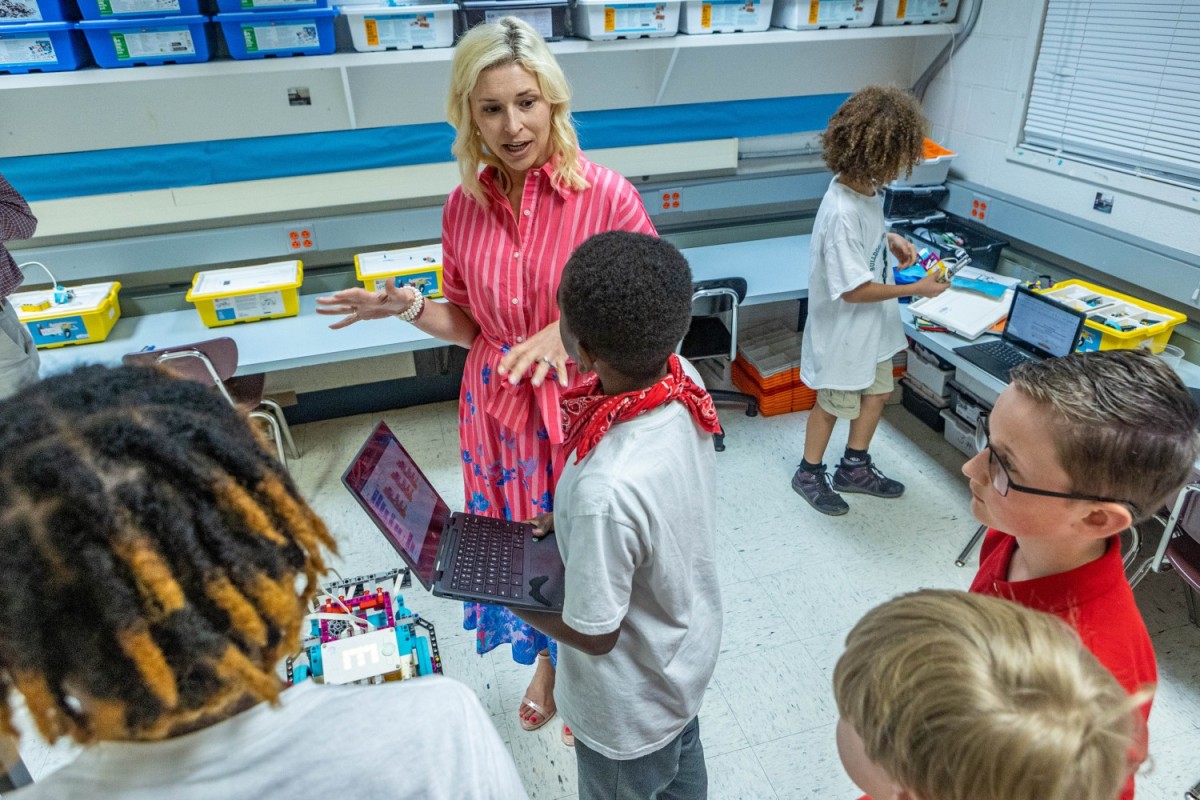
 Kentucky1 week ago
Kentucky1 week agoKentucky first lady visits Fort Knox schools in honor of Month of the Military Child
-

 World1 week ago
World1 week ago'You are a criminal!' Heckler blasts von der Leyen's stance on Israel
-

 Politics1 week ago
Politics1 week agoTrump trial: Jury selection to resume in New York City for 3rd day in former president's trial
-

 News1 week ago
News1 week agoHouse passes bill requiring warrant to purchase data from third parties
-

 World1 week ago
World1 week agoColumbia University leaders face scrutiny over anti-Semitism on campus
-

 Politics1 week ago
Politics1 week agoFormer Wisconsin Democratic Rep. Peter Barca launches congressional comeback bid