Science
How L.A. County is trying to remake addiction treatment — no more 'business as usual'

Gary Horejsi wrestled with the decision before him, knowing a life could be in his hands.
It was the third time that the woman had used drugs or alcohol since coming to CRI-Help, which runs a 135-bed residential facility in North Hollywood where people are treated for substance use disorder.
CRI-Help needed to be a safe place for people grappling with their addictions. In the past, others had been removed for less. Horejsi, the clinical director, had the final say on whether she should be discharged.
He perused her file on his computer. The woman was still trying, CRI-Help staffers told him. She hadn’t shared drugs with anyone. And if she were to leave, the risks of an overdose were graver than before.
Horejsi decided to let her stay.
“Things can’t be business as usual anymore,” their chief executive, Brandon Fernandez, later said at a CRI-Help staff meeting. If someone leaves treatment and resumes using drugs the same way they were before, “that could very well look like them dying.”
“So are we going to be willing to do something different?”
“Things can’t be business as usual anymore,” CRI-Help Chief Executive Brandon Fernandez told his staff at a meeting in North Hollywood on April 10.
(Myung J. Chun / Los Angeles Times)
Fernandez had gathered CRI-Help staff in their North Hollywood conference room to talk about a Los Angeles County initiative that could reshape such decisions. It’s called Reaching the 95% — or R95 — and its goal is to engage with more people than the fraction of Angelenos already getting addiction treatment.
Across the country, more than 48 million people had a drug or alcohol use disorder, according to the latest results from the National Survey on Drug Use and Health. Only 13 million received treatment in the previous year. Among those who did not get treatment, roughly 95% said they did not think that they should.
Those numbers have collided with the grim toll of fentanyl, an especially potent opioid that has driven up deaths across the country. In Los Angeles County, the number of overdose deaths tied to fentanyl skyrocketed between 2016 and 2022, soaring from 109 to 1,910, according to a county report.
“We can’t just take the approach that we’ve been taking and kind of assume that everyone wants the services that we offer,” said Dr. Gary Tsai, director of the Substance Abuse Prevention and Control division at the L.A. County Department of Public Health. “That’s just not the reality.”
His department is trying to nudge addiction treatment facilities to change their approach, by offering financial incentives for those that meet R95 requirements. Among them: changing their rules to not automatically eject people who have a “lapse” of drug use.
Fernandez, whose organization is participating in R95, said abstinence is still its aspirational goal — and “we still have the ability to use our own clinical judgment on a case-by-case basis,” such as if people endanger other participants. But “we shouldn’t have blanket policies.”
To get R95 funding, they also cannot require people to be totally abstinent before being admitted. And under R95, treatment programs are also being encouraged to partner with syringe programs rooted in “harm reduction” — a philosophy focused on minimizing the harmful effects of drug use — to address the needs of people who may not want to enter or remain in treatment.
Some treatment providers “view us as the enemy instead of as allies,” said Soma Snakeoil, executive director of the Sidewalk Project, which provides Narcan spray to reverse overdoses and other services on L.A.’s Skid Row.
With R95, she said, “the biggest change is that harm reduction organizations and treatment providers are talking to each other in a way that was not happening before.”

Soma Snakeoil, executive director of the Sidewalk Project, gives first aid to a woman with an open wound on her foot last year in Los Angeles.
(Francine Orr / Los Angeles Times)
The county is also prodding addiction treatment facilities to reexamine whether the way they operate could be turning people away, and look more closely at the “customer experience.” Tsai compared the situation to a restaurant drawing few customers: “How do we get more people in the door?”
Too often, “the drug dealers do a much better job of delivering their product to our patients than we do,” said Dr. Randolph Holmes, chair of government affairs for the California Society of Addiction Medicine.
When Johnny Guerrero decided to get off Skid Row and go into residential treatment in Los Angeles, he was initially turned away because he had arrived “late — maybe 10 minutes late,” the 35-year-old said.
He was only able to get in, he said, because the harm reduction worker who had taken him to the facility let him stay the night at her home, then brought him back the next morning. Even then, “there was so much paperwork. I was so dopesick. There was just hurdle after hurdle after hurdle.”
“They did not make it easy for an addict to get help,” Guerrero said.
In many cases, “the biggest barrier is just being able to get somebody on the phone” with a treatment provider, said Amanda Cowan, executive director of Community Health Project LA, which provides clean syringes and other services to people who use drugs. “When people are ready, they are ready in that moment.”
As of late March, roughly half of the addiction treatment providers that contract with L.A. County were on track to become “R95 Champions,” which could yield hundreds of thousands of dollars each in additional funding.

CRI-Help’s George T. Pfleger center in North Hollywood.
(Myung J. Chun / Los Angeles Times)
To get those funds, they must turn in admissions and discharge policies that adhere to the R95 guidelines, as well as an “engagement policy.” They are also supposed to meet R95 requirements in one other area of their choice, which could include a “customer walkthrough” to see what might turn away clients.
CRI-Help, for instance, had decided to change how it asks newcomers to undergo a search. “The last thing we want to do is trigger someone’s trauma history and potentially have them walk out the door,” Fernandez said.
To ensure it was consistently done with sensitivity, CRI-Help drew up a script for staffers, emphasizing that consenting to a search would help maintain a safe facility. The hope is that “they feel they’re doing something as a part of a community — versus being forced to undergo something that’s uncomfortable.”
Staffers also tell them that if they have any drugs to hand over, “there’s not going to be any consequence, you can still come into treatment,” Fernandez said. “And if we find them on you, there still won’t be any negative consequences.”
The L.A. County push comes as state and federal officials have stressed the need for “low barrier” approaches to addiction care. Even cutting back on drug use can have positive results, researchers have found.
But some of the changes can be at odds with long-standing beliefs among treatment providers, many of whom got into the field after successfully battling their own addictions in programs firmly focused on abstinence.
Many in the field think “this is what works” because it did work for them, said Vitka Eisen, chief executive of HealthRight 360, another R95 participant. But “we’re the survivors, and we don’t talk to those who didn’t survive.”
Addiction researchers have long called to reexamine how people are treated for substance use disorders. More than a decade ago, a Columbia University center found that “much of what passes for ‘treatment’ of addiction bears little resemblance to the treatment of other health conditions.”
“This is inexcusable given decades of accumulated scientific evidence attesting to the fact that addiction is a brain disease,” the National Center on Addiction and Substance Abuse lamented in its report.
Experts argue that part of the problem is that addiction treatment has long been separated from the rest of the healthcare system. Richard Rawson, senior advisor to UCLA Integrated Substance Abuse Programs, said a major shift was the emergence of buprenorphine, a medication for opioid addiction that could be prescribed in ordinary clinics just like medicines for other chronic conditions.
But some Southern California treatment providers have viewed using buprenorphine and other such medications as short of sobriety, UC San Diego researchers found — even as California has ushered in requirements for licensed treatment facilities to either offer or help people access such medications.
Addiction is now much more widely understood as a medical condition, but “how much of that philosophy actually gets down to the level of the counselor?” Rawson said. “I think that’s still a work in progress.”
Tsai said a challenge in rolling out R95 is the ingrained idea that “you’re ready or not” for substance use treatment. But “we don’t actually treat any other health condition that way,” he said. “You don’t tell someone with diabetes, ‘Your blood sugar has to be completely under control, and then you’ll be ready for treatment.’”
In North Hollywood, counselors and other CRI-Help employees seated around the conference table studied the R95 goals printed on an L.A. County handout. One staffer said she was struggling with a specific statement, particularly for people in a residential setting: “Requiring abstinence is too high of a bar” for treatment.
Fernandez decided to share his own story. More than a decade ago, he was struggling with drug use, which had worsened after the death of his father. He was unemployed and didn’t have a stable place to live. When an outpatient counselor suggested residential treatment, he initially brushed off the suggestion.

CRI-Help’s staffers had questions and concerns about the changing approach to addiction treatment but ultimately seemed supportive.
(Myung J. Chun / Los Angeles Times)
He changed his mind after a “tough weekend,” but had no intention of abstaining from all drugs in the long term. Fernandez said he was nonetheless welcomed at CRI-Help: “Let’s just help you out for now.”
“I came here begrudgingly with a total attitude that I was going to continue smoking weed when I left treatment. I definitely wasn’t going to stop drinking,” even as he recognized that other things he was doing might be a problem, Fernandez told the CRI-Help employees.
Among those who had gone to treatment, he asked the group, “were you ready for total abstinence on Day One?”
“No. That wasn’t even my plan,” the same staffer replied with a rueful laugh.
Still, she and others were anxious about how they would keep everyone safe if clients used drugs, especially if they tried to bring them into the facility. “That worries me a little bit,” she said.
“It worries me too,” Fernandez said.
What preoccupies CRI-Help staff is how to balance the needs of people who have had a “lapse” into drug use with maintaining a safe environment for other clients grappling with addiction.
Horejsi said in an interview that whenever someone uses — even if they don’t share their drugs — “everyone knows, and that in itself does have an effect on people. Sometimes people will feel less safe.”
But Horejsi stressed to the group that “we’re already not discharging people for using” alone.
When people have relapsed, the North Hollywood center has monitored them one-on-one in its television room until staff are sure they are safe, then decided on their next steps. Some have ultimately been moved to another CRI-Help residential facility to continue getting treatment and have a “fresh start,” he said.
The clinical director also urged his co-workers to look back at the many changes CRI-Help had already undergone, such as starting to offer medication for addiction treatment. He reminded them that years ago, CRI-Help clients could be discharged if a doctor had given them an opioid pill at the hospital.

Mary Grayson, a longtime staff member at CRI-Help, spoke positively of the organizations changes over the years.
(Myung J. Chun / Los Angeles Times)
“What about when we discharged people because they talked about getting — they glorified drugs?” said Mary Grayson, a longtime CRI-Help employee.
Leaning forward in her seat, Grayson reminded her co-workers that “CRI-Help is not what it was when I walked through those doors 25 years ago — thank God!”
It started with “two shacks on this property. Two raggedy shacks. And look at where we are now,” she said. “Without us changing and growing, we won’t be able to be who we are.”

Science
Q&A: Learn how Olympians keep their cool from Team USA's chief sports psychologist

Your morning jog or weekly basketball game may not take place on an Olympic stage, but you can use Team USA’s techniques to get the most out of your exercise routine.
It’s not all about strength and speed. Mental fitness can be just as important as physical fitness.
That’s why the U.S. Olympic & Paralympic Committee created a psychological services squad to support the mental health and mental performance of athletes representing the Stars and Stripes.
“I think happy, healthy athletes are going to perform at their best, so that’s what we’re striving for,” said Jessica Bartley, senior director of the 15-member unit.
Bartley studied sports psychology and mental health after an injury ended her soccer career. She joined the USOPC in 2020 and is now in Paris with Team USA’s 592 competitors, who range in age from 16 to 59.
Bartley spoke with The Times about how her crew keeps Olympic athletes in top psychological shape, and what the rest of us can learn from them. Her comments have been edited for length and clarity.
Why is exercise good for mental health?
It gets you moving. It gets the endorphins going. And there’s often a lot of social aspects that are really helpful.
There are a number of sports that stretch your brain in ways that can be really, really valuable. You’re thinking about hand-eye coordination, or you’re thinking about strategy. It can improve memory, concentration, even critical thinking.
What’s the best way to get in the zone when it’s time to compete?
When I work with athletes, I like to understand what their zone is. If a 0 or a 1 is you’re totally chilled out and a 10 is you’re jumping around, where do you need to be? What’s your number?
People will say, “I’m at a 10 and I need to be at an 8 or a 7.” So we’ll talk about ways of bringing it down, whether it’s taking a deep breath, listening to relaxing music, or talking to your coach. Or there’s times when people say they need to be more amped up. That’s when you see somebody hitting their chest, or jumping up and down.
If you make a mistake in the middle of a competition, how do you move on instead of dwelling on it?
I often teach athletes a reset routine. I played goalie, so I had a lot of time to think after getting scored on. I would undo my goalie gloves and put them back on, which to me was a reset. I would also wear an extra hairband on my wrist, and when I would snap it, that meant I needed to get out of my head.
It’s not just a physical reset — it helps with a mental reset. If you do the same thing every single time, it goes through the same neural pathway to where it’s going to reset the brain. That can be really impactful.
Do Olympic athletes have to deal with burnout?
Oh, yeah. Everybody has a day where they don’t want to do whatever it is. That’s when you have to ask, “What’s in my best interests? Do I need a recovery day, or do I really need to get in the pool, or get in the gym?”
Sometimes you really do need what we like to refer to as a mental health day.
How can you psych yourself up for a workout when you just aren’t feeling it?
It’s really helpful to think about why you’re doing this and why you’re pushing yourself. Do you have goals related to an activity or sport? Is there something tied to values around hard work or discipline, loyalty or dependability?
When you don’t want to get in the gym, when you don’t want to go for a run, think about something bigger. Tie it back to values.
Is sleep important for maintaining mental health?
Yes! We started doing mental health screens with athletes before the Tokyo Games. We asked about depression, anxiety, disordered eating and body image, drugs and alcohol, and sleep. Sleep was actually our No. 1 issue. It’s been a huge initiative for us.
How much sleep should we be getting?
It’s different for everyone, but generally we know seven to nine hours of sleep is good. Sometimes some of these athletes need 10 hours.
I highly recommend as much sleep as you need. If you didn’t get enough sleep, napping can be really valuable.
Is napping just for Olympic athletes or is it good for everybody?
Everybody! Naps are amazing.
What if there’s no time for a nap?
There are different ways of recharging. Naps could be one of them, but maybe you just need to get off your feet for 20 minutes. Maybe you need to do a meditation or mindfulness exercise and just close your eyes for five minutes.
How do you minimize the effects of jet lag?
We try to shift one hour per day. That’s the standard way of doing it. If you can, it’s super helpful. But it’s not always possible.
The thing we tell athletes is that our bodies are incredible, and you will even things out if you can get back on schedule. One or two nights of crummy sleep is not going to impact your overall performance.
What advice do you give athletes who have trouble falling asleep the night before a competition?
You don’t want to change much right before a competition, so I usually direct athletes to do what they would normally do.
Do you need to unwind by reading a book? Do you need to talk on the phone with somebody and get your mind off things? Can you put your mind in a really restful place and think about things that are really relaxing?
Are there any mindfulness or meditation exercises that you find helpful?
There are some athletes who benefit greatly from an hourlong meditation. I love something quick, something to reset my brain, maybe close my eyes for a minute.
If I’m feeling like I need to take a moment, I love mindful eating. You savor a bite and go, “Oh, my gosh, I have not been fully engaged with my senses today.” Or you could take a mindful walk and take in the sights, the smells, all of the things that are around you.
What do you eat when you need a quick nutrition boost?
Cashews. I tend to carry those with me. They’ve got enough energy to make sure I keep going, physically.
I’ve always got gummy bears on me too. There’s no nutritional value but they keep me going mentally. I’m a big proponent of both.
Is it OK to be superstitious in sports?
It depends how flexible you are. Maybe you put on your socks or shoes a certain way, or listen to certain music. Routines are really soothing. They set your brain up for success in a particular performance. It can be really, really helpful.
But I’ve also seen an athlete forget their lucky underwear or their lucky socks, and they’re all out of sorts. So your routine has to be flexible enough that you’re not going to completely fall apart if you don’t do it exactly.
Are Olympians made of stronger psychological stuff than the rest of us?
Not necessarily. There are some who don’t get feathers ruffled and have a high tolerance for the fanfare. There’s also a lot of regular human beings who just happen to be fantastic at a particular activity.
Science
‘Ready, Steady, Slow’: Championship Snail Racing at 0.006 M.P.H.

Earlier this month, the rural village of Congham, England, played host to a less likely group of athletes: dozens of garden snails. They had gathered to compete in the World Snail Racing Championships, where the world record time for completing the 13.5 inch course stands at 2 minutes flat. At that speed — roughly 0.006 miles per hour — it would take the snails more than six days to travel a mile.
Science
Caring for condor triplets! Record 17 chicks thrive at L.A. Zoo under surrogacy method

A new method of rearing California condors at the Los Angeles Zoo has resulted in a record-breaking 17 chicks hatched this year, the zoo announced Wednesday.
All of the newborn birds will eventually be considered for release into the wild under the U.S. Fish and Wildlife Service’s California Condor Recovery Program, a zoo spokesperson said.
“What we are seeing now are the benefits of new breeding and rearing techniques developed and implemented by our team,” zoo bird curator Rose Legato said in a statement. “The result is more condor chicks in the program and ultimately more condors in the wild.”
Breeding pairs of California condors live at the zoo in structures the staff “affectionately calls condor-miniums,” spokesperson Carl Myers said. When a female produces a fertilized egg, the egg is moved to an incubator. As its hatching approaches, the egg is placed with a surrogate parent capable of rearing the chick.
California condor eggs are cared for at L.A. Zoo. The animal is critically endangered.
(Jamie Pham / L.A. Zoo)
This bumper year of condor babies is the result of a modification to a rearing technique pioneered at the L.A. Zoo.
Previously, when the zoo found itself with more fertilized eggs than surrogate adults available, staff raised the young birds by hand. But condors raised by human caretakers have a lower chance of survival in the wild (hence the condor puppets that zookeepers used in the 1980s to prevent young birds from imprinting on human caregivers).
In 2017, the L.A. Zoo experimented with giving an adult bird named Anyapa two eggs instead of one. The gamble was a success. Both birds were successfully released into the wild.
Faced with a large number of eggs this year, “the keepers thought, ‘Let’s try three,’” Myers said. “And it worked.”
The zoo’s condor mentors this season ultimately were able to rear three single chicks, eight chicks in double broods and six chicks in triple broods. The previous record number of 15 chicks was set in 1997.
Condor experts applauded the new strategy.
“Condors are social animals and we are learning more every year about their social dynamics. So I’m not surprised that these chick-rearing techniques are paying off,” said Jonathan C. Hall, a wildlife ecologist at Eastern Michigan University. “I would expect chicks raised this way to do well in the wild.”
The largest land bird in North America with an impressive wingspan up to 9½ feet, the California condor could once be found across the continent. Its numbers began to decline in the 19th century as human settlers with modern weapons moved into the birds’ territory. The scavenger species was both hunted by humans and inadvertently poisoned by lead bullet fragments embedded in carcasses it ate. The federal government listed the birds as an endangered species in 1967.
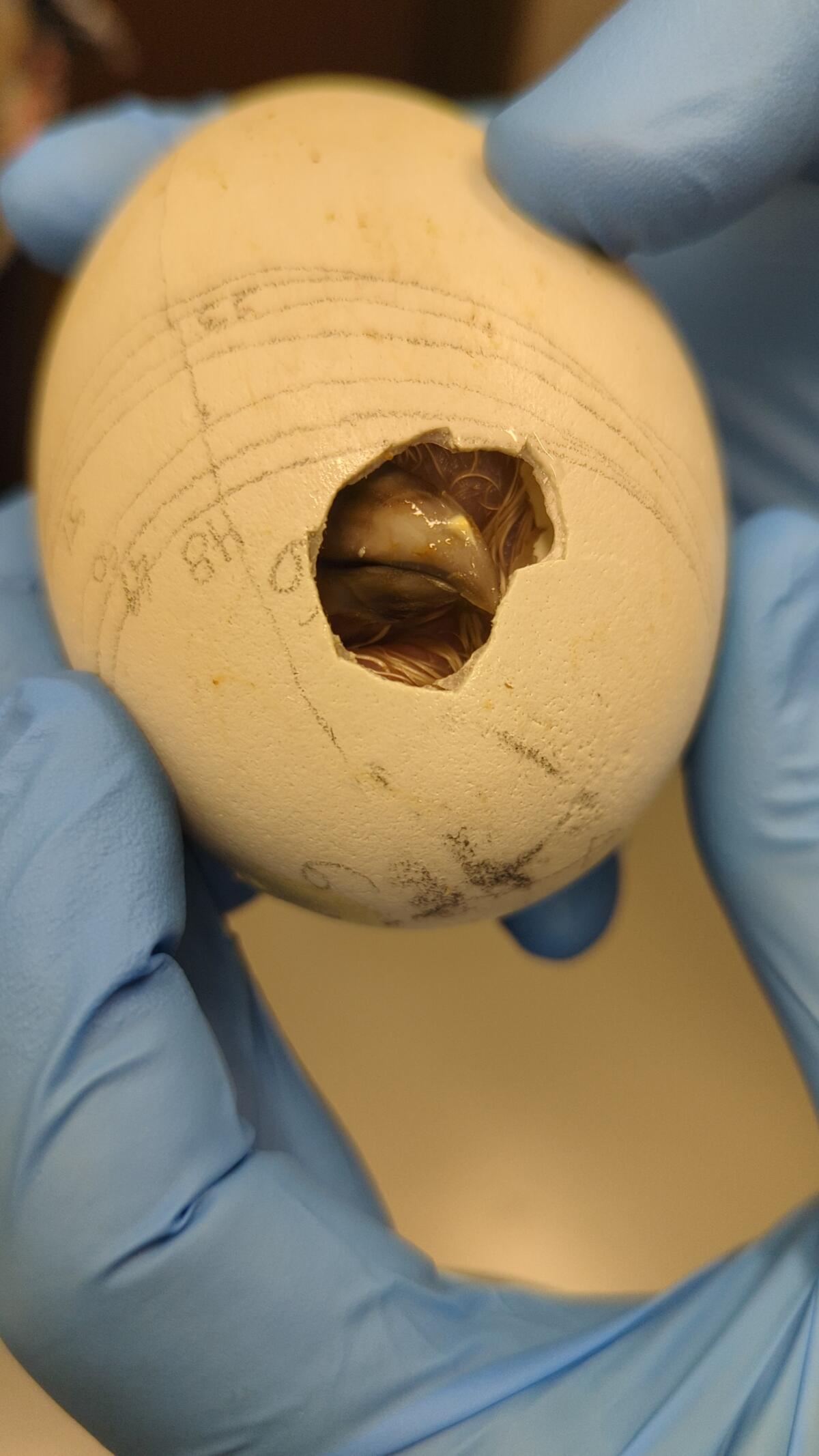
A condor, one of a record-breaking 17 at the zoo, makes its way out of its shell.
(Jamie Pham / L.A. Zoo)
When the California Condor Recovery Program began four decades ago, there were only 22 California condors left on Earth. As of December, there were 561 living individuals, with 344 of those in the wild. Despite the program’s success in raising the population’s numbers, the species remains critically endangered.
In addition to the ongoing threat of lead poisoning, the large birds are also at risk from other toxins. One 2022 study found more than 40 DDT-related compounds in the blood of wild California condors — chemicals that had made their way from contaminated marine life to the top of the food chain.
“Despite our success in returning condors to the wild, free-flying condors continue to face many obstacles with lead poisoning being the No. 1 cause of mortality,” said Joanna Gilkeson, spokesperson for Fish and Wildlife’s Pacific Southwest Region. “Innovative strategies, like those the L.A. Zoo is implementing, help us to produce more healthy chicks and continue releasing condors into the wild.”
The chicks will remain in the zoo’s care for the next year and a half before they are evaluated for potential release to the wild. Thus far, the zoo has contributed 250 condor chicks to Fish and Wildlife’s program, some of which the agency has redeployed to other zoos as part of its conservation efforts.
In a paper published earlier this year, a team of researchers found that birds born in captivity have slightly lower survival rates for their first year or two but then have equally successful outcomes to wild-hatched birds.
“Because condors reproduce slowly, releases of captive-bred birds are essential to the recovery of the species, especially in light of ongoing losses due to lead-related mortality,” said Victoria Bakker, a quantitative ecologist at Montana State University and lead author of the paper. “The team at the L.A. Zoo should be recognized for their innovative and important contributions to condor recovery.”
-

 World1 week ago
World1 week agoOne dead after car crashes into restaurant in Paris
-
 Midwest1 week ago
Midwest1 week agoMichigan rep posts video response to Stephen Colbert's joke about his RNC speech: 'Touché'
-

 News1 week ago
News1 week agoVideo: Young Republicans on Why Their Party Isn’t Reaching Gen Z (And What They Can Do About It)
-

 Movie Reviews1 week ago
Movie Reviews1 week agoMovie Review: A new generation drives into the storm in rousing ‘Twisters’
-

 News1 week ago
News1 week agoIn Milwaukee, Black Voters Struggle to Find a Home With Either Party
-
 Politics1 week ago
Politics1 week agoFox News Politics: The Call is Coming from Inside the House
-

 News1 week ago
News1 week agoVideo: J.D. Vance Accepts Vice-Presidential Nomination
-

 World1 week ago
World1 week agoTrump to take RNC stage for first speech since assassination attempt















