Science
The Ex-Patients’ Club

On a recent Friday morning, Daniel, a lawyer in his early 40s, was in a Zoom counseling session describing tapering off lithium. Earlier that week he had awakened with racing thoughts, so anxious that he could not read, and he counted the hours before sunrise.
At those moments, Daniel doubted his decision to wean off the cocktail of psychiatric medications which had been part of his life since his senior year in high school, when he was diagnosed with bipolar disorder.
Was this his body adjusting to the lower dosage? Was it a reaction to the taco seasoning he had eaten the night before? Or was it what his psychiatrist would have called it: a relapse?
“It still does go to the place of — what if the doctors are right?” said Daniel.
On his screen, Laura Delano nodded sympathetically.
Ms. Delano is not a doctor; her main qualification, she likes to say, is having been “a professional psychiatric patient between the ages of 13 and 27.” During those years, when she attended Harvard and was a nationally ranked squash player, she was prescribed 19 psychiatric medications, often in combinations of three or four at a time.
Then Ms. Delano decided to walk away from psychiatric care altogether, a journey she detailed in a new memoir, “Unshrunk: A Story of Psychiatric Treatment Resistance.” Fourteen years after taking her last psychotropic drug, Ms. Delano projects a radiant good health that also serves as her argument — living proof that, all along, her psychiatrists were wrong.
Since then, to the alarm of some physicians, an online DIY subculture focused on quitting psychiatric medications has expanded and begun to mature into a service industry.
Ms. Delano is a central figure in this shift. From her house outside Hartford, Conn., she offers coaching to paying clients like Daniel. But her ambitions are grander. Through Inner Compass Initiative, the nonprofit she runs with her husband, Cooper Davis, she hopes to provide support to a large swath of people interested in reducing or quitting psychiatric medications.
“People are realizing, ‘I don’t actually need to go find a doctor who knows how to do this,’” she said. In fact, she added, they may not even need to tell their doctor.
“That sounds quite radical,” she allowed. “I imagine a lot of people would hear that and be, like, ‘That’s dangerous.’ But it’s just been the reality for thousands and thousands of people out there who have realized, ‘I have to stop thinking that psychiatry is going to get me out of this situation.’”
Increasingly, many psychiatrists agree that the health care system needs to do a better job helping patients get off psychotropic medications when they are ineffective or no longer necessary. The portion of American adults taking them approached 25 percent during the pandemic, according to government data, more than triple what it was in the early 1990s.
But they also warn that quitting medications without clinical supervision can be dangerous. Severe withdrawal symptoms can occur, and so can a relapse, and it takes expertise to tease them apart. Psychosis and depression may flare up, and the risk of suicide rises. And for people with the most disabling mental illnesses, like schizophrenia, medication remains the only evidence-based treatment.
“What makes tremendous sense for Laura” and “millions of people who are over-diagnosed and over-treated makes no sense at all for people who can’t get medicine,” said Dr. Allen Frances, a professor emeritus of psychiatry at Duke University School of Medicine.
“Laura does not generalize to the person with chronic mental illness and has a clear chance of ending up homeless or in the hospital,” he said. “Those people don’t wind up looking like Laura when they are taken off medication.”
It was hard to say what a life after psychiatric treatment would look like for Daniel, who asked to be identified by only his first name to discuss his mental health history. He has been tapering off lithium for nine months under the care of a nurse-practitioner, and settled, for the moment, at 450 milligrams, half his original dose.
He had become convinced that the drugs were harming him. And yet, when the waves of anxiety and insomnia hit him, he wavered. Daniel is a litigator. He had depositions coming up at work, and the way his thoughts were jumping around scared him.
“I can’t avoid that fear, you know, ‘I’m doing a lot better on less lithium, but it’s just going to fall apart again,’ ” he told Ms. Delano.
Ms. Delano listened quietly, and then told him a story from her own life.
It happened a few months after she quit the last of her medications. On a night walk, her senses built to a crescendo. Christmas lights seemed to be winking messages at her. She recognized hypomania, a symptom of bipolar disorder, and the thought crossed her mind: The doctors had been right. Then some kind of force moved through her, and she realized that these sensations were not a sign of mental illness at all.
“I was like, ‘This is you healing,’ ” she said. “This is you, coming alive.”
She told Daniel that she couldn’t promise he would never have another manic episode. But she could tell him that her own fear had dissipated, over time. “I get to write my own story from here on in,” she said. “And that takes an act of faith.”
Housewives and retirees
Peer support around withdrawing from psychiatric medications dates back 25 years, to the early days of digital social networks.
Adele Framer, a retired information architect from San Francisco, discovered such groups in 2005 while going through a difficult withdrawal from Paxil. At the time, Ms. Framer said, physicians dismissed severe withdrawal as “basically impossible.”
People circulated between the groups, comparing “tapers” in “a viral information-sharing process,” said Ms. Framer, who launched her own site, Surviving Antidepressants, in 2011. Users on her site exchanged highly technical tapering protocols, with dose reductions so tiny that they sometimes required syringes and precision scales.
Dr. Mark Horowitz, an Australian psychiatrist, discovered Ms. Framer’s site in 2015 and used the peer advice he found to taper off Lexapro himself.
“At that point, I understood who the experts were,” he said. “I have six academic degrees, I have a Ph.D., I know how antidepressants work, and I was taking advice from retired engineers and housewives on a peer support site to help come off the drugs.”
In recent years, mainstream psychiatry has begun to acknowledge the need for more support for patients getting off medications.
This is most visible in Britain, whose health service has updated its guidance for clinicians to acknowledge withdrawal and recommend regular reviews to discontinue unnecessary medications. In 2024, the Maudsley Prescribing Guidelines in Psychiatry, a respected clinical handbook, issued its first “de-prescribing” volume. Dr. Horowitz was one of its authors.
There are early signs of movement in the United States, as well. Dr. Jonathan E. Alpert, chairman of the American Psychiatric Association’s Council on Research, said that the group plans to issue its own de-prescribing guide.
The American Society of Clinical Psychopharmacology is working on a guide to help doctors identify when a medication should be discontinued. “There has never been an incentive in industry to tell people when to stop using their product,” said Dr. Joseph F. Goldberg, the group’s president. “So it really falls to the nonindustry community to ask those questions.”
Dr. Gerard Sanacora, the director of the Yale Depression Research Program, said there are practical reasons the current health care system “doesn’t provide much support” for patients seeking to reduce medications: Relapse prevention can be time-consuming, and many physicians are only reimbursed for 15-minute “med management” appointments.
But he said it was important that trained clinicians still have a role. In a “taper,” patients encounter difficulties of two kinds: withdrawal, and the relapse of underlying conditions. It takes skill to distinguish between them, he said, and a licensed practitioner guarantees “some level of minimum competency” during a period of especially high risk.
“The main thing is, they can worsen and kill themselves,” he said of patients.
A success story
Ms. Delano entered the conversation in 2010, when she began blogging about her life. She was 27 years old, living with her aunt and uncle and attending day treatment at McLean Hospital in Massachusetts. Her platform was Mad in America, a website where a range of former psychiatric patients exchanged stories about their treatment.
Within that subculture, Ms. Delano stood out for her eloquence and charisma. She had grown up in Greenwich, Conn., where she was a top student and standout athlete. A relative of Franklin D. Roosevelt, she was presented as a debutante on two successive nights at New York’s Waldorf Astoria and Plaza hotels.
On her blog, and later in a 10,000-word profile in The New Yorker, she described the shadow plot of her psychiatric treatment.
In ninth grade, she was diagnosed with bipolar disorder and prescribed Depakote and Prozac. In college, her pharmacologists added Ambien and Provigil. Over the years, this list expanded, but she still seemed to be getting worse. Four times she was so desperate that she checked herself into psychiatric hospitals. At 25, she made a harrowing attempt at suicide.
Then, at 27, she picked up a book by the journalist Robert Whitaker, “Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America.” In the book, Mr. Whitaker proposed that the increasing use of psychotropic medications was to blame for the rise in psychiatric disorders. In scientific journals, reviewers dismissed Mr. Whitaker’s analysis as polemical, cherry-picking data to support a broad, oversimplified argument.
But for Ms. Delano, it was an epiphany. She mentally reviewed her treatment history and came to a radical conclusion. “I’d been confronted with something I’d never considered,” she writes in “Unshrunk.”“What if it wasn’t treatment-resistant mental illness that had been sending me ever deeper into the depths of despair and dysfunction, but the treatment itself?”
She quit five drugs over the six months that followed, under the guidance of a psychopharmacologist. She describes a brutal withdrawal, complete with constipation, diarrhea, aches, spasms and insomnia, as “angsty energy that had lived in me for years began to scratch viciously beneath the surface of my skin.”
But she also experienced a kind of awakening. “I knew it as clear as day, the second it occurred to me,” she writes. “I was ready to stop being a psychiatric patient.”
Born in 1983, five years before Prozac entered the market, Ms. Delano was part of the first large wave of Americans to be prescribed medications in their teens. Many readers recognized, in her blog entries, elements of their own stories — the way a diagnosis had become part of their identities, the way a single prescription had expanded into a cocktail.
She also provided something the ex-patient community had lacked: an aspirational model. Her life had clearly flourished after quitting her medications. In 2019 she married Mr. Davis, an activist she met in the ex-patient movement; they are raising two boys in an airy, sun-drenched colonial-style house.
On the Surviving Antidepressants website, users sometimes invoked her name wistfully.
“I thought I’d be like a Laura Delano and others and heal right away,” a user from Kansas commented.
A French user, struggling to wean off Valium, returned to Ms. Delano’s videos as to a mantra.
“9.30 am: I manage to stop a panic attack with agitation, by breathing.
10:30 a.m.: It rains. I spend time on my smartphone. Laura Delano. Laura Delano. Laura Delano. On a loop. Maybe I’m in love.”
‘I feel for psychiatry’
Emails began to flow in to Ms. Delano as she blogged about quitting her medications. Most were from people who wanted her advice on tapering. Often, she said, they had tried to taper too fast and were spinning out.
She encouraged them, assuring “overwhelmed, exhausted partners and parents” that what they were witnessing was not relapse, but withdrawal. Ms. Delano found that she was spending 25 hours a week on these calls. And a coaching business was born.
“I saw the demand for what I had to offer and made the difficult decision to stop giving my time away for free,” she writes in her memoir.
The market for assisting withdrawal from psychiatric medications is becoming crowded these days, with some private clinics charging thousands of dollars a week. And a watershed moment arrived last month, when Health Secretary Robert F. Kennedy Jr. announced that the new “Make America Healthy Again” commission would examine the “threat” posed by antidepressants and stimulants.
Mr. Kennedy has long expressed skepticism about psychiatric medications; in his confirmation hearings, he suggested that selective serotonin reuptake inhibitors, or S.S.R.I.s, have contributed to a rise in school shootings, and that they can be harder to quit than heroin. There is no evidence to back up either of these statements. But Mr. Davis agreed.
“He might be the only person in the room who gets how serious it can be,” Mr. Davis wrote on X during the hearings.
Ms. Delano and Mr. Davis both offer coaching — for $595 a month, you can join a group support program. But the project that excites them more is the membership community hosted by their nonprofit, Inner Compass Initiative, which, for $30 a month, links up members via livestreams, Zoom gatherings and a private social network.
They dream of a national “de-prescribing” network along the lines of Alcoholics Anonymous, said Mr. Davis, who became the group’s executive director early this year. “We know there is a sea change coming,” he said. “It’s already beginning. In a lot of circles, it’s deeply unfashionable to take psych meds.”
Ms. Delano has tempered her language since her Mad in America Days, when she protested outside annual meetings of the American Psychiatric Association, denouncing the use of four-point restraints and electroshock machines.
In the early pages of her memoir, she assures readers that she is not “anti-medication” or “anti-psychiatry.”
“To be clear, I am neither of these things,” she writes. “I know that many people feel helped by psychiatric drugs, especially when they’re used in the short term.”
Still, there is no mistaking the bedrock of mistrust that underlies her project. “I feel for psychiatry,” she said. “It’s a big ask we’re putting on them, to basically step back and consider that their entire paradigm of care is inadvertently causing harm to a lot of people.”
An echo chamber
Earlier this month, Mr. Davis flew to Washington to hand-deliver copies of “Unshrunk” to elected officials and explore whether Inner Compass might find new sources of funding in the new, pharma-skeptical dispensation. He wanted to make sure, he said, “that the people working on policy are at least considering our ideas.”
The rollout of Mr. Kennedy’s agenda has raised hopes throughout “critical psychiatry” and “anti-psychiatry” communities that their critiques will, for the first time, be taken seriously.
Some in the medical world fear this augurs a deepening mistrust in science. And it is true — the written resources Inner Compass provides are overwhelmingly negative about every major class of psychiatric medications, which remain the only evidence-based treatment for severe mental illnesses.
A section on antipsychotics, for instance, cites studies that purport to show that people who take them fare worse than people who never take them or stop them. (This is misleading; people do not take them unless they have severe symptoms.) A section on antidepressants cites a study suggesting that they cause people to commit acts of violence. (The study was criticized for distorting its findings.)
Dr. Alpert, who is also chairman of psychiatry and behavioral sciences at Montefiore Einstein, reviewed Inner Compass’s resources and described them as “biased” and “frightening.” He said online peer communities risk becoming “echo chambers,” since they tend to attract people who have had bad experiences with medical treatment.
Because quitting psychiatric medications can be so risky, he said, a pervasive mistrust of medical care could have serious consequences.
“I mean, what happens when people taper their medications because of an echo chamber, and they’re more suicidal, or they get more psychotic, and they need to be hospitalized, or they lose their job?” he said. “Who cares about those people?”
This worry was shared even by some of Ms. Delano’s admirers in the world of patient advocacy. Mr. Whitaker recalled acquaintances who, after setting out to quit their medications, fell into “despair.”
“Once you start going down that road, it becomes your identity,” said Mr. Whitaker. “People want to come off, and the next thing you know, there’s no service provider, no science, and they’re moving into that void.”
Numerous people in withdrawal communities described members who struggled with suicidal thinking, or who had died by suicide.
“More often than not, at least from what I’ve seen, once people conclude that the medications hurt them, then it’s all-or-nothing, black-and-white thinking,” said Kate Speer, a strategist for the Harvard T.H.Chan School of Public Health’s Center for Health Communication “They can’t recognize the providers are there to help, even when what they have done is not helpful.”
Ms. Delano said the issue of suicide comes up regularly in withdrawal communities. “I know so many people who have killed themselves over the years, in withdrawal or even beyond” she said. In 2023, a young woman who joined Inner Compass died by suicide, she said.
Afterward, Ms. Delano and Mr. Davis consoled distraught community members, who worried that they should have taken some action to intervene.
Ms. Delano said she would call 911 if a member overdosed on pills, but, short of that, she doesn’t weigh in on treatment choices. She noted that many members come to withdrawal groups precisely because they feel they have been harmed by the medical system.
“We have given psychiatry and licensed mental health professionals this godlike power to keep people alive,” she said. “Speaking for myself — this is not an organizational belief, but for me personally — I don’t think anyone should have that power over another human being.”
A ‘better me’
In Inner Compass gatherings, many people describe tapering processes as so difficult that they had to stop and reinstate medications. Some were on their fifth or sixth attempt, and some wept, describing how challenging it was.
Ms. Delano tries to keep the pressure off. “You’re in the driver’s seat,” she told one coaching client, who had reinstated a low dose of Valium. “It doesn’t mean, quote unquote, giving up or losing or failing.”
Daniel seemed to be looking for some inspiration to stick it out. He was getting better, he was sure of it, accessing levels of emotion that had been blunted by medication for 15 years.
He credited Ms. Delano for getting him this far; it was reading her story in the New Yorker that made him see it was possible to “come off the medications and be OK.” On a recent Zoom session, he showed her the Post-it note that he sometimes pulls out as a reminder to himself.
“IT WAS THE DRUGS,” he had written
“It was the drugs!” Ms. Delano exclaimed. She welled up toward the end of their session, reflecting on how much he had already achieved.
“The trade-off is worth it,” she told him. “The more your life expands — the meaning, the connection, the beauty, the possibility, the more that continues to expand in your life, the more all these beautiful things come online, the less weight, the less power the hard stuff has.”
When they hung up, he was feeling certain of his path again.
She has this effect on him, making him imagine how he will feel when he is off medication — “this better, more complete me,” as he put it. He thinks it will take two or three years to taper off completely.
If it proves too difficult, “I just have to take 450 milligrams and consider myself lucky,” he said. “But there is a desire to, you know, just kind of be free. Free of it.”
If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline or go to SpeakingOfSuicide.com/resources for a list of additional resources.

Science
Diablo Canyon clears last California permit hurdle to keep running

Central Coast Water authorities approved waste discharge permits for Diablo Canyon nuclear plant Thursday, making it nearly certain it will remain running through 2030, and potentially through 2045.
The Pacific Gas & Electric-owned plant was originally supposed to shut down in 2025, but lawmakers extended that deadline by five years in 2022, fearing power shortages if a plant that provides about 9 percent the state’s electricity were to shut off.
In December, Diablo Canyon received a key permit from the California Coastal Commission through an agreement that involved PG&E giving up about 12,000 acres of nearby land for conservation in exchange for the loss of marine life caused by the plant’s operations.
Today’s 6-0 vote by the Central Coast Regional Water Board approved PG&E’s plans to limit discharges of pollutants into the water and continue to run its “once-through cooling system.” The cooling technology flushes ocean water through the plant to absorb heat and discharges it, killing what the Coastal Commission estimated to be two billion fish each year.
The board also granted the plant a certification under the Clean Water Act, the last state regulatory hurdle the facility needed to clear before the federal Nuclear Regulatory Commission (NRC) is allowed to renew its permit through 2045.
The new regional water board permit made several changes since the last one was issued in 1990. One was a first-time limit on the chemical tributyltin-10, a toxic, internationally-banned compound added to paint to prevent organisms from growing on ship hulls.
Additional changes stemmed from a 2025 Supreme Court ruling that said if pollutant permits like this one impose specific water quality requirements, they must also specify how to meet them.
The plant’s biggest water quality impact is the heated water it discharges into the ocean, and that part of the permit remains unchanged. Radioactive waste from the plant is regulated not by the state but by the NRC.
California state law only allows the plant to remain open to 2030, but some lawmakers and regulators have already expressed interest in another extension given growing electricity demand and the plant’s role in providing carbon-free power to the grid.
Some board members raised concerns about granting a certification that would allow the NRC to reauthorize the plant’s permits through 2045.
“There’s every reason to think the California entities responsible for making the decision about continuing operation, namely the California [Independent System Operator] and the Energy Commission, all of them are sort of leaning toward continuing to operate this facility,” said boardmember Dominic Roques. “I’d like us to be consistent with state law at least, and imply that we are consistent with ending operation at five years.”
Other board members noted that regulators could revisit the permits in five years or sooner if state and federal laws changes, and the board ultimately approved the permit.
Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
Science
When slowing down can save a life: Training L.A. law enforcement to understand autism
Kate Movius moved among a roomful of Los Angeles County sheriff’s deputies, passing out a pop trivia quiz and paper prism glasses.
She told them to put on the vision-distorting glasses, and to write with their nondominant hand. As they filled out the tests, Movius moved about the City of Industry classroom pounding abruptly on tables. Then came the cowbell. An aide flashed the overhead lights on and off at random. The goal was to help the deputies understand the feeling of sensory overwhelm, which many autistic people experience when incoming stimulation exceeds their capacity to process.
“So what can you do to assist somebody, or de-escalate somebody, or get information from someone who suffers from a sensory disorder?” Movius asked the rattled crowd afterward. “We can minimize sensory input. … That might be the difference between them being able to stay calm and them taking off.”
Movius, founder of the consultancy Autism Interaction Solutions, is one of a growing number of people around the U.S. working to teach law enforcement agencies to recognize autistic behaviors and ensure that encounters between neurodevelopmentally disabled people and law enforcement end safely.
She and City of Industry Mayor Cory Moss later passed out bags filled with tools donated by the city to aid interactions: a pair of noise-damping headphones to decrease auditory input, a whiteboard, a set of communication cards with words and images to point to, fidget toys to calm and distract.
“The thing about autistic behavior when it comes to law enforcement is a lot of it may look suspicious, and a lot of it may feel very disrespectful,” said Movius, who is also the parent of an autistic 25-year-old man. Responding officers, she said, “are not coming in thinking, ‘Could this be a developmentally disabled person?’ I would love for them to have that in the back of their minds.”
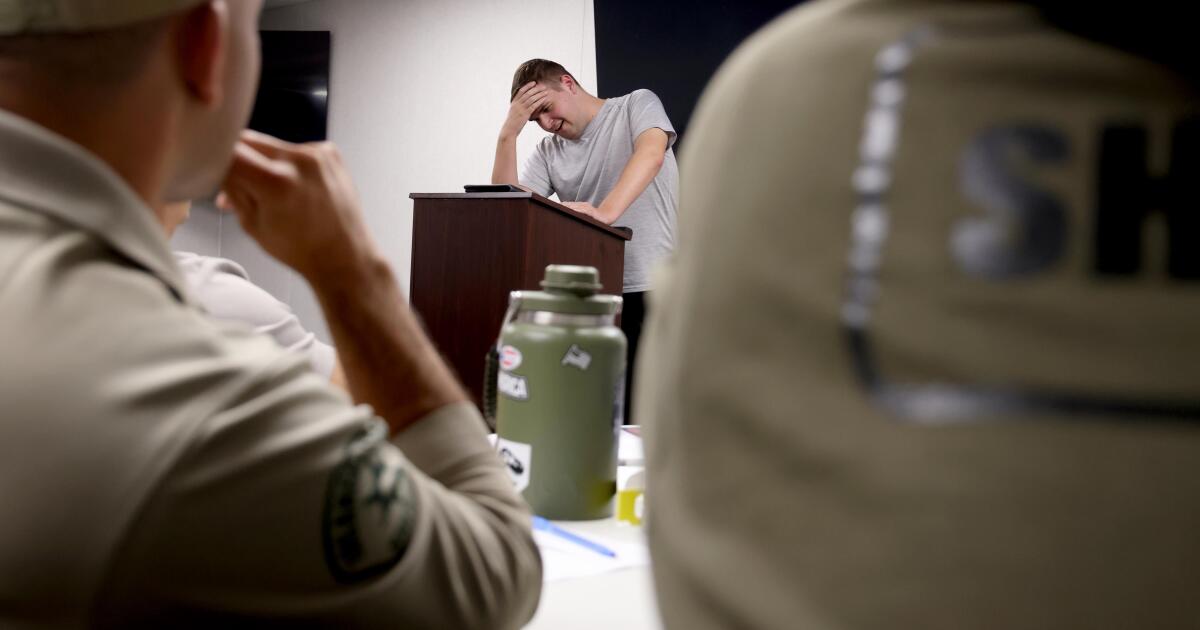
A sheriff’s deputy reads a pamphlet on autism during the training program.
(Genaro Molina / Los Angeles Times)
Autism spectrum disorder is a developmental condition that manifests differently in nearly every person who has it. Symptoms cluster around difficulties in communication, social interaction and sensory processing.
An autistic person stopped by police might hold the officer’s gaze intensely or not look at them at all. They may repeat a phrase from a movie, repeat the officer’s question or temporarily lose their ability to speak. They might flee.
All are common involuntary responses for an autistic person in a stressful situation, which a sudden encounter with law enforcement almost invariably is. To someone unfamiliar with the condition, all could be mistaken for intoxication, defiance or guilt.
Autism rates in the U.S. have increased nearly fivefold since the Centers for Disease Control began tracking diagnoses in 2000, a rise experts attribute to broadening diagnostic criteria and better efforts to identify children who have the condition.
The CDC now estimates that 1 in 31 U.S. 8-year-olds is autistic. In California, the rate is closer to 1 in 22 children.
As diverse as the autistic population is, people across the spectrum are more likely to be stopped by law enforcement than neurotypical peers.
About 15% of all people in the U.S. ages 18 to 24 have been stopped by police at some point in their lives, according to federal data. While the government doesn’t track encounters for disabled people specifically, a separate study found that 20% of autistic people ages 21 to 25 have been stopped, often after a report or officer observation of a person behaving unusually.
Some of these encounters have ended in tragedy.
In 2021, Los Angeles County sheriff’s deputies shot and permanently paralyzed a deaf autistic man after family members called 911 for help getting him to a hospital.
Isaias Cervantes, 25, had become distressed about a shopping trip and started pushing his mother, his family’s attorney said at the time. He resisted as two deputies attempted to handcuff him and one of the deputies shot him, according to a county report.
In 2024, Ryan Gainer’s family called 911 for support when the 15-year-old became agitated. Responding San Bernardino County sheriff‘s deputies shot and killed him outside his Apple Valley home.
Last year, police in Pocatello, Idaho, shot Victor Perez, 17, through a chain-link fence after the nonspeaking teenager did not heed their shouted commands. He died from his injuries in April.

Sheriff’s deputies take a trivia quiz using their non-writing hands, while wearing vision-distorting glasses, as Kate Movius, standing left, and Industry Mayor Cory Moss, right, ring cowbells. The idea was to help them understand the sensory overwhelm some autistic people experience.
(Genaro Molina / Los Angeles Times)
As early as 2001, the FBI published a bulletin on police officers’ need to adjust their approach when interacting with autistic people.
“Officers should not interpret an autistic individual’s failure to respond to orders or questions as a lack of cooperation or as a reason for increased force,” the bulletin stated. “They also need to recognize that individuals with autism often confess to crimes that they did not commit or may respond to the last choice in a sequence presented in a question.”
But a review of multiple studies last year by Chapman University researchers found that while up to 60% of officers have been on a call involving an autistic person, only 5% to 40% had received any training on autism.
In response, universities, nonprofits and private consultants across the U.S. have developed curricula for law enforcement on how to recognize autistic behaviors and adapt accordingly.
The primary goal, Movius told deputies at November’s training session, is to slow interactions down to the greatest extent possible. Many autistic people require additional time to process auditory input and verbal responses, particularly in unfamiliar circumstances.
If at all possible, Movius said, wait 20 seconds for a response after asking a question. It may feel unnaturally long, she acknowledged. But every additional question or instruction fired in that time — what’s your name? Did you hear me? Look at me. What’s your name? — just decreases the likelihood that a person struggling to process will be able to respond at all.
Moss’ son, Brayden, then 17, was one of several teenagers and young adults with autism who spoke or wrote statements to be read to the deputies. The diversity of their speech patterns and physical mannerisms showed the breadth of the spectrum. Some were fluently verbal, while others communicated through signs and notes.
“This population is so diverse. It is so complicated. But if there’s anything that we can show [deputies] in here that will make them stop and think, ‘Hey, what if this is autism?’ … it is saving lives,” Moss said.

Mayor Cory Moss, left, and Kate Movius hug at the end of the training program last November. Movius started Autism Interaction Solutions after her son was born with profound autism.
(Genaro Molina / Los Angeles Times)
Some disability advocates cautioned that it takes more than isolated training sessions to ensure encounters end safely.
Judy Mark, co-founder and president of the nonprofit Disability Voices United, says she trained thousands of officers on safe autism interactions but stopped after Cervantes’ shooting. She now urges families concerned about an autistic child’s safety to call an ambulance rather than law enforcement.
“I have significant concern about these training sessions,” Mark said. “People get comfort from it, and the Sheriff’s Department can check the box.”
While not a panacea, supporters argue that a brief course is better than no preparation at all. Some years ago, Movius received a letter from a man whose profoundly autistic son slipped away as the family loaded their car at the beach. He opened the unlocked door of a police vehicle, climbed into the back and began to flail in distress.
Though surprised, the officer seated at the wheel de-escalated the situation and helped the young man find his family, the father wrote to Movius. He had just been to her training.
-

 World1 day ago
World1 day agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts2 days ago
Massachusetts2 days agoMother and daughter injured in Taunton house explosion
-

 Montana1 week ago
Montana1 week ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Oklahoma1 week ago
Oklahoma1 week agoWildfires rage in Oklahoma as thousands urged to evacuate a small city
-

 Louisiana4 days ago
Louisiana4 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Technology6 days ago
Technology6 days agoYouTube TV billing scam emails are hitting inboxes
-

 Denver, CO2 days ago
Denver, CO2 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Technology6 days ago
Technology6 days agoStellantis is in a crisis of its own making
























