Science
This Nonprofit Health System Cuts Off Patients With Medical Debt

Many hospitals in the United States use aggressive tactics to collect medical debt. They flood local courts with collections lawsuits. They garnish patients’ wages. They seize their tax refunds.
But a wealthy nonprofit health system in the Midwest is among those taking things a step further: withholding care from patients who have unpaid medical bills.
Allina Health System, which runs more than 100 hospitals and clinics in Minnesota and Wisconsin and brings in $4 billion a year in revenue, sometimes rejects patients who are deep in debt, according to internal documents and interviews with doctors, nurses and patients.
Although Allina’s hospitals will treat anyone in emergency rooms, other services can be cut off for indebted patients, including children and those with chronic illnesses like diabetes and depression. Patients aren’t allowed back until they pay off their debt entirely.
Nonprofit hospitals like Allina get enormous tax breaks in exchange for providing care for the poorest people in their communities. But a New York Times investigation last year found that over the past several decades, nonprofits have fallen short of their charitable missions, with few consequences.
Allina has an explicit policy for cutting off patients who owe money for services they received at the health system’s 90 clinics. A 12-page document reviewed by The Times instructs Allina’s staff on how to cancel appointments for patients with at least $4,500 of unpaid debt. The policy walks through how to lock their electronic health records so that staffers cannot schedule future appointments.
“These are the poorest patients who have the most severe medical problems,” said Matt Hoffman, an Allina primary care doctor in Vadnais Heights, Minn. “These are the patients that need our care the most.”
Allina Health said it has a robust financial assistance program that in an average year helps over 12,000 of its 1.9 million patients with medical bills. The hospital system cuts off patients only if they have racked up at least $1,500 of unpaid debt three separate times. It contacts them by phone and with repeated letters that include information about applying for financial help, said Conny Bergerson, a hospital spokeswoman.
“Allina Health’s goal is, and will always be, to have zero patients go without services for financial reasons,” Ms. Bergerson said. She said that cutting off services was “rare” but declined to provide information on how often it happens.
Allina suspended its policy of cutting off patients in March 2020, at the onset of the coronavirus pandemic, before reinstating it in April 2021.
An estimated 100 million Americans have medical debts. Their bills make up about half of all outstanding debt in the country.
About 20 percent of hospitals nationwide have debt-collection policies that allow them to cancel care, according to an investigation last year by KFF Health News. Many of those are nonprofits. The government does not track how often hospitals withhold care.
Under federal law, hospitals are required to treat everyone who comes to the emergency room, regardless of their ability to pay. But the law — called the Emergency Medical Treatment and Labor Act — is silent on how health systems should treat patients who need other kinds of lifesaving care, like those with aggressive cancers or diabetes.
In 2020, thanks to its nonprofit status, Allina avoided roughly $266 million in state, local and federal taxes, according to the Lown Institute, a think tank that studies health care.
In exchange, the Internal Revenue Service requires Allina and thousands of other nonprofit hospital systems to benefit their local communities, including by providing free or reduced-cost care to patients with low incomes.
But the federal rules do not dictate how poor a patient needs to be to qualify for free care. In 2020, Allina spent less than half of 1 percent of its expenses on charity care, well below the nationwide average of about 2 percent for nonprofit hospitals, according to an analysis of hospital financial filings by Ge Bai, a professor at the Johns Hopkins Bloomberg School of Public Health.
Allina is one of Minnesota’s largest health systems, having largely grown through acquisitions. Since 2013, its annual profits have ranged from $30 million to $380 million. Last year was the first in the past decade when it lost money, largely owing to investment losses.
The financial success has paid dividends. Allina’s president earned $3.5 million in 2021, the most recent year for which data is available. The health system recently built a $12 million conference center.
Yet Allina sometimes plays hardball with patients. Doctors have become accustomed to seeing messages in the electronic medical record notifying them that a patient “will no longer be eligible to receive care” because of “unpaid medical balances.”
Dr. Rita Raverty, a primary care doctor who works at an Allina clinic, said the notifications were alarming because they meant she could not provide continuous care for some of her patients facing a number of health risks.
“Nobody wins when patients can’t get preventive care,” Dr. Raverty said. “It creates worse disease outcomes when you’re not catching things early.”
Doctors and patients described being unable to complete medical forms that children needed to enroll in day care or show proof of vaccination for school.
Serena Gragert, who worked as a scheduler at an Allina clinic in Minneapolis until 2021, said the computer system simply wouldn’t let her book future appointments for some patients with outstanding balances.
Ms. Gragert and other Allina employees said some of the patients who were kicked out had incomes low enough to qualify for Medicaid, the federal-state insurance program for poor people. That also means those patients would be eligible for free care under Allina’s own financial assistance policy — something many patients are unaware exists when they seek treatment.
Ms. Bergerson, the Allina spokeswoman, did not dispute that but said the health system goes “to tremendous lengths to assist patients with their financial obligations for medical care.”
Allina employees said the policy has forced them to ration care.
Beth Gunhus, a pediatric nurse practitioner, recalled a case in which a mother brought in her three children. One had scabies, an intensely itchy skin condition caused by mites burrowing into the body. She wanted to follow best practices and treat the entire family, who were sharing one bed in a single room they rented, to ensure it didn’t spread further. But she could write a prescription for only two of the children. The third’s account was locked because of unpaid bills.
“There are so many better ways of saving money than what we’re doing,” Ms. Gunhus said.
Allina says the policy applies only to debts related to care provided by its clinics, not its hospitals. But patients said in interviews that they got cut off after falling into debt for services they received at Allina’s hospitals.
Because Allina is the dominant health system in some rural parts of Minnesota, getting kicked out can leave patients with few options.
Jennifer Blaido lives in Isanti, a small town outside Minneapolis, and Allina owns the only hospital there. Ms. Blaido, a mechanic, said she racked up nearly $200,000 in bills from a two-week stay at Allina’s Mercy Hospital in 2009 for complications from pneumonia, along with several visits to the emergency department for asthma flare-ups. Ms. Blaido, a mother of four, said most of the hospital stay was not covered by her health insurance and she was unable to scrounge together enough money to make a dent in the debt.
Last year, Ms. Blaido had a cancer scare and said she couldn’t get an appointment with a doctor at Mercy Hospital. She had to drive more than an hour to get examined at a health system unconnected to Allina.
Allina does not make this policy explicit to patients. It is not mentioned in the health system’s list of “frequently asked questions” about billing practices. In at least one case, Allina has denied that it even existed.
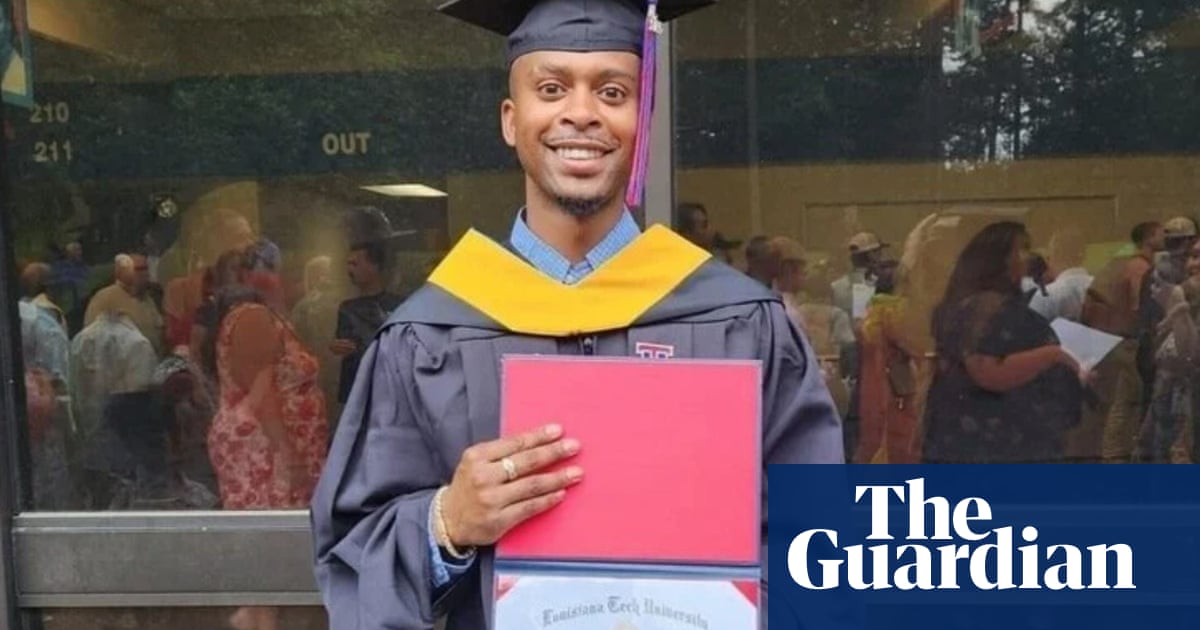
In a lawsuit filed last year in state court in Minnesota, Allina sued a couple, Jordan and JoLynda Anderson, for nearly $10,000 in unpaid medical bills.
In court filings, the couple described how Allina canceled Ms. Anderson’s appointments and told her that she could not book new ones until she had set up three separate payment plans — one with the health system and two with its debt collectors.
Even after setting up those payment plans, which totaled $580 a month, the canceled appointments were never restored. Allina allows patients to come back only after they have paid the entire debt.
Ms. Anderson recalls being devastated about losing her visit to an endocrinologist that specialized in a chronic condition she has. She had already been waiting four months for the appointment, and was unable to get a new one.
“It felt like I was being punished, and the punishment was you get to stay ill,” she said.
Ms. Bergerson declined to comment on these cases, citing patient privacy.
When the Andersons asked in court for a copy of Allina’s policy of barring patients with unpaid bills, the hospital’s lawyers responded: “Allina does not have a written policy regarding the canceling of services or termination of scheduled and/or physician referral services or appointments for unpaid debts.”
In fact, Allina’s policy, which was created in 2006, instructs employees on how to do exactly that. Among other things, it tells staff to “cancel any future appointments the patient has scheduled at any clinic.”
It does provide a few ways for patients to continue being seen despite their unpaid bills. One is by getting approved for a loan through the hospital. Another is by filing for bankruptcy.
Susan C. Beachy contributed research.

Science
Want to live to 100? That may depend on your sex

Do you want to live to 100? The path to becoming a healthy centenarian — as opposed to just a centenarian — is surprisingly different for those born as women and men, says social researcher and author Maddy Dychtwald. And it’s never too early to start on the journey, even when you’re young and spry. (We’re talking to you, zoomers.)
As co-founder of Age Wave, a nonprofit think tank focusing on longevity and aging, Dychtwald has been researching these topics for nearly 40 years. In her new book, “Ageless Aging: A Woman’s Guide to Increasing Healthspan, Brainspan, and Lifespan,” Dychtwald addresses the most recent aging picture for women and identifies a holistic plan for longevity. It weaves together science and medicine, psychology and spirituality, as well as financial advice in a research-based guidebook that’s brimming with actionable steps.
“There’s this ripple effect,” Dychtwald says of the lifestyle she recommends for maximizing healthspan — meaning how long you are living in good health, versus how long you are just living. “If you can impact one piece — sleep, nutrition, fitness, having a sense of purpose and connection — it begins to affect the others.” This interview has been edited for length and clarity.

Shelf Help is a new wellness column where we interview researchers, thinkers and writers about their latest books — all with the aim of learning how to live a more complete life.
How is longevity different for women than men?
Woman have actually won the longevity lottery. We live, on average in the United States, six years longer than men. So that’s incredibly positive. But there is a dark side to this. And that is: We women, on average, spend the last 12 to 14 years in declining health. So we are not doing a great job of matching our healthspan to our lifespan. There’s a gendered gap when it comes to healthspan. Why? I don’t know that the answer is clear, even in the minds of scientists. What we do know is that estrogen has protective properties for women. But once their estrogen levels decline, they have more health challenges than men do, as they get older. But it’s something scientists don’t fully understand yet.
If women are 51% of the population, doesn’t it stand to reason that scientists would better understand this by now?
You would think! I think the healthcare system, overall, is well-meaning. But it’s been created by men and as a result, the focus has really been more on men than women. One great example of how women can, as a community, really motivate physicians and researchers and scientists to change is the whole breast cancer issue. Women really spoke out on this and I think, as a result, we’ve seen great strides in research and survival rates and treatment methodologies.

Author Maddy Dychtwald.
(Lisa Keating Photography)
You endured a health challenge, which is one of the things that led to your writing this book. Can you tell us about that?
I’m a big exerciser, it’s how I manage stress. I started getting pain in my hips, to the point where I was limping. I did PT, I got cortisone treatments, I did a variety of things to manage the pain. But it wasn’t solving the problem. Turns out I needed double hip surgery — I was 68, which is young for the condition I had. But they couldn’t see me for months — and I was in excruciating pain. I started researching and learned, from experts in my network, that I needed to get my inflammation levels down. I went on an anti-inflammation diet — I cut out gluten, sugar and dairy — and I found that within six weeks all my pain went away. I thought: “Whoa, there are all these things that we can all do — and they don’t necessarily cost any money — to live better, longer.” I started looking at other things I could do. I worked with a psychiatrist at Harvard who taught me about meditation and affirmations. I was doing precovery, essentially — preparing for my surgery in advance. And it made a difference. This book is the distillation of all that, along with the work I’ve been doing at Age Wave for 40 years.
New research around genetics versus lifestyle choices also informs the book — and your decision to direct it at women. What does the latest research tell us about how to influence our destiny?
We used to just assume that genetics were our destiny. That whatever our genetic package is, that’s kind of the hand that we were dealt. But, in fact, according to the most recent science from Alphabet’s Calico Life Sciences and other research, up to 90% of our health and longevity are literally within our control. And I find that an incredibly empowering piece of information. It gives us almost total agency. I didn’t want to just keep that information to myself, I wanted to share it with the world. There are a lot of books out there on longevity, but there aren’t many that really focus in on women and longevity. And obviously, women and men are really different.
We used to just assume that genetics were our destiny. That whatever our genetic package is, that’s kind of the hand that we were dealt. But, in fact, according to the most recent science … up to 90% of our health and longevity are literally within our control.
— Maddy Dychtwald
During COVID, I was home more than I had been before. There were so many health issues I saw around me and I had an opportunity to really lean into my own sense of purpose. And in order to lean into it in a way that felt good to me, I wanted to [educate] women in their 40s, 50s, 60s and beyond. There are tens of millions of women just in the U.S. in that age group who are starting to feel the aches and pains of getting older, or who are coping with a chronic degenerative disease, or just dealing with the reality of menopause — and who are looking for solutions. I wanted to give women a one-stop resource to clear up the confusion, give them straightforward answers based on science as well as action steps to live better, longer.
You talk about a “holistic recipe” for healthy aging as a woman. What are the ingredients to that — what daily activities, for example, do you incorporate to promote longevity?
There are a lot of books out there on sleep or exercise or nutrition or hormones or having a positive attitude — and by the way, our attitudes toward our own aging can actually add 7½ years to our lifespan — but it’s not just about one thing, it’s all these things working together. They don’t exist in silos.
Take finances — there’s a gender pay gap. I encourage all women to take charge of their finances. If you don’t have your financial house in order, chances are it will affect your stress levels, your health, your well-being. And you may not even have the financial well-being to pay for your health — and that’s a scary place to be.
If you exercise effectively, it affects your mood and your stress. That helps with sleep, which helps with cognition and so many other things, including managing your finances. It’s cyclical.
Sleep is such a key ingredient. What do you do to manage that?
Sleep is not my superpower. But I learned there were things I could do. One was to really be mindful of my circadian rhythms; controlling our sleep-wake cycles are very important. I learned that what I did during the day was as important, if not more important, than what I did at night to go to sleep. It’s simple — anyone can do it — and it doesn’t cost a penny. Which is: When you get up first thing in the morning, watch the sun rise for 10 minutes. If it’s already up, get sun on your skin for 10 minutes. I do what I call “stacking my habits.” So at the same time, I do some breathing exercises that help me be calm and energetic simultaneously — what a great way to start my day.
One surprising piece of new research that you cite is that exercise has a bigger impact on health, and staving off brain decline later in life, for woman over men.
Yes. We already know that exercising in the morning is the best time of day to exercise, it brings optimal results, and it’s best on an empty stomach. But brand-new research, in a February 2024 study from the Smidt Heart Institute at Cedars-Sinai, says that women don’t have to exercise as hard, or as long, as men to get optimal results. They can get the same health benefits as men from exercise in less time.
For example, women can reduce their risk of death by 18% by doing 140 minutes of moderate aerobic exercise per week, while men need 300 minutes to achieve the same benefit. Women can also achieve the same survival benefit from moderate to vigorous aerobic exercise, like cycling or brisk walking, after 2½ hours per week, while men need about five hours. And when it comes to building muscle mass, strengthening exercises such as weightlifting or core exercises, women can achieve the same positive benefits after one session weekly while men need three sessions.
TAKEAWAYS
From “Ageless Aging”
You talk about two topics that demand the medical community’s much closer attention. What are they?
Brain health — no one wants to talk about anything above the neck — and hormones. Hormones affect our cognition, sleep, joints and bones, mood. If you’re not able to sleep at night, it affects your brain health, brainspan and longevity. If your bone density is impacted, you’re more likely to fall, and that could lead to health issues.
And Alzheimer’s disease is twice as likely to happen to women than men — people don’t want to talk about it. It’s super scary. But there are things we can do. Dr. Andrea Pfeifer, a neurosurgeon and CEO of AC Immune, a company working on a vaccine for Alzheimer’s, says probiotics are what she takes — the gut-brain connection is very real. Many physicians recommend the Mediterranean diet. I do the anti-inflammatory diet.
Another thing is limiting or stopping alcohol. And exercise — every single brain expert I spoke to said that’s the No. 1 thing to protect healthspan and brainspan. The fear of cognitive decline and Alzheimer’s for women is real, but only 4% of women have a genetic connection. And we can take steps to prevent or delay it.
Are there any positive sides of aging for women?
We gain a certain amount of wisdom and experience as we get older. According to recent studies we’ve done at Age Wave, women, as it turns out, from the age of 50 on, they seem to be gaining more confidence in themselves and their lives, whereas men seem to plateau out at around 50. This is all in general, of course. But for women, empowering.

Shelf Help is a new wellness column where we interview researchers, thinkers and writers about their latest books — all with the aim of learning how to live a more complete life. Want to pitch us? Email alyssa.bereznak@latimes.com.
Science
Like water sloshing in a giant bathtub, El Niño begins an inevitable retreat

A few weeks ago, the Australian Bureau of Meteorology declared that the Pacific Ocean is no longer in an El Niño state and has returned to “neutral.” American scientists at the National Oceanic and Atmospheric Administration have been more hesitant, but they estimate that there is an 85% chance that the Pacific will enter a neutral state in the next two months and a 60% chance that a La Niña event will begin by August.
After an El Niño that was one of the three strongest in the last 40 years and that brought a wet winter to the U.S. — and California, in particular — this transition could mean a dramatic shift in weather as we enter the summer.
The progression from El Niño to La Niña, which is part of a broad system called the “El Niño Southern Oscillation,” or ENSO, is the result of conditions in the tropical Pacific. During the neutral phase, which is or soon will be in effect, the so-called trade winds rush from east to west along the equator. These winds push warm surface water with them, bathing Indonesia and New Guinea in the balmy waters of the “Pacific Warm Pool” and forcing cold water to rise from the deep ocean along the coast of South America.
Aggressive and impactful reporting on climate change, the environment, health and science.
As an El Niño phase begins, these winds weaken, so that warm sea surface temperatures move east toward South America. This can cause climatic shifts across the globe: landslides in Peru, drought in Australia, fish die-offs in the eastern Pacific and more frequent atmospheric rivers in Southern California. These changing weather patterns also weaken the trade winds further, leading to more warm water off the coast of South America, which in turn weakens the winds, and so on.
So what prevents El Niño events from continuing to strengthen forever?
Well, it turns out you can think of the Pacific Ocean sort of like one enormous bathtub, and El Niño like a wave of warm water sloshing from one end of the bathtub to another. When that wave reaches the Ecuadorean coast, it bounces back, carrying the warm water back toward Asia and Oceania, which strengthens the trade winds, which push the warm water faster, until the wave reaches the other end of the “bathtub” — this is a La Niña phase, when the west Pacific is especially warm and the east Pacific especially cold — at which point the process repeats. This is the “oscillation” that gives ENSO its name, and it is why a strong La Niña event often follows a strong El Niño.
This winter’s El Niño event had sea surface temperature anomalies of 3.6 degrees (2 degrees Celsius), which qualifies it for the unofficial status of “very strong El Niño.” As is typical, the warm waters of El Niño led to high global temperatures, but because of the unprecedented effects of climate change, these temperatures were anything but typical. In December, when El Niño was at its peak, global surface temperatures were 0.45 degrees (0.25 degrees Celsius) above the next hottest December on record.
This increase may not seem so unusual given the current era of ever-climbing temperatures, but when you consider that the difference between the coldest December on record (back in 1916) and the second-hottest (in 2016) is less than 3.6 degrees, it is far more shocking — so surprising that prominent climate scientists have begun to publicly wonder whether there are elements missing from our understanding of climate change.
Fortunately, the onset of neutral ENSO conditions, followed by the likely La Niña, should begin to bring global temperatures down, at least temporarily. This will be little consolation for the U.S., as the National Weather Service predicts above-average summer temperatures for virtually the entire country. Moreover, La Niña events are associated with drier conditions across the southwestern U.S. that could persist into next winter. While this year’s generous Sierra snowpack should insulate California from the effects of a scorching summer, the state is never more than one below-average winter from a drought.
There are also potential implications for the rest of the country — La Niña has been linked to higher hail and tornado activity in the Southeast and an increase in hurricanes in the Atlantic and Gulf of Mexico. In fact, many experts are predicting a “hyperactive” hurricane season in the tropical Atlantic, with one forecast going as high as an unprecedented 33 named storms. On the flip side, however, there will probably be a slow hurricane season in the east Pacific, with little chance of a reprise of Hurricane Hilary’s passage over Southern California last August.
Of course, all of these forecasts — that La Niña tends to cause dry conditions in Southern California, that this location will get more hurricanes while that region gets more hail, and even how strong an El Niño or La Niña event can become — are based on correlations and theories that researchers have rigorously developed using data from the last half century.
But given the recent rapidity of climate change, there are no guarantees that the trends of the past will continue to hold in the future. In situations such as these, climate scientists generally look to computer models to understand how phenomena such as ENSO might shift over time.
Unfortunately, many climate models have not yet developed the ability to predict ENSO accurately — its complexity and the fact that it requires the ocean and atmosphere to shift in tandem make it particularly challenging to represent. This means that as we move into a new era of accelerating climate change, the future of ENSO remains uncertain.
Ned Kleiner is a scientist and catastrophe modeler at Verisk. He has a doctorate in atmospheric science from Harvard.
Science
Video: Northern Lights Glow in the Sky Amid Solar Storm

new video loaded: Northern Lights Glow in the Sky Amid Solar Storm
transcript
transcript
Northern Lights Glow in the Sky Amid Solar Storm
Powerful solar flare activity made the aurora borealis visible unusually far south.
-
[Laughing] Holy moly. I know. This — I thought it would just be over on the horizon a little — Behind us, too. Yeah. A little green on the horizon. Nothing like this. This is — This is like, ‘Oh, my god.’ Everywhere.
Recent episodes in Science
-

 Politics1 week ago
Politics1 week agoHouse Dems seeking re-election seemingly reverse course, call on Biden to 'bring order to the southern border'
-

 World1 week ago
World1 week agoSpain and Argentina trade jibes in row before visit by President Milei
-
 Politics1 week ago
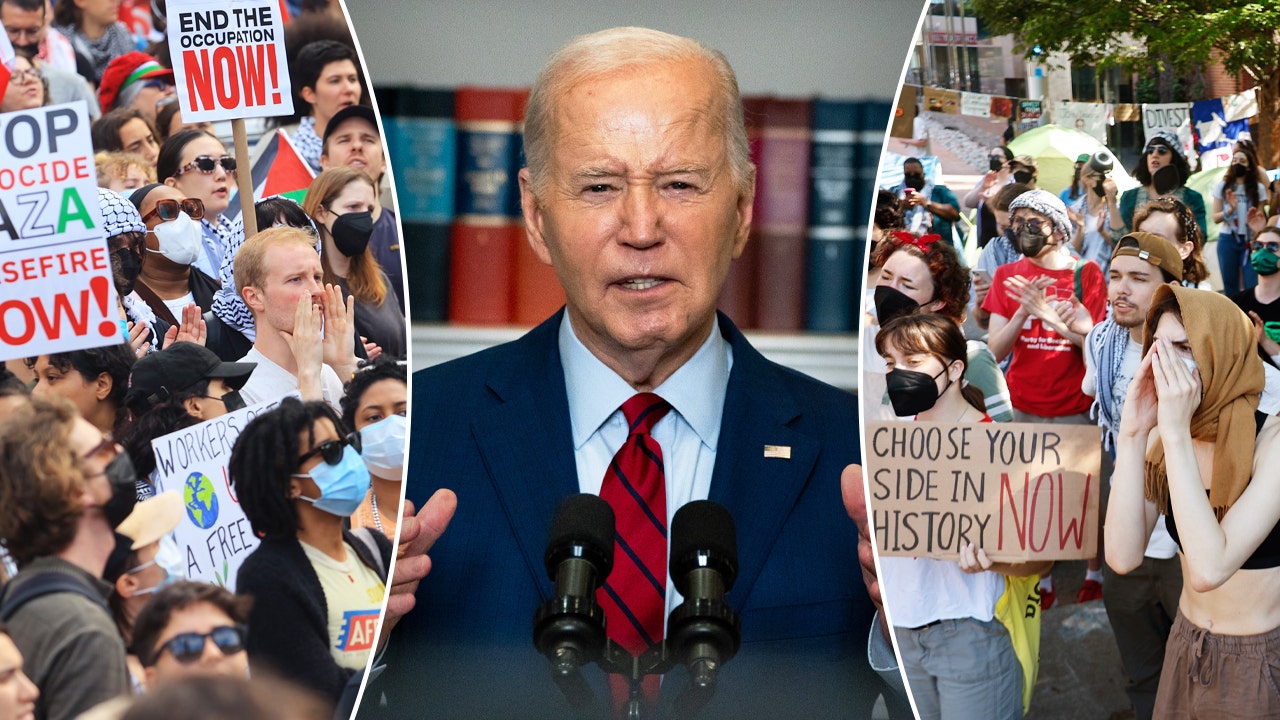
Politics1 week agoAnti-Israel groups accuse Chicago, DNC of trying to ‘protect’ Biden from protests at 2024 Dem convention
-

 World1 week ago
World1 week agoGerman socialist candidate attacked before EU elections
-

 Politics1 week ago
Politics1 week agoFetterman says anti-Israel campus protests ‘working against peace' in Middle East, not putting hostages first
-
 News1 week ago
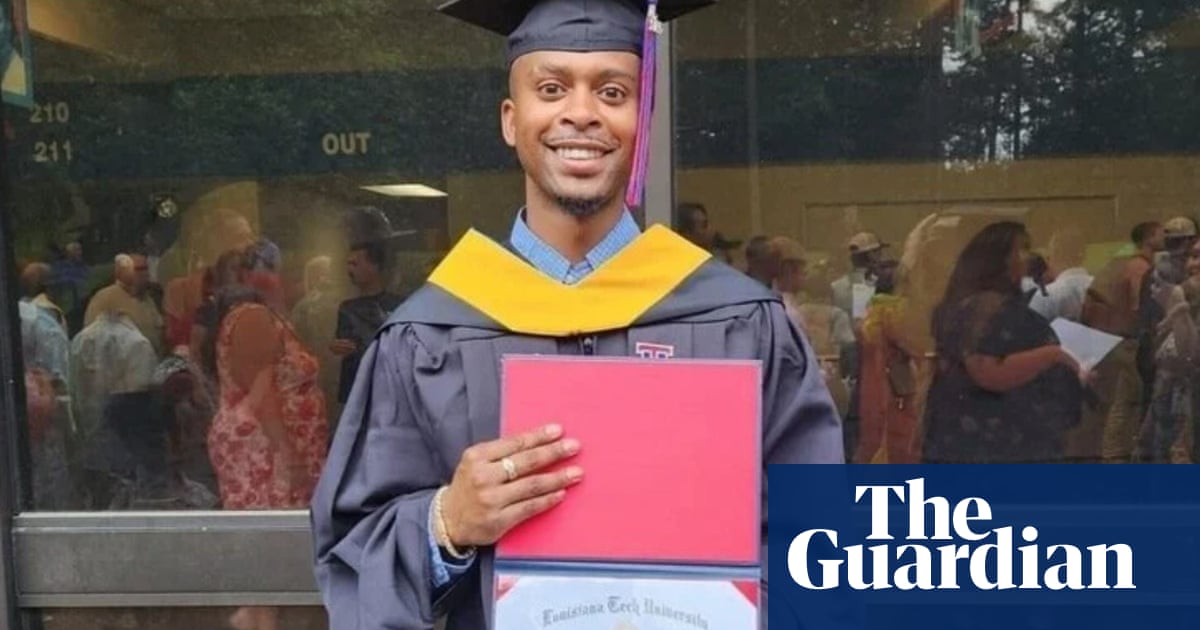
News1 week agoUS man diagnosed with brain damage after allegedly being pushed into lake
-

 World1 week ago
World1 week agoGaza ceasefire talks at crucial stage as Hamas delegation leaves Cairo
-

 Politics1 week ago
Politics1 week agoRepublicans believe college campus chaos works in their favor
















Pingback: Report Calls Out Healthcare Provider for Canceling Appointments for Patients With Unpaid Debts – AccountsRecovery.net