Health
Pastor based in Dallas shares depression journey, urges others to seek help: ‘Don’t hesitate’

Pastors and other clergy members often serve as pillars of support in times of crisis. Yet what happens when they’re the ones who need to be lifted up?
Mark Dance, a former pastor who lives in Dallas, knows firsthand that mental health struggles can impact those in church leadership.
During his three decades of leading various churches, Dance, now 59, experienced a three-year bout of clinical depression — and now, as a pastor advocate for GuideStone, he helps support other pastors who are struggling.
ILLINOIS PASTOR AND AUTHOR URGES OTHERS AMID TODAY’S EVIL, ‘MAKE AMERICA LOVE AGAIN’
He revealed the details of his story to Fox News Digital.
The ‘three-year fog’
Dance’s mental health challenge began about 15 years ago, when he was in his third pastoral position, he said.
Mark Dance, pictured with his wife, Janet Dance, said he suffered through a three-year period of depression while serving as a pastor. (Dr. Mark Dance)
He and his wife, Janet Dance, were busy navigating life in ministry while raising teenagers — and they were also in the middle of a major move from one church campus to another.
“I noticed that I had become different,” he told Fox News Digital. “I was avoiding people, where I used to love being with people. And it became difficult to sleep, eat and make decisions.”
“I was working way too much, and using ‘the God card’ as an excuse.”
Dance also noticed that he’d lost a significant amount of weight. It was a period that he now refers to as a “three-year fog.”
“I was working way too much, and using ‘the God card’ as an excuse,” he said.
FLORIDA MOM-TO-BE GETS SURPRISE OF HER LIFE FROM HER OWN MOTHER: ‘WISH FULFILLED’
“I was a ‘churchaholic’ who refused to receive the gift of a day off and did not honor the Sabbath. I was neglecting myself, and it just all caught up with me.”
Dance had been down before, he said, but usually he was able to shake it off within a week or two. “But this time, I was stuck for a long time,” he said.
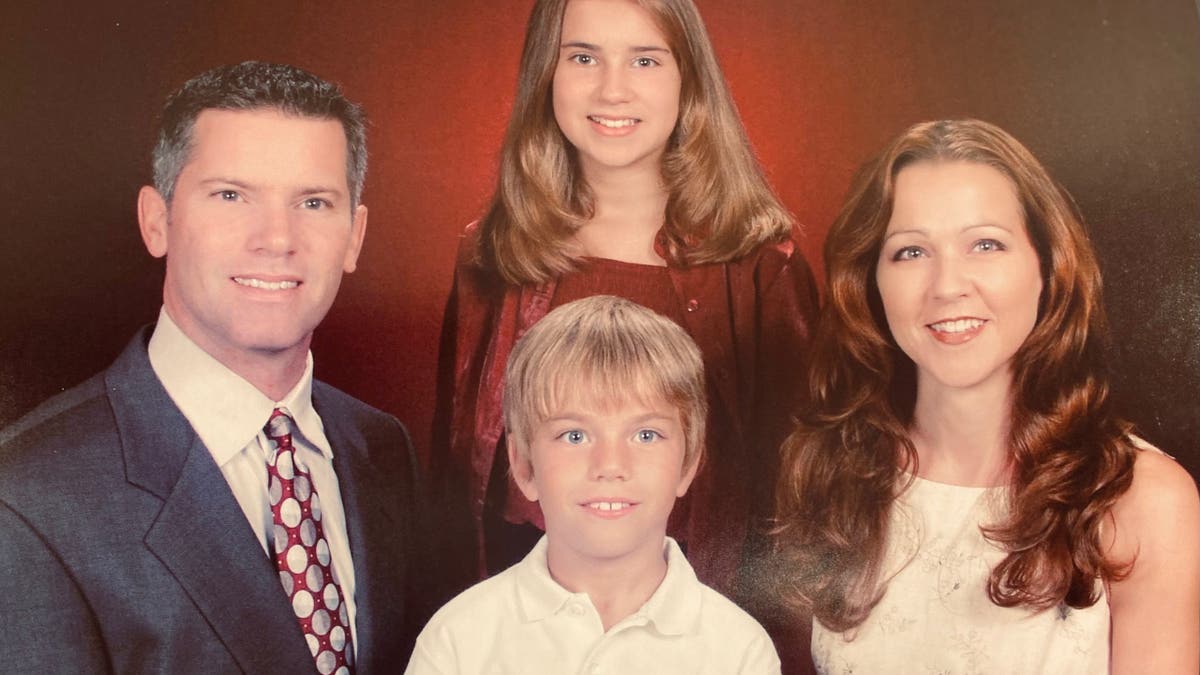
Mark Dance is pictured with his family in 2002. He and his wife, Janet Dance, were busy navigating a life in the ministry while raising their teenagers when his depression journey began, he said. (Dr. Mark Dance)
Although it was “out of character” for him to ask for help, Dance reached out to his family physician — who diagnosed him with clinical depression, prescribed medication and told him to “throttle down.”
By slowing down and focusing on his own needs, Dance was eventually able to “get healthy again.”
A few years later, he transitioned into a new role of helping other pastors overcome their own mental health struggles.
Those in church leadership are just as vulnerable to mental health struggles as the people they serve, Dance said.
“My clinical depression was equivalent to a common cold compared to some other types,” he told Fox News Digital.
AMERICAN VETERANS WHO COMMIT SUICIDE ARE 95% MALE, CRISIS OFTEN DRIVEN BY FAMILY DISPUTES, SAY EXPERTS
“Depression is kind of like cancer in that regard — there are different levels. In my case, it was diagnosed early and was treatable.”
Learning to practice self-compassion
While it might seem that those in church leadership are perpetually strong, they are just as vulnerable to mental health struggles as the people they serve, Dance said.
“We deal with the same issues — health problems, marriage challenges, problems with kids or money,” he said. “But it is more difficult for us to ask for help because it’s counterintuitive for us as caregivers.”

“My wife is my biggest fan and advocate,” Dance said. “Janet stepped up and became the leader of our home and our marriage for about three years, when I couldn’t lead anything.” (Dr. Mark Dance)
A pastor feels compelled to succeed both at work and at home, Dance noted — “because our spouse and kids are in our job description in the Bible.”
That can lead to unrealistic expectations and added pressure, he said.
“About one out of four pastors will experience a mental health challenge,” he told Fox News Digital. “And I just happened to be one of those.”
ILLINOIS PASTOR AND AUTHOR URGES OTHERS AMID TODAY’S EVIL, ‘MAKE AMERICA LOVE AGAIN’
Dr. Norman Blumenthal, director of the Ohel Zachter Family National Trauma Center in New York, noted that members of the clergy are often “benevolent and idealistic individuals” who extend themselves to others, even at the expense of their own well-being.
“It’s essential to remember that charity and care entail giving generously, but not excessively,” Blumenthal, who is not associated with GuideStone, told Fox News Digital.
“We can give a piece of ourselves, but not ourselves in entirety. When setting limits and triaging those we help, clergy often provide more effectively and abundantly than less.”
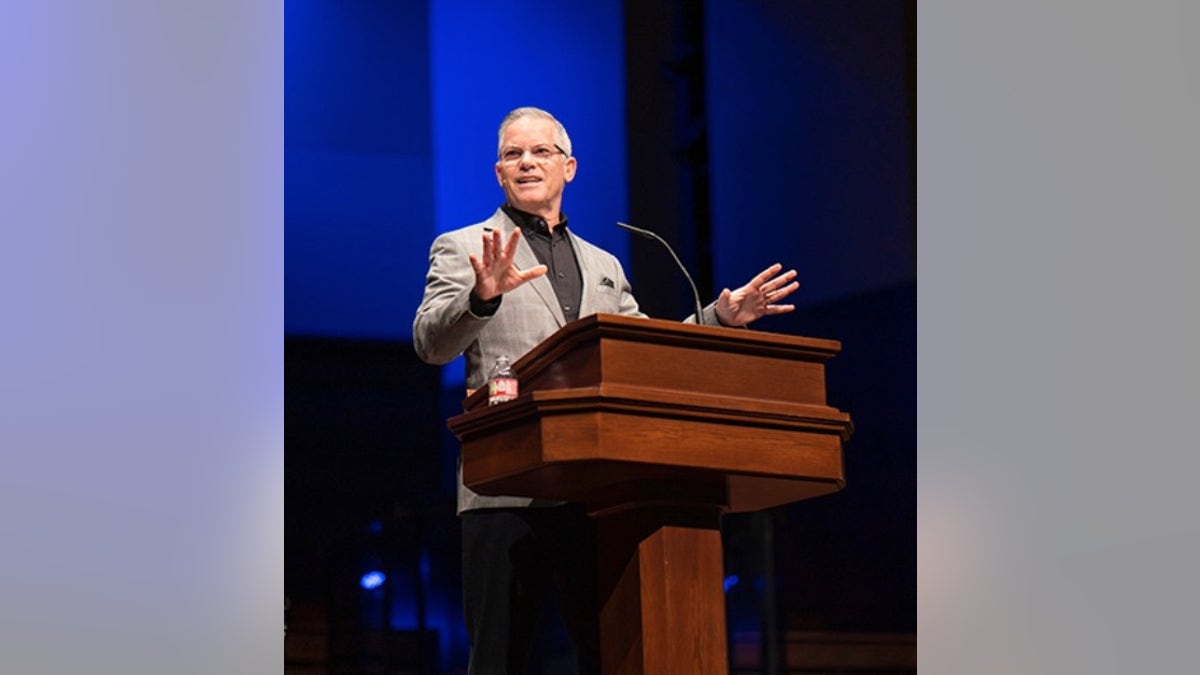
While it might seem that those in church leadership are perpetually strong, they are just as vulnerable to mental health struggles as the people they serve, Dance pointed out. (Dr. Mark Dance)
While pastoring requires compassion for others, exercising self-compassion is just as important, according to Yale University’s Dr. Emma Seppälä, author of “Sovereign: Reclaim your Freedom, Energy and Power in a Time of Distraction, Uncertainty, and Chaos.”
“Often, people in service-oriented professions give a lot to others without taking into account that they need to give to themselves as well,” Connecticut-based Seppälä, who is also not associated with GuideStone, told Fox News Digital.
“As I tell pastors, the only thing between you and help is your pride.”
“You can’t easily give from an empty cup. Self-compassion is the ability to treat oneself as one would treat a loved one — with kindness, consideration, respect and nurturing.”
This might include the ability to set boundaries so that there is enough time in the day to get exercise or proper nutrition, Seppälä added.
“Ideally, pastors should include themselves in their ministry.”
Having the courage to ask for help
Clergy members who experience depression or other mental health conditions need just as much help as the general population, Dance said.
While counseling others dealing with depression, he often hears the common sentiment that depression “sneaks up on you.”

Mark Dance (far right) is pictured in a recent photo with his wife, Janet Dance, and the couple’s children, Brad and Holly. (Dr. Mark Dance)
“It’s usually not a big freight train that runs you over,” he said. “It can start with lack of sleep, or a dramatically increased or decreased appetite. It can be very subtle.”
Reaching out for help takes courage and humility, Dance pointed out.
“As I tell pastors, the only thing between you and help is your pride,” he said.
NURSES CALL FOR CHANGE AS MANY REVEAL THEY’RE ‘EXTREMELY LIKELY’ TO LEAVE PROFESSION: ‘EMOTIONAL, STRESSFUL’
In his role, Dance often tells preachers, “Don’t self-diagnose and don’t hesitate to ask for help.”
“God has not called us to be competent in everybody else’s profession — if you’re a pastor, it’s OK not to be a mental, physical or financial health professional. Just be a pastor and let other people help you.”

Dance’s wife, Janet, encouraged him to seek help during his struggles. Clergy members who experience depression or other mental health conditions need just as much help as the general population, Dance said. (Dr. Mark Dance)
At GuideStone, Dance said, the focus is on helping pastors and ministers to “stay well and finish well.”
“I help people think about what a strong finish would look like at the end of their ministry, and it’s very fulfilling.”
Supported by faith
During Dance’s depression journey, he relied on his church and his faith to get him through.
“Church is a place where you can grow in all areas — not just one,” he said. “For me, church became a place where I could receive help from my own members.”
“And that’s the experience I’ve had for the last 36 years of industry — if the pastors ask for help, the church members will reciprocate.”
“I learned to become more physically, mentally and spiritually healthy, through the process of my mind being renewed by the Lord and His people.”
The pastor also drew strength from the Bible — particularly his favorite verse, below.
“Do not conform to the pattern of this world, but be transformed by the renewing of your mind. Then you will be able to test and approve what God’s will is — his good, pleasing and perfect will” (Romans 12:2).
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Listening to God is an important part of self-care, according to Dance.
“He’s the one who designed us — He knows how to help us stay well,” he said. “I learned to become more physically, mentally and spiritually healthy, through the process of my mind being renewed by the Lord and His people.”
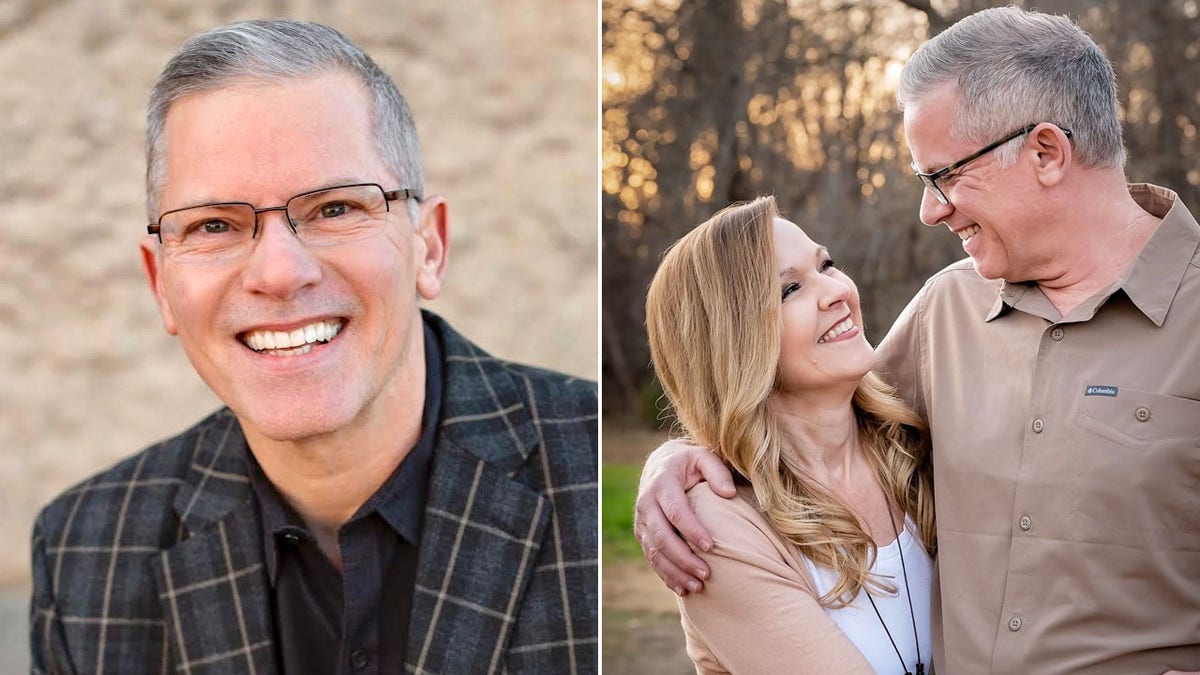
Pastors and others can visit www.GuideStone.org/mentalhealth to see Dance’s video testimony and to get support from a pastoral counselor, Dance told Fox News Digital. (Dr. Mark Dance)
Dance also draws support from his wife of 36 years and their two children.
“My wife is my biggest fan and advocate,” he said. “Janet stepped up and became the leader of our home and our marriage for about three years, when I couldn’t lead anything.”
“She’s a big part of how I got healthy and how I’m staying healthy.”
Pastors and others can visit www.GuideStone.org/mentalhealth to see Dance’s video testimony and to get support from a pastoral counselor.
For more Health articles, visit www.foxnews.com/health.

Health
What Happens If You Eat Eggs Every Day? Nutritionists Share the Benefits

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Ask a doctor: ‘I swallowed a bug — now what should I do?'

Most people have experienced that moment of discomfort when they realize a bug has wound up where it shouldn’t be — in their windpipe.
That includes Taylor Swift, who on more than one occasion has accidentally swallowed a bug while performing on stage in front of thousands of people.
It can be a startling and somewhat disgusting occurrence — but is this dangerous, or just a nuisance?
LOCAL DENGUE FEVER CASES CONFIRMED IN FLORIDA KEYS, SPREAD BY MOSQUITO BITES
Dr. Raj Dasgupta, a quadruple board-certified physician in California, shared with Fox News Digital the true impacts of accidentally swallowing a bug, and the best thing to do if it happens.
“Swallowing a bug can often happen accidentally when you’re eating or drinking outside, or if a bug flies into your mouth,” Dasgupta, who serves as chief medical advisor for Fortune Recommends, told Fox News Digital via email.
Dr. Raj Dasgupta, a quadruple board-certified physician in California, discussed the impact of accidentally swallowing a bug — and the best thing to do if it happens. (Sleepoplis)
“It can also happen if you’re talking or laughing outdoors. Sometimes it might even happen indoors if bugs are in your food or drink and you don’t realize it.”
ASK A DOCTOR: ‘HOW CAN I PREVENT SCARRING FROM BUG BITES AND POISON IVY?’
Swallowing a bug is usually not dangerous, Dasgupta noted.
“The stomach’s digestive acids usually break down the bug, and it is passed out of the body without causing harm,” he said.

“Swallowing a bug can happen accidentally when you’re eating or drinking outside, or if a bug flies into your mouth,” the doctor told Fox News Digital. (iStock)
If the bug carries harmful bacteria or parasites, however, it could cause gastrointestinal issues or allergic reactions, according to the doctor.
The type of bug can make a difference, he said.
“Bugs like beetles or ants are less of a concern, but bugs that are known to spread diseases — such as mosquitoes — might be riskier.”
If you happen to swallow a bug, drinking some water can help wash it down, Dasgupta said.

Taylor Swift has announced the accidental swallowing of bugs, mid-concert, on more than one occasion. (Marcelo Endelli/TAS23/Getty Images for TAS Rights Management)
“If you start feeling sick, like abdominal pain, vomiting or nausea, keep an eye on your symptoms,” the doctor said.
If you have severe stomach pain, ongoing vomiting, trouble breathing, or swelling, rash or itching, Dasgupta said to see a doctor.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“If you know the bug could have diseases or if you have health conditions that might complicate things, it’s a good idea to get checked out to be safe,” he added.
For more Health articles, visit www.foxnews/health
Some bugs — including grasshoppers, beetles, termites, mealworms and even stink bugs — are actually considered edible in certain countries, and are prepared and eaten as part of meals, according to WebMD’s website.
Health
“I’m a Dietitian, and Here’s Why an Overly Restrictive Diet Can Backfire”

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
-

 World1 week ago
World1 week agoOne dead after car crashes into restaurant in Paris
-
 Midwest1 week ago
Midwest1 week agoMichigan rep posts video response to Stephen Colbert's joke about his RNC speech: 'Touché'
-

 News1 week ago
News1 week agoVideo: Young Republicans on Why Their Party Isn’t Reaching Gen Z (And What They Can Do About It)
-

 Movie Reviews1 week ago
Movie Reviews1 week agoMovie Review: A new generation drives into the storm in rousing ‘Twisters’
-

 News1 week ago
News1 week agoIn Milwaukee, Black Voters Struggle to Find a Home With Either Party
-
 Politics1 week ago
Politics1 week agoFox News Politics: The Call is Coming from Inside the House
-

 News1 week ago
News1 week agoVideo: J.D. Vance Accepts Vice-Presidential Nomination
-

 World1 week ago
World1 week agoTrump to take RNC stage for first speech since assassination attempt















