Science
Bob Saget’s death calls attention to head injuries. What should you look out for?

The demise of fashionable comic Bob Saget whereas on tour in Florida final month was shocking and tragic, however the damage that claimed his life is extra widespread than you would possibly suppose.
In response to the medical expert in Florida who carried out the post-mortem, Saget most definitely fell and struck the again of his head, inflicting bleeding on his mind. Saget’s household mentioned he in all probability thought nothing of the damage and went to sleep. A lodge worker discovered him useless in mattress the following afternoon.
On a typical day, mind accidents like Saget’s declare the lives of greater than 160 individuals in america, the Facilities for Illness Management and Prevention says. About 61,000 individuals died from a traumatic mind damage, or TBI, within the U.S. in 2019 alone.
Granted, the commonest reason for demise from TBI is a gun-related suicide. Automotive crashes and assaults are different widespread sources of those accidents. However nearly half the hospitalizations from TBI come from the straightforward act of falling down, the CDC says.
Saget was 65, placing him in an age group that’s significantly inclined to damaging falls. A 2006 examine revealed by the Journal of the American Geriatrics Society discovered that “in individuals aged 65 and older, TBI is liable for greater than 80,000 emergency division visits every year; three-quarters of those visits lead to hospitalization because of the damage.” Greater than half of these accidents resulted from falls.
In response to the CDC, “information recommend that some teams are at larger threat of dying from a TBI or experiencing long-term well being issues after the damage.” These teams embody racial and ethnic minorities, members and veterans of the armed companies, homeless individuals, and residents of rural areas.
Everybody hits their head on one thing sooner or later of their lives. So how do you inform when there’s trigger for alarm? Right here’s some recommendation from three specialists on mind accidents: Dr. Christopher C. Giza, director of the UCLA Steve Tisch BrainSport Program; Dr. Could Kim-Tenser, a neurologist with Keck Medication of USC; and Dr. Joshua Marcus, a neurosurgeon at Nuvance Well being in Connecticut.
What causes a traumatic mind damage?
1000’s of People endure traumatic mind accidents yearly, however incidents like those that claimed Saget’s life are uncommon. And though head traumas are “tremendous widespread,” Marcus mentioned, “the overwhelming minority lead to something critical.”
Bumping the headboard as you’re entering into mattress shouldn’t ship you to the hospital. “It must be a reasonably traumatic fall,” Kim-Tenser mentioned. “It actually must be a reasonably arduous hit to the top,” involving a tough influence on a tough floor.
Giza agreed. “Hitting your head on the headboard just isn’t going to create plenty of power,” he mentioned. In contrast, he mentioned, “slipping within the lavatory and hitting your head on the aspect of the bath goes to have appreciable power.”
The mind can be injured in a much less direct manner, when a forceful occasion — a automotive wreck, for instance — shoves it in opposition to the cranium. A shearing damage is when “the mind goes a technique, the power goes the opposite manner,” Marcus mentioned. Then there are contracoup accidents, when a power on one aspect of the top sends the mind into the cranium on the opposite aspect.
The injury is prompted when a blood vessel contained in the cranium ruptures, inflicting blood to pool between the mind and its environment. “The cranium is a closed field, largely,” Giza mentioned, “so in case you begin filling up a part of that house with bleeding, the remainder of the stuff will get squished.”
When you begin squeezing the mind, it doesn’t work very nicely. Folks can go right into a coma or change into paralyzed. And if the strain is utilized to the mind stem (the half close to the spinal wire), it might probably intervene with an individual’s respiratory and heartbeat, Giza mentioned. Past that, he mentioned, the pooled blood irritates the floor of the mind, probably triggering seizures.
Giza and Marcus mentioned that some components of the top are worse than others on the subject of mind accidents. As a result of the compartment across the mind stem is comparatively small, Giza mentioned, it takes much less blood to trigger issues there. And fracturing the temporal bone above the ear may sever an artery, inflicting blood to stream quickly into the mind, Marcus mentioned.
Crimson-flag signs
Specialists say the telltale indicators of a critical mind damage are typically adjustments in habits and psychological features. A seizure, paralysis, substantial confusion, a lack of coordination and vomiting are pink flags that ought to ship you straight to the emergency room, Giza mentioned.
Kim-Tenser additionally pointed to feeling disoriented and drifting out and in of lucidity as indications of an actual downside. Marcus added numbness and tingling to the checklist, in addition to feeling torpid or sleepy. “Being drained after a head damage is a nasty signal,” Marcus mentioned.
That’s not essentially a motive to maintain an individual who’s suffered a blow to the top awake all evening, Giza mentioned. However monitoring that particular person is extraordinarily essential, he mentioned, as a result of it’s an indication of a significant issue if neurological or behavioral signs worsen over time.
For instance, delicate complications are widespread after head accidents, in order that they’re not pink flags on their very own. But when they worsen as a substitute of fading after a couple of days, that’s a motive to see your physician.
Marcus famous that generally accidents trigger delayed bleeding, so essential signs might take a couple of days to emerge. That’s very true with older sufferers, he mentioned.
“It isn’t quite common for anyone to hit their head after which to have a critical mind bleed and never have it detected,” Giza mentioned. “However one other threat that may amplify issues is that if anyone is totally alone. Being fully alone is extraordinarily problematic in case your signs begin to worsen.” When you begin to get confused or have reminiscence issues and also you’re by your self, he mentioned, chances are you’ll not acknowledge the scenario you’re in.
As with so many issues in medication, private elements can play an essential position in figuring out whether or not a head trauma ends in critical damage. In response to the Cleveland Clinic, you’re extra inclined to mind bleeding in case you’re older, as a result of the blood vessels round your mind are extra inclined to ripping; in case you’re a hemophiliac or taking blood thinners; in case you play contact sports activities; in case you abuse alcohol, as a result of “broken livers can’t produce sufficient of the proteins that assist the blood to clot;” or in case you’re a child, as a result of your weak neck muscle tissue depart you extra susceptible to move damage.
Different issues to observe for
Even when there are not any red-flag signs, a head damage should still be critical sufficient to warrant calling your physician and being monitored for a couple of days.
Being delicate to gentle or noise, feeling nauseous and having blurred or double imaginative and prescient are all indicators that warrant additional consideration, Giza mentioned. When you misplaced consciousness when the damage occurred, Marcus mentioned, “that’s a regarding symptom associated to the autumn itself.”
A lump on the top might look actually unhealthy, Giza mentioned, however it doesn’t essentially imply there’s an underlying mind damage. The swelling could also be confined to the skin of the cranium. The extra swelling there’s, nevertheless, the tougher it will likely be for a health care provider to really feel for a cranium fracture, he mentioned.
Neither is plenty of bleeding essentially an indication of a mind damage. “A lower to the scalp can bleed fairly impressively,” Giza mentioned, noting that just about 20% of the center’s output will get pumped to the top (primarily for the mind).

Science
What to know about infectious diseases during this holiday season

It’s that time of year, when families and friends come together to share their holiday cheer and a few circulating pathogens.
Peter Chin-Hong, an infectious disease specialist at UC San Francisco, said people should be on the lookout for the “Big Four”: three respiratory viruses currently moving through the U.S. — influenza, COVID-19 and RSV — and one stomach virus — norovirus.
According to WastewaterScan — an infectious disease monitoring network led by researchers at Stanford and Emory universities, with lab-testing partner Verily, Alphabet Inc.’s life sciences organization — those four viruses are running hot around the nation.
In the case of COVID-19, the half of the U.S. east of Montana, Wyoming, Colorado and New Mexico — is trending “high,” while the Western states are still generally low, with some hot spots in major cities such as San Francisco, Seattle, Salt Lake and Boise, according to WastewaterScan.
But that’s likely to change as holiday travel moves those viruses around in what Chin-Hong referred to as “the Great Holiday Equalizer.”
It’s flu, though, that is grabbing most physicians’ and researchers’ attention right now, he said.
While the federal Centers for Disease Control and Prevention‘s outlook for the severity of the flu‘s impact this season was low, Chin-Hong said he saw ominous signs coming from the typical bellwethers for the U.S.: the United Kingdom and South America.
In the UK, there were nearly four times the number of flu cases in early December than they were the same time last year. A similar trend occurred during the winter season in the South American nations of Chile, Ecuador and Uruguay, where hospitalizations were higher than in the 2023 flu season. Elsewhere on the southern continent, seasonal flu rates were fairly typical.
Chin-Hong suspects the CDC’s outlook is based on the assumption that people have some “carryover immunity” from last year, and he said vaccinations help.
But until flu season gets into full swing, it’s difficult to know exactly what it’ll look like and whether the vaccines have the circulating strains fully covered.
Chin-Hong said there are two predominant strains of the virus circulating: H1N1 and H3N2, with the latter virus associated with more severe disease, which may be causing the surges of hospitalizations abroad. But he said this year’s vaccine should cover it.
“It’s never too late” to get vaccinated, he said, noting that flu season in the U.S. is just beginning.
In addition, with the ominous threat of H5N1 bird flu simmering in the background, there is concern that it could mix with a human seasonal flu. Getting vaccinated and keeping the seasonal flu at bay, he said, will decrease the chances for such an occurrence.
Researchers and health officials say there is no evidence that H5N1 can be transmitted between people. But to keep extra safe as the virus moves through the nation’s dairy herds and commercial poultry operations, people should avoid raw milk, raw eggs and undercooked meat. Pasteurization and proper cooking techniques inactivate the virus.
But it’s not only the flu that’s threatening to dampen the nation’s good tidings.
COVID-19, RSV and norovirus are also prevalent.
COVID-19 has recently begun to show up in high levels in municipal wastewater, but Chin-Hong said that doesn’t necessarily mean we’ll see a surge in hospitalizations. Indeed, while the number of COVID cases is ticking up, the CDC predicts there will be fewer cases in the U.S. this year than in 2023.
“Some people think the reason why people are not getting it as much this year is because we got it so recently, particularly in California, and so that carryover immunity is kind of protecting us, at least for the time being,” Chin-Hong said. “The other hypothesis is that we just had enough cycles of it in the population, so maybe it kind of is low this year.”
But, he said, COVID has proven itself a nimble and adaptable virus, continually spawning recombinant variants, so “coupled with low vaccination rates, that’s always the fear with COVID, that it’ll surge back.”
The best things one can do to avoid the three respiratory viruses — influenza, COVID and RSV — is to follow “The three V’s: Vaccinate, ventilate and wash your hands very often,” he said. If you must be indoors or in close proximity to others, masks do make a difference. But try to mingle and cavort outdoors or in well-ventilated areas.
As for norovirus, which causes gastrointestinal distress and typically spreads via items handled by multiple people — such as airplane trays, handrails and buffet serving spoons — washing your hands is key. In addition, keeping your hands away from your face is critical; that’s the primary route of infection.
Chin-Hong said norovirus is seemingly everywhere these days.
“Anecdotally, a lot of colleagues of mine have been out with it,” he said.
In addition, there is some rhinovirus (common cold), pertussis and walking pneumonia circulating, he said.
And of course, he said, if you’re not feeling well, stay home. Nothing stops a virus or contagious bacteria is its tracks like keeping isolated — even if it means missing out on holiday revelries.
Science
Why scientists say we are fighting H5N1 bird flu with one hand tied behind our backs

As the H5N1 bird flu virus steamrolls its way across the globe — killing wild animals, commercial livestock and even some people — scientists and health officials fear we’re on the precipice of another global pandemic.
But when, where and how that could come to pass is hard to predict — in part, some researchers say, because of guardrails the federal government has placed around gain-of-function research.
The term describes experiments that seek to understand a virus’ potential to adapt to new hosts, spread more easily, survive longer in the environment and cause those infected to become sicker. Though many scientists view the approach as a critical tool for conducting biological research, other experts have long complained that it’s unacceptably risky — a reputation exacerbated by persistent speculation that the virus responsible for the COVID-19 pandemic was created in gain-of-function experiments in a laboratory in Wuhan, China.
That led many virologists to steer clear of the work to avoid its stigma and regulatory red tape. Some in the field say that has deprived officials of valuable information that could have helped them anticipate and prepare for H5N1’s next moves.
“Do I believe if that research was more widely accepted, we’d have a better grip on this virus and what it might do next? Or how quickly it could change? Or what that would take?” asked Richard Webby, director of the World Health Organization’s Collaborating Center for Studies on the Ecology of Influenza in Animals and Birds. “YES.”
Felicia Goodrum, a molecular virologist at the University of Arizona, said gain-of-function research could enable health officials to recognize worrisome H5N1 mutations and identify targets for antivirals and vaccines.
“Without it, we’re just flying in the dark,” she said.
Critics of this line of research don’t see it that way. They say the work is too dangerous, making it possible for a souped-up pathogen to escape into the environment where people have no natural immunity. Even worse, they argue, it could wind up in the hands of nefarious actors who could use it as a bioweapon.
These risks outweigh the promise of work that may not be as helpful as its supporters suggest, said Marc Lipsitch, professor of epidemiology at the Harvard T.H. Chan School of Public Health.
What scientists and health officials need to know to contain the outbreak, Lipsitch argues, are things like which animals are infected, which people have been exposed, how many of them caught the virus and how sick they became as a result.
“Those are basic epidemiology and veterinary questions,” Lipsitch said. “I can’t think of any route by which gain-of-function studies could have informed — much less answered — those questions.”
An animal caretaker collects a blood sample from a dairy calf vaccinated against bird flu in Ames, Iowa, in July.
(USDA Agricultural Research Service via Associated Press)
The controversy dates to 2011, when two independent research groups said they had conducted gain-of-function experiments that resulted in strains of H5N1 that could be spread via air between ferrets, a species used to model influenza’s behavior in humans.
H5N1 was first identified in wild geese in China in 1996 and soon spread among birds in Asia, jumping to people on hundreds of occasions along the way. More than half of those known infections were fatal.
The high mortality rate and geographical spread of the virus prompted then-President George W. Bush to establish a $7.1-billion program to prepare for its inevitable arrival on U.S. shores. He spearheaded the establishment of a global surveillance and preparedness network via the WHO, as well as a national one. He also directed federal funds into the stockpile of vaccines and antiviral medications, as well as millions of dollars toward laboratory research.
Amid this flood of support, Yoshihiro Kawaoka‘s team at the University of Wisconsin in Madison and Ron Fouchier‘s at Erasmus University in the Netherlands simultaneously began to experiment with H5N1, introducing genetic mutations into its RNA to see what changes could transform it from a virus that passed easily between birds into one that passed efficiently between people.
Kawaoka and his colleagues combined the H5 hemagglutinin gene from the bird flu virus with genes from the 2009 H1N1 swine flu virus. Then they coaxed their hybrid to evolve in a way that allowed it to bind with mammalian cells rather than bird cells. They found that four mutations in the H5 gene were enough to create a virus capable of spreading between ferrets in neighboring cages.
Meanwhile, the researchers in Fouchier’s lab tinkered solely with H5N1. They added a handful of mutations that helped fuel previous flu pandemics, then infected their ferrets. The virus didn’t spread on its own at first, so the scientists helped it along by transferring it from the noses of infected animals to healthy ferrets. After 10 such passages, the virus had evolved to the point where it spread on its own from one ferret to another.
The studies offered valuable confirmation that the bird flu virus had the potential to spark a human pandemic, said Dr. Arturo Casadevall, an immunologist and infectious disease physician at Johns Hopkins University.
“Before those experiments were done, we did not know whether H5N1 had the biological capacity to become mammalian-transmissible,” he said.
But they also underscored the risk that scientists could accelerate the threat. “That was the original gain-of-function poster child,” Casadevall said.
Concern that information in the studies could be put to ill use prompted Kawaoka and Fouchier to voluntarily pause their work in 2012, and their papers were published only after passing a thorough safety review by the U.S. National Science Advisory Board for Biosecurity. Gain-of-function research resumed the following year.
Fears were revived in 2014 after federal labs mishandled samples of smallpox, anthrax and H5N1. Nobody was sickened, but it prompted a three-year freeze on federal funding for gain-of-function experiments involving particularly dangerous pathogens, until stricter oversight rules were put in place.
Plans for such experiments now go through several layers of review at a potential researcher’s institution. If the work is funded by the National Institutes of Health, additional reviews follow.
“There are a lot of regulatory hurdles to assure there’s appropriate risk mitigation,” said Seema Lakdawala, a virologist at Emory University who studies influenza viruses. “We’re all being extra careful because nobody wants to be accused of having done something unsafe.”

Biohazard suits hang in a Biosafety Level 4 laboratory at the U.S. Army Medical Research Institute of Infectious Diseases at Ft. Detrick, Md.
(Patrick Semansky / Associated Press)
Those hurdles can delay a research project by several months or more, if they are approved at all, she said. The uncertainties have acted as a deterrent, especially for scientists in the early stages of their careers.
“It’s definitely uncomfortable to do gain-of-function research,” Goodrum said. “We’re discouraging people from entering the field.”
To some, the timing couldn’t be worse.
At least 65 people in the U.S. have been infected with H5N1 since it arrived in North America in 2021, according to the Centers for Disease Control and Prevention Most of the cases have involved workers on dairy and poultry farms, and their symptoms — including conjunctivitis and upper respiratory irritation — have tended to be mild. But in two cases, people have become severely ill, including a person in Louisiana and a teenager in Canada.
There is no evidence that the virus can spread directly from one person to another, the CDC said. Scientists expect that will change sooner or later. With flu season picking up steam, the risk is rising.
“The thing I’m most afraid of today is a recombination event between the stuff going around in cows and the seasonal flu,” Casadevall said. If both viruses infected the same mammal at the same time, their components could mix and match in a way that creates “a strain that is able to infect humans very easily, and for which we don’t have immunity.”
“That is a gain-of-function experiment being done by nature,” he added.
It’s a point that Webby suggested as well, noting that gain-of-function experiments are a whole lot safer in a sealed-off Biosafety Level 3 laboratory equipped with special ventilation systems and other precautions “than on a farm.”
But Lipsitch and others say the fact that the virus is constantly mutating and changing calls into question the relevance of gain-of-function research. A viral strain that can be concocted in a laboratory is not necessarily going to match whatever emerges in the environment.
“There’s a big element of randomness in evolution,” Lipsitch said. “The fact that an experiment goes one way in the lab doesn’t mean it will go the same way somewhere else.”

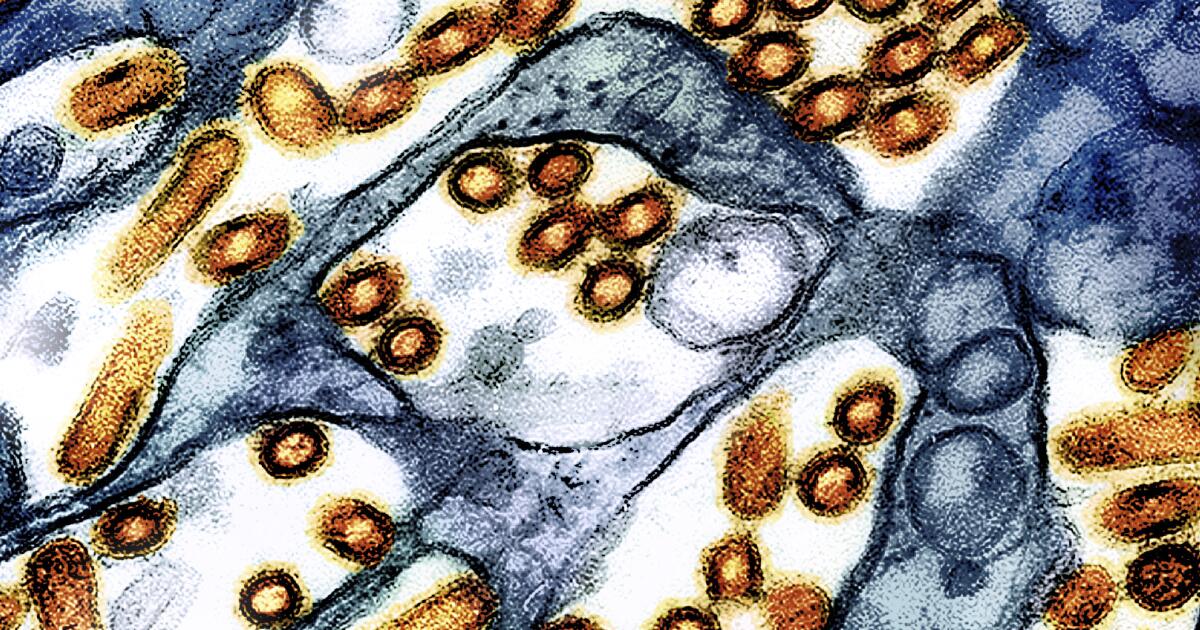
Three rod-shaped H5N1 influenza virus particles are seen in a pair of colorized transmission electron micrographs.
(CDC and NIAID)
Even if it’s a close match, Lipsitch said, there’s “compelling evidence that what you learn in one strain can be the opposite for a very closely related strain. So the generalizability is very low.”
He cited a paper that took the mutations that made H5N1 “more mammal-friendly” in Kawaoka’s and Fouchier’s experiments and applied them to a slightly different version of the virus. In that case, the researchers found “a completely different effect.”
These shortcomings make the research risks harder to justify, said Nicholas Evans, a bioethicist at the University of Massachusetts Lowell.
“I think what the gain-of-function debate has yet to answer is, ‘What is the social value of these studies?’” he said.
To Evans, there appears to be very little, especially considering the lack of urgency in the government’s response.
“Saying that this particular piece of extremely niche biological research into H5N1 would have made a material difference in an outbreak that has largely been characterized by a lack of interest on behalf of public federal agricultural and public health regulators just is kind of nonsense to me,” he said.
Kawoaka declined to discuss his research, and Fouchier could not be reached.
Michael Imperiale, a virologist at the University of Michigan in Ann Arbor, said the experiments conducted by Kawaoka and Fouchier are extremely useful as blueprints of what to watch out for as the virus sweeps the globe. And he’s surprised more people aren’t talking about their value.
“No one seems to point out the fact that those gain-of-function experiments … gave us an important piece of information, which is that that virus can jump,” Imperiale said.
Other gain-of-function experiments conducted on H5N1 years ago have tipped off scientists about potential mutations that could help the real-world virus spread more easily through the air, get better at infecting cells in the mammalian respiratory tract, and become resistant to antiviral medications.
“Those experiments 10 years ago were so informative,” Lakdawala said. “It helped us be better prepared.”
But unless the scientific community stands up for the work and challenges its negative image, that won’t be the case in the future, Goodrum said. “It’s very likely that we will be less prepared for the next pandemic than we were for the last one.”
Science
Gov. Newsom declares emergency in California after CDC confirms severe case of bird flu in Louisiana
Gov. Gavin Newsom declared a state of emergency Wednesday as the H5N1 bird flu virus moved from the Central Valley to Southern California dairy herds, while federal officials confirmed the first U.S. case of severe illness in a hospitalized Louisiana patient — a concerning development as the virus continues to spread throughout the nation via migrating birds.
The declaration by Newsom will allow for a more streamlined approach among state and local agencies to tackle the virus, providing “flexibility around staffing, contracting, and other rules to support California’s evolving response,” according to a statement.
“Building on California’s testing and monitoring system — the largest in the nation — we are committed to further protecting public health, supporting our agriculture industry, and ensuring that Californians have access to accurate, up-to-date information,” Newsom said in the statement. “While the risk to the public remains low, we will continue to take all necessary steps to prevent the spread of this virus.”
According to the U.S. Department of Agriculture, 645 dairy herds in California have reportedly been infected with the H5N1 virus since August. Nationwide, the number is 865 and stretches back to March, when the virus was first detected in Texas herds.
There have also been a number of infections identified in pet cats in California, including three announced on Wednesday.
According to the CDC, 61 people have acquired the virus since March — the vast majority at dairies or commercial poultry operations. Most suffered from mild illness, including conjunctivitis, or pink eye, and upper respiratory irritation.
In California, 34 people have become infected with H5N1, with all but one contracting the virus from infected dairy. The outlier was a child in Alameda County; the source of that infection has not been determined. There was also a suspected case in a child from Marin County who drank raw milk known to be infected with the virus. The CDC was unable to confirm illness in that child.
The case in Louisiana is concerning to public health officials because of its severity. Federal officials would not provide details about the patient’s symptoms, deferring all inquiries to Louisiana’s Department of Public Health.
Emails and calls to that agency went unanswered.
According to CDC officials, the patient was reportedly in close contact with sick and dead birds from a backyard flock on the patient’s property. The virus was a version of the H5N1 bird flu that researchers have labeled D1.1 and is circulating in wild birds.
The strain circulating in dairy cows is known as B3.13.
It was the D1.1 version that was detected in a Canadian teenager hospitalized with severe illness in November. The source for that patient’s infection remains unknown.
According to Demetre Daskalakis, director of the CDC’s National Center for Immunization and Respiratory Diseases, Louisiana health officials and the CDC are investigating the patient’s contacts and performing further genetic analysis of the patient’s virus to determine what, if any, changes may have have occurred.
“These additional laboratory investigations help us to identify concerning changes in the virus, including changes that would signal an increased ability to infect humans, increased ability to be transmitted from person to person, or changes that would indicate that currently available diagnostics, antiviral treatments or candidate vaccine viruses may be less effective,” said Daskalakis in a news conference Wednesday morning.
He said analyses so far have not indicated changes in the virus that would make it “better adapted to infect or spread among humans.”
Analyses of the Canadian teen’s virus showed mutational changes that would make it easier for that version of H5N1 to infect people. However, it is unclear if those changes came prior to the infection — in the wild — or during the course of the child’s infection.
None of the child’s family members or contacts were infected, suggesting the changes occurred in the teenager during the infection and therefore the virus reached a dead end when it was unable to spread beyond the child.
These cases are akin to those recorded historically in Asia and the Middle East, where the H5N1 virus had resulted in a mortality rate of roughly 50%. Since the virus was first identified in 1997, there have been 948 cases reported worldwide leading to 464 deaths.
The cases associated with the B3.13 strain circulating in the nation’s dairy herds have so far resulted in only mild symptoms.
Still, research indicates that changes in at least one viral isolate taken from a dairy worker in Texas had acquired mutational changes that allowed for airborne transmission between mammals, and was 100% lethal in laboratory ferrets.
However, as in the case of the Canadian teen, it is believed that version was unique to the dairy worker and did not spread beyond.
Other research shows that only one mutational change is required for the B3.13 version to pass efficiently between people.
The D1.1 version of the virus “worries me a bit,” said Richard Webby, director of the World Health Organization’s Collaborating Center for Studies on the Ecology of Influenza in Animals and Birds. “Not necessarily because I know it will evolve differently, but it does have a different combination of H5 and N1 which theoretically could help support a different set of mutations” than what researchers have seen in experiments with the B3.13 version.
Daskalakis said the CDC still considers the risk to the general population to be low, and the agency is working to expedite influenza and bird flu testing in clinical and public health laboratories “to help accelerate identification of such cases through its routine influenza surveillance.”
According to Newsom’s office, “California has already established the largest testing and monitoring system in the nation to respond to the outbreak.”
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/24924653/236780_Google_AntiTrust_Trial_Custom_Art_CVirginia__0003_1.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/24924653/236780_Google_AntiTrust_Trial_Custom_Art_CVirginia__0003_1.png) Technology7 days ago
Technology7 days agoGoogle’s counteroffer to the government trying to break it up is unbundling Android apps
-

 News1 week ago
News1 week agoNovo Nordisk shares tumble as weight-loss drug trial data disappoints
-

 Politics1 week ago
Politics1 week agoIllegal immigrant sexually abused child in the U.S. after being removed from the country five times
-

 Entertainment1 week ago
Entertainment1 week ago'It's a little holiday gift': Inside the Weeknd's free Santa Monica show for his biggest fans
-

 Lifestyle1 week ago
Lifestyle1 week agoThink you can't dance? Get up and try these tips in our comic. We dare you!
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25672934/Metaphor_Key_Art_Horizontal.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25672934/Metaphor_Key_Art_Horizontal.png) Technology3 days ago
Technology3 days agoThere’s a reason Metaphor: ReFantanzio’s battle music sounds as cool as it does
-

 Technology1 week ago
Technology1 week agoFox News AI Newsletter: OpenAI responds to Elon Musk's lawsuit
-

 News5 days ago
News5 days agoFrance’s new premier selects Eric Lombard as finance minister


















