Science
Bob Saget’s death calls attention to head injuries. What should you look out for?

The demise of fashionable comic Bob Saget whereas on tour in Florida final month was shocking and tragic, however the damage that claimed his life is extra widespread than you would possibly suppose.
In response to the medical expert in Florida who carried out the post-mortem, Saget most definitely fell and struck the again of his head, inflicting bleeding on his mind. Saget’s household mentioned he in all probability thought nothing of the damage and went to sleep. A lodge worker discovered him useless in mattress the following afternoon.
On a typical day, mind accidents like Saget’s declare the lives of greater than 160 individuals in america, the Facilities for Illness Management and Prevention says. About 61,000 individuals died from a traumatic mind damage, or TBI, within the U.S. in 2019 alone.
Granted, the commonest reason for demise from TBI is a gun-related suicide. Automotive crashes and assaults are different widespread sources of those accidents. However nearly half the hospitalizations from TBI come from the straightforward act of falling down, the CDC says.
Saget was 65, placing him in an age group that’s significantly inclined to damaging falls. A 2006 examine revealed by the Journal of the American Geriatrics Society discovered that “in individuals aged 65 and older, TBI is liable for greater than 80,000 emergency division visits every year; three-quarters of those visits lead to hospitalization because of the damage.” Greater than half of these accidents resulted from falls.
In response to the CDC, “information recommend that some teams are at larger threat of dying from a TBI or experiencing long-term well being issues after the damage.” These teams embody racial and ethnic minorities, members and veterans of the armed companies, homeless individuals, and residents of rural areas.
Everybody hits their head on one thing sooner or later of their lives. So how do you inform when there’s trigger for alarm? Right here’s some recommendation from three specialists on mind accidents: Dr. Christopher C. Giza, director of the UCLA Steve Tisch BrainSport Program; Dr. Could Kim-Tenser, a neurologist with Keck Medication of USC; and Dr. Joshua Marcus, a neurosurgeon at Nuvance Well being in Connecticut.
What causes a traumatic mind damage?
1000’s of People endure traumatic mind accidents yearly, however incidents like those that claimed Saget’s life are uncommon. And though head traumas are “tremendous widespread,” Marcus mentioned, “the overwhelming minority lead to something critical.”
Bumping the headboard as you’re entering into mattress shouldn’t ship you to the hospital. “It must be a reasonably traumatic fall,” Kim-Tenser mentioned. “It actually must be a reasonably arduous hit to the top,” involving a tough influence on a tough floor.
Giza agreed. “Hitting your head on the headboard just isn’t going to create plenty of power,” he mentioned. In contrast, he mentioned, “slipping within the lavatory and hitting your head on the aspect of the bath goes to have appreciable power.”
The mind can be injured in a much less direct manner, when a forceful occasion — a automotive wreck, for instance — shoves it in opposition to the cranium. A shearing damage is when “the mind goes a technique, the power goes the opposite manner,” Marcus mentioned. Then there are contracoup accidents, when a power on one aspect of the top sends the mind into the cranium on the opposite aspect.
The injury is prompted when a blood vessel contained in the cranium ruptures, inflicting blood to pool between the mind and its environment. “The cranium is a closed field, largely,” Giza mentioned, “so in case you begin filling up a part of that house with bleeding, the remainder of the stuff will get squished.”
When you begin squeezing the mind, it doesn’t work very nicely. Folks can go right into a coma or change into paralyzed. And if the strain is utilized to the mind stem (the half close to the spinal wire), it might probably intervene with an individual’s respiratory and heartbeat, Giza mentioned. Past that, he mentioned, the pooled blood irritates the floor of the mind, probably triggering seizures.
Giza and Marcus mentioned that some components of the top are worse than others on the subject of mind accidents. As a result of the compartment across the mind stem is comparatively small, Giza mentioned, it takes much less blood to trigger issues there. And fracturing the temporal bone above the ear may sever an artery, inflicting blood to stream quickly into the mind, Marcus mentioned.
Crimson-flag signs
Specialists say the telltale indicators of a critical mind damage are typically adjustments in habits and psychological features. A seizure, paralysis, substantial confusion, a lack of coordination and vomiting are pink flags that ought to ship you straight to the emergency room, Giza mentioned.
Kim-Tenser additionally pointed to feeling disoriented and drifting out and in of lucidity as indications of an actual downside. Marcus added numbness and tingling to the checklist, in addition to feeling torpid or sleepy. “Being drained after a head damage is a nasty signal,” Marcus mentioned.
That’s not essentially a motive to maintain an individual who’s suffered a blow to the top awake all evening, Giza mentioned. However monitoring that particular person is extraordinarily essential, he mentioned, as a result of it’s an indication of a significant issue if neurological or behavioral signs worsen over time.
For instance, delicate complications are widespread after head accidents, in order that they’re not pink flags on their very own. But when they worsen as a substitute of fading after a couple of days, that’s a motive to see your physician.
Marcus famous that generally accidents trigger delayed bleeding, so essential signs might take a couple of days to emerge. That’s very true with older sufferers, he mentioned.
“It isn’t quite common for anyone to hit their head after which to have a critical mind bleed and never have it detected,” Giza mentioned. “However one other threat that may amplify issues is that if anyone is totally alone. Being fully alone is extraordinarily problematic in case your signs begin to worsen.” When you begin to get confused or have reminiscence issues and also you’re by your self, he mentioned, chances are you’ll not acknowledge the scenario you’re in.
As with so many issues in medication, private elements can play an essential position in figuring out whether or not a head trauma ends in critical damage. In response to the Cleveland Clinic, you’re extra inclined to mind bleeding in case you’re older, as a result of the blood vessels round your mind are extra inclined to ripping; in case you’re a hemophiliac or taking blood thinners; in case you play contact sports activities; in case you abuse alcohol, as a result of “broken livers can’t produce sufficient of the proteins that assist the blood to clot;” or in case you’re a child, as a result of your weak neck muscle tissue depart you extra susceptible to move damage.
Different issues to observe for
Even when there are not any red-flag signs, a head damage should still be critical sufficient to warrant calling your physician and being monitored for a couple of days.
Being delicate to gentle or noise, feeling nauseous and having blurred or double imaginative and prescient are all indicators that warrant additional consideration, Giza mentioned. When you misplaced consciousness when the damage occurred, Marcus mentioned, “that’s a regarding symptom associated to the autumn itself.”
A lump on the top might look actually unhealthy, Giza mentioned, however it doesn’t essentially imply there’s an underlying mind damage. The swelling could also be confined to the skin of the cranium. The extra swelling there’s, nevertheless, the tougher it will likely be for a health care provider to really feel for a cranium fracture, he mentioned.
Neither is plenty of bleeding essentially an indication of a mind damage. “A lower to the scalp can bleed fairly impressively,” Giza mentioned, noting that just about 20% of the center’s output will get pumped to the top (primarily for the mind).

Science
If you're living with a drug or mental health problem, here's where to look for help

Fatal overdoses in the U.S. fell for the first time in five years in 2023, according to preliminary estimates recently released by the Centers for Disease Control and Prevention, but UCLA researcher Joseph Friedman warns that the new findings should not be interpreted to mean that the nation’s drug and mental health crises are abating.
Friedman has analyzed “deaths of despair” that result from overdose, suicide and liver disease due to alcoholism and found that while death rates for white Americans have dipped, rates have risen in recent years among people of color in the U.S., especially among Native and Black Americans. Illegal opioids such as fentanyl have ravaged Black and low-income communities in Los Angeles.
While it’s difficult to pinpoint the exact reasons behind substance abuse or suicide, Friedman as well as other experts in addiction medicine and mental health say racial inequality, economic distress and historical trauma have aggravated those problems in marginalized communities.
If you or someone you know needs immediate help for a mental health, substance-use or suicidal crisis, call or text 988, or chat online by visiting the suicide and crisis line’s website. For mental health resources and referrals, call the Los Angeles County Department of Mental Health’s Help Line 24/7 at (800) 854-7771.
Here are other organizations that offer information, counseling and support services:
Nakeya Fields, a licensed clinical social worker in Pasadena, founded the Black Mental Health Task Force, a coalition that brings together mental health professionals, clients, nonprofits, community organizations, educators and others in California to raise awareness about mental wellness. Her Therapeutic Play Foundation offers activities designed to improve resilience and coping skills through creative arts, play and sports. It provides individual, couples, group and family therapy for Black, Latinx, LGBTQ+ and other members of marginalized populations.
The American Indian Counseling Center, a division of the Los Angeles County Mental Health Department, offers crisis intervention, 24/7 intensive mental health services and counseling for all ages, as well as physician consultations for medications and referrals to culturally relevant support groups. Call (562) 402-0677 and ask to speak with the on-duty worker.
United American Indian Involvement’s behavioral health program provides outpatient substance use disorder treatment and mental health services to American Indians and Alaska Natives living throughout Los Angeles County. Visit the website or call (213) 202-3970.
Melanin and Mental Health offers an online network of Black and brown mental healthcare providers that is searchable by geographic area, issue type and treatment sought. It’s also possible to filter results by therapists’ racial background and specialty, as well as by insurance carrier.
The Black Mental Health Alliance offers confidential referrals to culturally competent mental health professionals who are in its database of licensed therapists.
Painted Brain advocates for mental wellness in underserved L.A. communities by offering self-care, relaxation and therapeutic art and play sessions, support groups and trainings for mental health professionals. As part of its peer-led model, many of the staff have experienced mental health issues themselves. Its community center and art space is located at 5980 W. Pico Blvd. in Los Angeles.
The Los Angeles LGBT Center offers individual, couples, family, group therapy and psychiatric care, as well as support for people struggling with substance use. The center has locations in West Hollywood, at Mi Centro in East L.A., at its Trans Wellness Center near MacArthur Park and in South L.A.’s Leimert Park neighborhood.
The Community Health Project Los Angeles provides services to people who use drugs by way of a harm-reduction approach that emphasizes offering clean needles as well as education on how to respond to an overdose.
Science
Are 'deaths of despair' really more common for white Americans? A UCLA report says no

Nakeya Fields has seen how the stresses that come with being Black — racial injustice, financial strain, social isolation — can leave people feeling hopeless and push some into substance abuse.
It’s one of the reasons the Pasadena social worker started offering “therapeutic play” gatherings for Black mothers like herself and children.
“I’m trying to host more safe spaces for us to come and share that we’re suffering,” the 32-year-old said. “And honestly, the adults need play more than kids.”
Yet while Black and brown mental health practitioners such as Fields have labored to address these issues within their communities, a very different conversation has been occurring in the nation at large.
For years, discussions about America’s substance-abuse crisis have focused almost exclusively on the narrative that it is white, middle-age adults who face the greatest risk of dying from drug overdoses, alcoholic liver disease and suicide.
The theory, which was presented by two Princeton economists in 2015 and based on data from 1999 to 2013, argued that despair was behind rising premature mortality rates among white Americans, especially those who were less educated.
Virtually overnight, the “deaths of despair” concept began to drive the national discourse over populist far-right politics; the rise of Donald Trump; and deepening political polarization over such topics as addiction treatment, law enforcement and immigration.
But after roughly a decade, researchers at UCLA and elsewhere have begun to dismantle this idea.
In a study published recently in the journal JAMA Psychiatry, authors found that deaths of despair rates for middle-age Black and Native Americans have surged past those of white Americans as the overdose crisis moves from being driven by prescription opioids to illegal drugs such as fentanyl and heroin.
While the opioid crisis did raise drug overdose deaths among white Americans for a time, it was an anomaly, said Joseph Friedman, a social medicine expert at UCLA’s David Geffen School of Medicine who was the lead author of the journal analysis. In fact, by 2022 the rate for white Americans had started to dip.
“What’s really important is that now, with these three causes of death, the gap has closed, and it’s moving in the other direction,” Friedman said.
Sandra Mims, a community health worker with Community Health Project L.A., puts out boxes of Narcan — a naloxone nasal spray that reverses the effects of opioid overdose — at an event at MacArthur Park in Los Angeles on International Overdose Awareness Day.
(Mel Melcon / Los Angeles Times)
The analysis found that deaths of despair for Black Americans hit a rate of 103.81 per 100,000 people in 2022, compared with 102.63 for white Americans. The rate for Native American and Alaska Native populations was even higher at 241.7 per 100,000 people in 2022.
The UCLA analysis doesn’t specify the midlife personal issues that might have led to addiction or suicide.
But the authors say that flaws in the methodology of the 2015 deaths of despair report skewed its conclusions about who was most at risk. Specifically, Friedman said that it failed to give enough consideration to long-standing racial inequities that Black Americans experience in income, educational attainment, incarceration and access to quality medical care, all of which can contribute to drug use and poor mental health outcomes. And statistics for Native Americans weren’t factored in at all.
“It was burned into the American psyche that it was white people in the rural U.S.,” Friedman said. “It was just a very small piece of the truth that was very interesting but was widely sold as something it wasn’t.”
Another recent worrying sign, Friedman says: Deaths of despair among Latinos are starting to catch up to those among Black and Native Americans.
Princeton professors Anne Case and her husband Angus Deaton, winner of the 2015 Nobel Prize in economic sciences, were thrust into the media spotlight when their deaths of despair findings were first published. Deaton told NPR that during a visit to the White House, even President Obama asked him about the phenomenon.
Their 2020 book, “Deaths of Despair and the Future of Capitalism,” was described by publisher Princeton University Press as “a troubling portrait of the American dream in decline.”
“For the white working class, today’s America has become a land of broken families and few prospects. As the college educated become healthier and wealthier, adults without a degree are literally dying from pain and despair,” the publisher said.
Fields, who employs yoga and pottery in her therapy, said this framing was misleading and racially biased.
“I’m actually flabbergasted that somebody has a term called ‘deaths of despair,’” Fields said. “It’s ‘despair’ when white people experience this suffering. But when we experience it, it’s just what we have to deal with.”

Nakeya Fields says it’s important to address mental wellness issues early, before people reach a crisis point and become another statistic.
(Jason Armond / Los Angeles Times)
Both Friedman and Fields say their critiques are not intended to minimize deaths among white Americans.
Still, Friedman wonders: “How do we empower Black and Native American communities in a way that enables them to treat these problems?”
Racism must be considered when trying to make sense of the crisis in premature deaths, says Dr. Helena Hansen, head of UCLA’s Department of Psychiatry and a senior author on Friedman’s analysis. Hansen, who is Black and specializes in addiction psychiatry, also co-authored the book “Whiteout: How Racial Capitalism Changed the Color of Opioids in America.”
For years, pharmaceutical companies steered expensive prescription pain medications, such as the opioid Oxycontin, as well as the most effective medications for opioid-use disorder, to white Americans with good access to healthcare, she said.
But at the same time, Black and brown Americans were unfairly subjected to law enforcement policies that prioritized incarceration for illegal drug use over increasing access to more humane medical strategies to help them, further harming already vulnerable communities, Hansen said.
“In our society, people with access to the new technologies and pharmaceuticals are more likely to be white,” Hansen says. “None of this is by accident. All of this is the direct result of careful racially and class-segmented marketing strategies by pharmaceutical companies.”
This two-tiered system arose because drug manufacturers, doctors and policymakers have for too long failed to see people from historically marginalized communities who live with addiction and mental health crises as worthy of the same sympathy and treatments that many white Americans receive, Hansen says.
Joseph Gone, a professor of anthropology at Harvard who has spent 25 years studying the intersection of colonialism, culture and mental health in Indigenous communities, agreed.
“Deaths of despair have been a reality for Indigenous communities since conquest and dispossession,” he said.
“It’s amazing how much grief our people contend with from early deaths — there are not that many communities in America that bear it quite the way we do,” said Gone, who is a member of the Aaniiih-Gros Ventre tribal nation of north-central Montana. “Until we acknowledge and take responsibility for the casualties of colonization, which endure to this day through deaths of despair, it’s going to be very hard to turn this around.”
Gone, who has collaborated with Friedman on previous research, says the mental health crisis in tribal nations is aggravated by widespread joblessness and generational poverty, and a lack of healthcare resources to treat people in need of immediate or long-term treatment.
Just one traveling psychiatrist serves reservations spread across both Montana and Wyoming — a region covering more than 243,300 square miles — mostly to manage patients’ prescriptions, he says.
And “for all of Indian country, we’re talking about a very small number of in-patient psychiatric facilities,” Gone says.
General practitioners can serve as a first line of defense, but they are not necessarily equipped to address the ongoing life crises that can lead to excessive drug and alcohol use, Gone says.
Fields says it’s important to address mental wellness issues early, before people reach a crisis point and become another statistic.
While her focus remains on Black women, she’s developed additional programming for adults, families and children, such as developmental screenings that measure for high stress levels. In June, Fields will co-present “Rap 4 Peace,” a conference and gala featuring hip-hop artists talking about mental health and reducing gun violence.
“This ‘tragedy of despair’ lives in us,” Fields says. “We breathe it. We go outside hoping that nobody will harm us or our children because they feel threatened by us. This is truly harmful to our bodies.”
Science
SpaceX plans to launch 90 rockets from Vandenberg Space Force Base by 2026. Could that harm the coast?

SpaceX plans to launch 90 rockets into space from a Santa Barbara County military base by 2026, tripling the number of blasts rocking the coastal community — and raising concerns from neighbors and environmental groups about the effects on marine life.
Founded by billionaire Elon Musk, SpaceX has ramped up the number of rocket launches from Vandenberg Space Force Base in recent years, and it has made clear its desire to increase the frequency of blastoffs. But during a California Coastal Commission hearing Friday, U.S. Space Force officials outlined for the first time its own plans to multiply the number of launches from the base, from 37 in 2023 to more than 120 a year by 2026.
The overwhelming majority of those rocket liftoffs would be conducted by SpaceX, which has already done more launches from the base than the commission has approved.
Last year SpaceX breached an agreement with the commission that limited the number of launches to six, sending 28 rockets into space.
It is seeking an agreement with the commission to do 36 launches a year, increasing to 90 in 2026.
The decision by the commission, which was created to protect the state’s coastal resources, will directly affect residents and marine life near the military base that hear and feel the rockets’ sonic booms.
It could also redirect the future of SpaceX, whose pursuit to redefine space exploration is already closely tied with U.S. military interests, given its work as a military contractor.
“The ultimate goal is for this to be more routine and not a huge deal,” said Space Force Col. Bryan Titus, operations vice commander at the base.
Formed in 2019, the U.S. Space Force has been looking to improve its ability to send rockets into space, Titus said, so SpaceX’s ability to launch with more frequency is a benefit to the U.S. military.
SpaceX launched 96 rockets in 2023 from Vandenberg and three other facilities: Cape Canaveral Space Force Station in Florida, NASA’s Kennedy Space Center in Merritt Island, Fla., and SpaceX Starbase in Boca Chica, Texas.
Environmental groups argue that turning launches into a routine event could affect marine life.
“We’re concerned that more frequent launches will result in permanent changes,” said Ana Citrin, legal and policy director for the Gaviota Coast Conservancy.
Federal agencies, including the U.S. Fish and Wildlife Service and National Marine Fisheries Service, monitor the effects of the liftoffs on such animals as sea otters, bats, western snowy plovers, California least terns and California red-legged frogs.
Thus far, the monitoring has shown that some of the animals might react to the blastoff by flushing, or fleeing from their nests and homes, but they return soon after, according to U.S. Space Force officials. No long-term effects have been seen, they said.
SpaceX did not respond to a request for comment.
Flushing or hunkering down after a blast are already signs of wildlife exhibiting signs of stress, said Duncan Leitch, a professor of integrative biology at UCLA.
Most animals can adapt to infrequent incidents, but exposure to more frequent stressful incidents can change their biology as well as their behavior, he said.
In the worst-case scenarios, he said, the ability of birds to communicate could be impeded, and migratory birds could avoid the area. Fish and other animals that use sound to communicate and navigate underwater — including whales — could be affected too.
“Over a longer period of time, there may be reductions in the population of fish as they move away from the sound, or they may be affected to the point that it affects their health,” Leitch said. “It would change the ecosystem as far as other animals that rely on the fish.
“Having sounds that are well into the damaging, or painful, range of decibels now occurring [100] times a year, the animals might not have the ability to change their behavior or accommodate these types of sounds.”
Some environmental groups, including the Surfrider Foundation, are asking the commission to reject the increase.
SpaceX “intends to begin increasing very rapidly, so we’re very concerned about this,” said Mandy Sackett, senior California policy coordinator for the Surfrider Foundation.
More frequent launches could change the way wildlife in the area responds in the long term, environmental groups said.
Members of the California Coastal Commission are also asking whether SpaceX should be entitled to circumvent the permit process, as federal agencies are.
Federal entities negotiate agreements with the commission but ultimately can move ahead even without commission approval. In such cases, the commission’s recourse would be through mediation or the courts.
Because SpaceX is a U.S. Space Force contractor, military officials argue that all launch operations at the base by the company are “federal activities.”
But U.S. Space Force officials said only 25% of the rockets launched into space by SpaceX are carrying payloads for the Department of the Defense.
The vast majority of the liftoffs are for the company’s private benefit, raising questions about why SpaceX can dispense with permits when 75% of its blasts from the base don’t involve the U.S. government.
“That is still pretty skewed for me,” Commissioner Mike Wilson said during a meeting Friday.
Some commissioners — whose focus is usually on environmental protection, development and water issues during their monthly meetings — also brought up the war in Ukraine during Friday’s discussion.
“I question the national security public benefit of concentrating that much power, literally communication power, in one company that we’re enabling in this case,” Wilson said. “[SpaceX] has already showed that it will play in international conflicts at the will of one human being.”
Wilson was referring to reports that Musk’s company refused to allow Ukraine to use satellite internet service from Starlink, a subsidiary of SpaceX, to help it carry out an attack against Russia in September 2022.
“If the idea is that we’re supporting these permits on the side that we’re promoting national defense, and then a single company is able to dismantle our allies during armed conflict — that really doesn’t align,” Commissioner Justin Cummings said.
“I suspect that would violate our strategies around national defense.”
Titus declined to address the question, saying it was “out of my lane,” but he said he would try to get answers to address the commissioners’ concerns.
Some commissioners on Friday also argued that SpaceX, not U.S. military officials, should be making the company’s case in front of the agency.
“When this comes back, I think it would be really important that a representative from SpaceX comes to the meeting,” Cummings said.
Cummings said it was “ridiculous” for SpaceX not to appear at the meeting, despite multiple efforts from the agency to have SpaceX officials speak.
“They obviously refuse to because they’ve never shown up,” he said.
On Friday, Commission Chair Caryl Hart suggested an agreement might not be possible unless SpaceX changes its stance.
“From my perspective,” Hart said, “I think we’re going to continue to hit significant obstacles in achieving a federal consistency ruling without having SpaceX.”
-

 News1 week ago
News1 week agoSkeletal remains found almost 40 years ago identified as woman who disappeared in 1968
-

 World1 week ago
World1 week agoIndia Lok Sabha election 2024 Phase 4: Who votes and what’s at stake?
-

 World1 week ago
World1 week agoUkraine’s military chief admits ‘difficult situation’ in Kharkiv region
-

 Movie Reviews1 week ago
Movie Reviews1 week agoAavesham Movie Review
-

 World1 week ago
World1 week agoCatalans vote in crucial regional election for the separatist movement
-

 News1 week ago
News1 week agoTrump, Reciting Songs And Praising Cannibals, Draws Yawns And Raises Eyebrows
-

 Movie Reviews1 week ago
Movie Reviews1 week agoUnfrosted Movie Review: A sweet origins film which borders on the saccharine
-
 Politics1 week ago
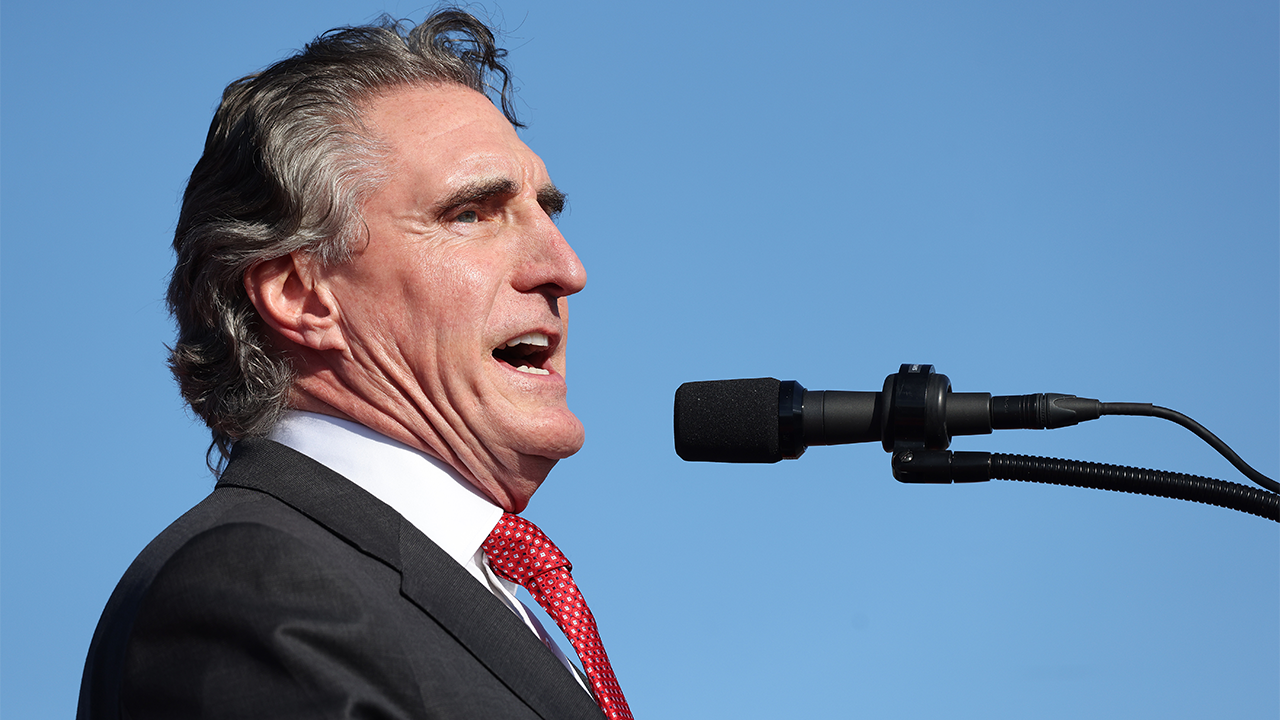
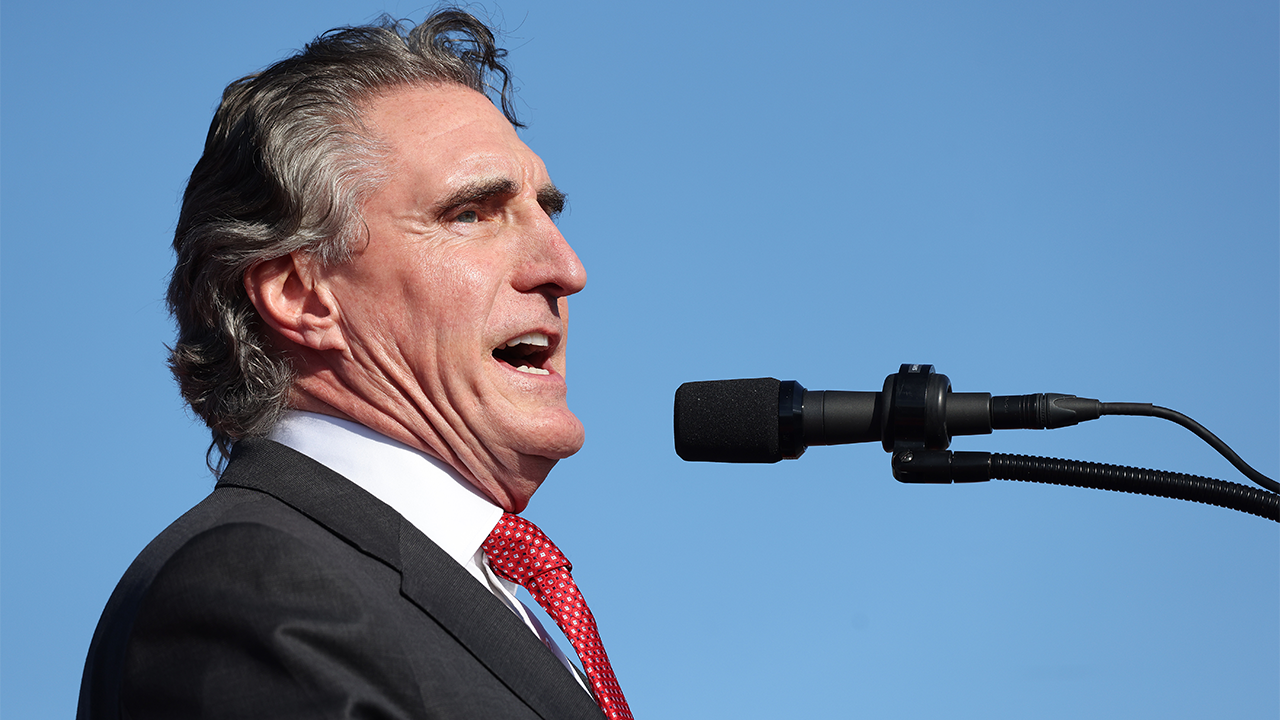
Politics1 week agoNorth Dakota gov, former presidential candidate Doug Burgum front and center at Trump New Jersey rally















