Health
Texas man dies after raw oyster dinner linked to bacteria in shellfish

A man who consumed raw oysters at a restaurant in Texas died days later from a bacterial infection, health officials said.
According to Galveston County Local Health Authority Dr. Philip Keiser, the latest victim of the shellfish bacteria infection was a man in his 30s from Galveston with underlying health issues.
“He had problems with his liver. He also had some other problems, and he had to take some medication that suppressed his immune system,” Dr. Keiser told FOX 26. “It just so happens that the conditions that he had really predisposed him to an overwhelming infection with Vibrio vulnificus.”
A basket of oysters. (AP Photo/Mark Lennihan/File)
Officials said that he consumed several raw oysters from a restaurant Aug. 29, and was admitted to the hospital Aug. 31. He died over Labor Day weekend.
Officials have not released the man’s identity or the name of the restaurant, but said investigators are working to identify the source of the bacteria.
FLORIDA OFFICIALS REPORT FIVE DEATHS FROM ‘FLESH-EATING’ BACTERIA IN TAMPA BAY SINCE JANUARY
“We’ve actually gone to the restaurant where he was eating, and we pulled the oysters from the shelf. There are tags to them, so we can identify the lots, and the state is actually analyzing them to see if we can find the bug in a particular lot of oysters,” Keiser said.
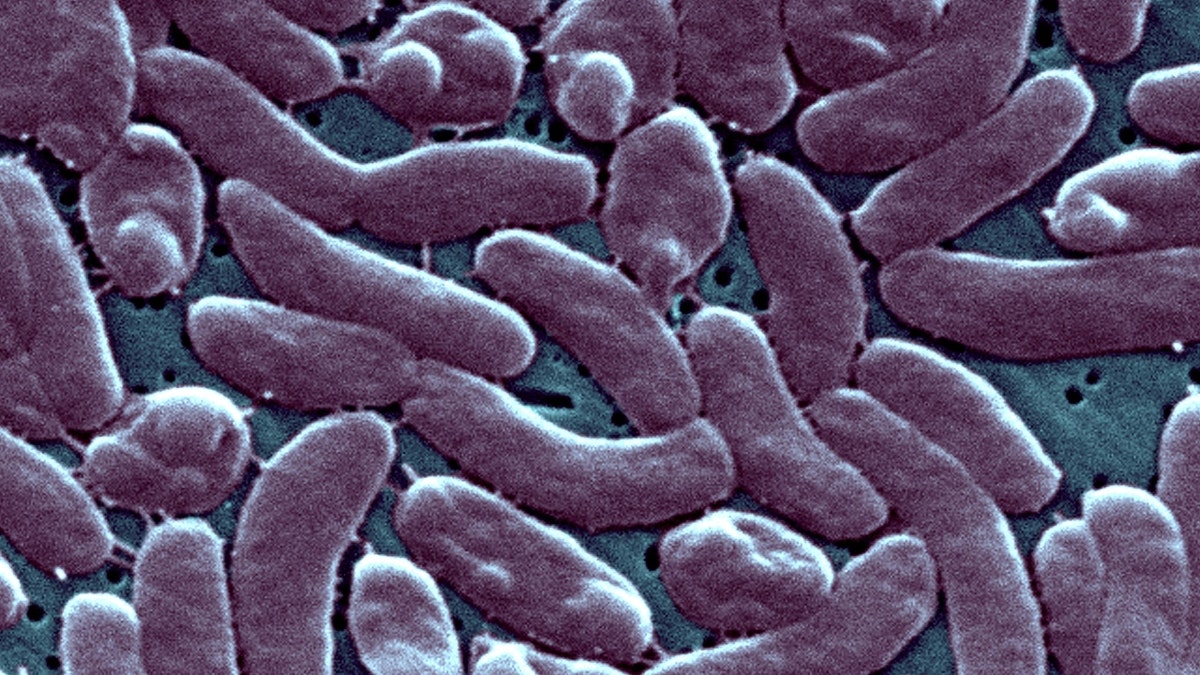
Vibriosis causes an estimated 80,000 illnesses and 100 deaths in the U.S. every year, according to the Centers for Disease Control and Prevention. (Photo By BSIP/Universal Images Group via Getty Images/File)
Vibriosis, the disease caused by the bacteria, can cause nausea, vomiting, chills, cramping, and fever. Death traditionally only occurs in people with a weakened immune system, but the bacterium is still responsible for 95% of seafood related deaths and has a mortality rate of 33%.
CONNECTICUT RESIDENTS DIE AFTER SHELLFISH BACTERIA INFECTION
The bacterium is traditionally found in warm waters during the summer months and is not transferable from person to person. Infected people typically begin to experience symptoms 12 to 72 hours after consumption and symptoms tend to come on quickly.

Woman tasting fresh raw oyster shellfish and drinking wine in seafood restaurant. (iStock)
The Centers for Disease Control and Prevention advises reducing your chances of contracting Vibriosis by; not consuming raw shellfish or food in contact with raw shellfish, do not swim in brackish water with open cuts and to thoroughly wash your hands before and after preparing shellfish.
The CDC has reported that nearly 80,000 people get vibriosis in the U.S. each year, and about 100 people die from it.
Fox News Digital’s Matteo Cina contributed to this report.

Health
FDA bans red food dye due to potential cancer risk

FDA looks to ban red food dye
Celebrity fitness trainer Jillian Michaels joins ‘Hannity’ to discuss the possibility of the FDA banning red food dye.
The U.S. Food and Drug Administration (FDA) has officially banned red dye — called Red 3, or Erythrosine — from foods, dietary supplements and ingested medicines, as reported by the Associated Press on Wednesday.
Food manufacturers must remove the dye from their products by January 2027, while drug manufacturers will have until January 2028 to do so, AP stated.
Any foods imported into the U.S. from other countries will also be subject to the new regulation.
RED FOOD DYE COULD SOON BE BANNED AS FDA REVIEWS PETITION
“The FDA is taking action that will remove the authorization for the use of FD&C Red No. 3 in food and ingested drugs,” said Jim Jones, the FDA’s deputy commissioner for human foods, in a statement.
The U.S. Food and Drug Administration has officially banned red dye — called Red 3, or Erythrosine — from foods, dietary supplements and ingested medicines (iStock)
“Evidence shows cancer in laboratory male rats exposed to high levels of FD&C Red No.3,” he continued. “Importantly, the way that FD&C Red No. 3 causes cancer in male rats does not occur in humans.”
The synthetic dye, which is made from petroleum, is used as a color additive in food and ingested drugs to give them a “bright cherry-red color,” according to an online statement from the FDA.

Food manufacturers must remove the dye from their products by January 2027, while drug manufacturers will have until January 2028 to do so. (iStock)
The petition to ban the dye cited the Delaney Clause, which states that the agency cannot classify a color additive as safe if it has been found to induce cancer in humans or animals.
The dye was removed from cosmetics nearly 35 years ago due to potential cancer risk.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“This is a welcome, but long overdue, action from the FDA: removing the unsustainable double standard in which Red 3 was banned from lipstick but permitted in candy,” said Dr. Peter Lurie, director of the group Center for Science in the Public Interest, which led the petition effort, as reported by AP.

Nearly 3,000 foods are shown to contain Red No. 3, according to Food Scores, a database of foods compiled by the Environmental Working Group. (iStock)
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Health and Fox News senior medical analyst, applauded the FDA’s ban.
“It was a long time coming,” he told Fox News Digital. “It’s been more than 30 years since it was banned from cosmetics in the U.S. due to evidence that it is carcinogenic in high doses in lab rats. There needs to be a consistency between what we put on our skin and what we put into our mouths.”
“There needs to be a consistency between what we put on our skin and what we put into our mouths.”
Siegel said he believes the FDA’s decision could be tied to the incoming new head of the Department of Health and Human Services, Robert F. Kennedy Jr.
“They knew it would have happened anyway under RFK Jr.,” he said. “It is already banned or severely restricted in Australia, Japan and the European Union.”

The food additive also “drew kids in” to a diet of empty calories and ultraprocessed foods, one doctor stated. (iStock)
The food additive also “drew kids in” to a diet of empty calories and ultraprocessed foods, Siegel added.
“It has also been linked to behavioral issues in children, including ADHD.”
Nearly 3,000 foods are shown to contain Red No. 3, according to Food Scores, a database of foods compiled by the Environmental Working Group.
For more Health articles, visit www.foxnews.com/health
The National Confectioners Association provided the below statement to Fox News Digital.
“Food safety is the number one priority for U.S. confectionery companies, and we will continue to follow and comply with FDA’s guidance and safety standards.”
The petition to remove Red No. 3 from foods, supplements and medications was presented in 2022 by the Center for Science in the Public Interest and 23 other organizations and scientists.
Health
How Yvette Nicole Brown Lost Weight and Got Her Diabetes Under Control

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
As bird flu spreads, CDC recommends faster 'subtyping' to catch more cases

As cases of H5N1, also known as avian flu or bird flu, continue to surface across the U.S., safety precautions are ramping up.
The U.S. Centers for Disease Control and Prevention (CDC) announced on Thursday its recommendation to test hospitalized influenza A patients more quickly and thoroughly to distinguish between seasonal flu and bird flu.
The accelerated “subtyping” of flu A in hospitalized patients is in response to “sporadic human infections” of avian flu, the CDC wrote in a press release.
ONE STATE LEADS COUNTRY IN HUMAN BIRD FLU WITH NEARLY 40 CONFIRMED CASES
“CDC is recommending a shortened timeline for subtyping all influenza A specimens among hospitalized patients and increasing efforts at clinical laboratories to identify non-seasonal influenza,” the agency wrote.
The CDC now recommends accelerated subtyping of influenza A in response to “sporadic human infections” in the U.S. (iStock)
“Clinicians and laboratorians are reminded to test for influenza in patients with suspected influenza and, going forward, to now expedite the subtyping of influenza A-positive specimens from hospitalized patients, particularly those in an intensive care unit (ICU).”
LOUISIANA REPORTS FIRST BIRD FLU-RELATED HUMAN DEATH IN US
The goal is to prevent delays in identifying bird flu infections and promote better patient care, “timely infection control” and case investigation, the agency stated.
These delays are more likely to occur during the flu season due to high patient volumes, according to the CDC.
For more Health articles, visit www.foxnews.com/health
Health care systems are expected to use tests that identify seasonal influenza A as a subtype – so if a test comes back positive for influenza A but negative for seasonal influenza, that is an indicator that the detected virus might be novel.

Identifying bird flu infections will support better patient care and infection control, the CDC says. (iStock)
“Subtyping is especially important in people who have a history of relevant exposure to wild or domestic animals [that are] infected or possibly infected with avian influenza A (H5N1) viruses,” the CDC wrote.
In an HHS media briefing on Thursday, the CDC confirmed that the public risk for avian flu is still low, but is being closely monitored.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The agency spokesperson clarified that this accelerated testing is not due to bird flu cases being missed, as the CDC noted in its press release that those hospitalized with influenza A “probably have seasonal influenza.”
Niels Riedemann, MD, PhD, CEO and founder of InflaRx, a German biotechnology company, said that understanding these subtypes is an “important step” in better preparing for “any potential outbreak of concerning variants.”

The CDC recommends avoiding direct contact with wild birds or other animals that may be infected. (iStock)
“It will also be important to foster research and development of therapeutics, including those addressing the patient’s inflammatory immune response to these types of viruses – as this has been shown to cause organ injury and death during the COVID pandemic,” he told Fox News Digital.
Since 2022, there have been 67 total human cases of bird flu, according to the CDC, with 66 of those occurring in 2024.
The CDC recommends that people avoid direct contact with wild birds or other animals that are suspected to be infected. Those who work closely with animals should also wear the proper personal protective equipment (PPE).
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology1 week ago
Technology1 week agoMeta is highlighting a splintering global approach to online speech
-

 Science6 days ago
Science6 days agoMetro will offer free rides in L.A. through Sunday due to fires
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology1 week ago
Technology1 week agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 News1 week ago
News1 week agoPhotos: Pacific Palisades Wildfire Engulfs Homes in an L.A. Neighborhood
-

 Education1 week ago
Education1 week agoFour Fraternity Members Charged After a Pledge Is Set on Fire
-

 Politics1 week ago
Politics1 week agoTrump trolls Canada again, shares map with country as part of US: 'Oh Canada!'
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg) Technology6 days ago
Technology6 days agoAmazon Prime will shut down its clothing try-on program
-

 News1 week ago
News1 week agoMapping the Damage From the Palisades Fire













