Health
Respiratory virus spiked as COVID, RSV cases fell, agency data shows

Health officials reported that cases of human metapneumovirus (HMPV) spiked this spring as COVID-19 and Respiratory Syncytial Virus cases fell.
National data from the Centers for Disease Control and Prevention shows circulating strains of coronavirus on a downward trend as temperatures have warmed.
In addition, both detections and percent positive respiratory syncytial virus tests in the U.S. have plummeted since late last year.
Agency data also showed nearly 11% of PCR tests and more than 19% of antigen tests for HMPV were positive in the U.S. in March.
US RESEARCH FINDS 1 IN 10 ADULTS GET LONG COVID AFTER OMICRON
Symptoms include cough, fever, nasal congestion and shortness of breath. (istock)
The CDC says symptoms of the respiratory virus commonly include cough, fever, nasal congestion and shortness of breath.
However, clinical symptoms of infection may progress to bronchitis or pneumonia.
It can take anywhere from three to six days for incubation, and the average duration of illness is largely similar to other respiratory infections caused by viruses.
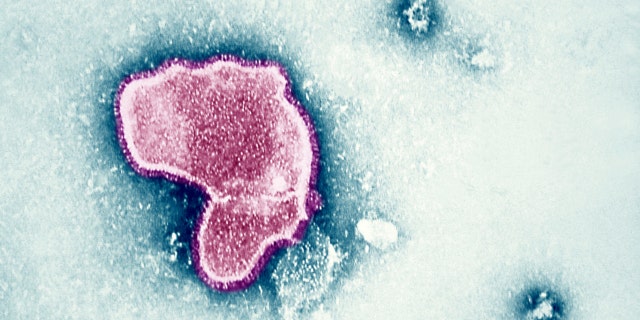
An electron micrograph reveals the morphologic traits of the Respiratory Syncytial Virus. (Photo By BSIP/UIG Via Getty Images)
HMPV can cause both upper and lower respiratory disease in people of all ages, especially among young children, older adults and those with weakened immune systems.
WHO CHIEF WARNS OF FUTURE PATHOGENS WITH ‘EVEN DEADLIER POTENTIAL’ THAN COVID-19
Discovered in 2001, HMPV is in the Pneumoviridae family, as well as RSV.
It is spread by coughs and sneezing, close personal contact and touching infected surfaces and then touching the mouth, nose or eyes.

A young woman blows her nose. (iStock)
There is currently no specific antiviral therapy to treat HMPV and no vaccine to prevent infection.
People can prevent the spread by avoiding close contact with those who are sick, not touching their eyes, noses or mouths with unwashed hands and by washing their hands often with soap and water for at least 20 seconds.
In addition, cleaning possible contaminated surfaces may potentially help stop the spread. Medical professionals should consider testing for it in the winter and spring, especially when HMPV is commonly circulating.

Health
Horoscope: What’s in Store for You May 20 — May 26, 2024?

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Disrupted sleep, plus nightmares could be linked to autoimmune diseases, experts say

Those who experience vivid nightmares and odd hallucinations might have an underlying autoimmune disease, a new study suggests.
An international research team led by scientists at the University of Cambridge and King’s College London explored the potential link between nightmares and hallucinations and systemic autoimmune rheumatic diseases.
The study, published in March in the journal eClinicalMedicine, included 676 people with lupus and 400 people from the medical field, as well as interviews with 69 people living with systemic autoimmune rheumatic diseases, SWNS reported.
STRUGGLING TO FALL ASLEEP? TRY THIS SIMPLE TRICK TO DRIFT OFF QUICKLY
Those with autoimmune diseases were asked about the timing of their neurological and mental health symptoms, such as disrupted sleep, hallucinations, depression and loss of balance.
Of the 29 symptoms listed, the participants were asked to rank such symptoms in the order in which they occurred relative to their disease flare-ups.
The study looked at not only the issues surrounding sleep, but also when the issues for participants began. (iStock)
The study found that three in five people experienced “vivid” and “distressing” nightmares that involved being trapped, attacked or falling — resulting in disrupted sleep.
One-third of those immune-compromised participants said they noticed the trend over a year before their lupus onset.
LUPUS EXPERT DEBUNKS 7 COMMON MYTHS ABOUT THE AUTOIMMUNE DISEASE: ‘NOT A DEATH SENTENCE’
Lupus is defined as “a disease that occurs when your body’s immune system attacks your own tissues and organs,” according to the Mayo Clinic.
One in four participants stated that they noticed hallucinations — although 85% said they didn’t experience the symptoms until the disease onset or later.

The study linked patients with an autoimmune disease, such as lupus, to disrupted sleep — including nightmares. (iStock)
Three in five people with lupus and one in three with other rheumatology-related conditions said they noticed an uptick in sleep disruptions just before their hallucinations would begin, according to SWNS.
The lead author of the study, Dr. Melanie Sloan of the University of Cambridge, noted in the study that in many cases, patients and doctors will not discuss mental health or neurological symptoms in relation to these diseases.
Three in five people with lupus noticed an uptick in sleep disruptions just before their hallucinations began.
“It’s important that clinicians talk to their patients about these types of symptoms and spend time writing down each patient’s individual progression of symptoms,” she said.
‘SLEEP DISORDER DROVE MY SON TO SUICIDE,’ NEW YORK MOTHER SAYS: ‘BROKE MY HEART’
Misdiagnosis was also mentioned in the study, as some participants said lupus and other autoimmune diseases were overlooked at first, SWNS reported.
For example, a participant from Scotland was diagnosed with borderline personality disorder at age 18 before being diagnosed with lupus at 19.

The study found that three in five people experienced disrupted sleep with “vivid” and “distressing” nightmares that involved being trapped, attacked or falling. (iStock)
“It was all very close together,” the participant said — noting that it was just a six-month period between “when my borderline personality disorder got under control and my lupus got under control,” SWNS said.
HAVING TROUBLE SLEEPING? IT COULD BE FOR THIS SURPRISING REASON, EXPERTS SAY
Dr. Raj Dasgupta, a California-based chief medical adviser for Sleepopolis, was not involved in the study but shared reaction to the findings with Fox News Digital.
Dasgupta, who is quadruple-board certified in pulmonary, sleep, internal and critical care medicine, said the study supports the perspective that a “high prevalence of neuropsychiatric symptoms, such as headaches, mood and fatigue” are commonly linked to patients with systemic lupus erythematosus (SLE).

Dr. Raj Dasgupta said that sleep issues among patients with SLE need to be discussed in order for people to achieve a better quality of life. (Sleepoplis)
SLE is a “chronic disease that can affect any organ, including the nervous system,” Dasgupta noted.
“This study also supports the fact that patients with SLE are subject to complications of its treatment, including steroid-related psychosis,” he added.
Misdiagnosis was also mentioned in the study.
Sleep issues are common in people with SLE, said Dasgupta, with over half of patients experiencing restlessness, poor sleep quality and difficulty falling asleep.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“These issues can be caused by pain, medication effects and the disease’s impact on the brain,” he said.
Fox News Digital reached out to the eClinicalMedicine journal for further information.
Sleepoplis consists of a team of writers, product reviewers and sleep experts who provide reviews and sleep health content, per the company’s website.
For more Health articles, visit foxnews.com/health
Health
Your June 2024 Horoscope: What’s in Store for You Based on Your Sign
Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
-

 Movie Reviews1 week ago
Movie Reviews1 week agoIs Coppola’s $120M ‘Megalopolis’ ‘bafflingly shallow’ or ‘remarkably sincere’? Critics can’t tell
-

 World1 week ago
World1 week agoTaiwan grapples with divisive history as new president prepares for power
-

 Movie Reviews1 week ago
Movie Reviews1 week agoGuruvayoor Ambalanadayil movie review: This Prithviraj Sukumaran, Basil Joseph-starrer is a total laugh riot
-

 Politics1 week ago
Politics1 week agoSouthern border migrant encounters decrease slightly but gotaways still surge under Biden
-

 World1 week ago
World1 week agoSlovakia PM Robert Fico in ‘very serious’ condition after being shot
-

 Crypto1 week ago
Crypto1 week agoVoice of Web3 by Coingape : Showcasing India’s Cryptocurrency Potential
-

 Politics1 week ago
Politics1 week agoTrump predicts 'jacked up' Biden at upcoming debates, blasts Bidenomics in battleground speech
-

 News1 week ago
News1 week agoThe NFL responds after a player urges female college graduates to become homemakers















