Health
Missing mammograms: Over 20% of women don’t follow breast cancer screening guidelines, study says

A new report has found that 21.7% of U.S. women aged 50 to 74 — around one in five — are not getting mammogram screenings at the recommended frequency.
The United States Preventive Services Task Force (USPSTF), made up of doctors and disease experts, recommends mammograms every two years for women aged 50 to 74 to detect breast cancer.
HelpAdvisor, an online health and finance resource based in California, analyzed survey data from the Centers for Disease Control and Prevention (CDC) to determine the share of women in each state in that age range who had not had a mammogram within two years.
NEW BREAST CANCER SCREENING GUIDELINES CALL FOR WOMEN TO START MAMMOGRAMS AT AGE 40
At least a quarter of the women in 13 states are not following the expert recommendations, the report found.
The state with the highest degree of non-compliance was Wyoming, where 34.2% of women aged 50-74 did not have a mammogram within two years.
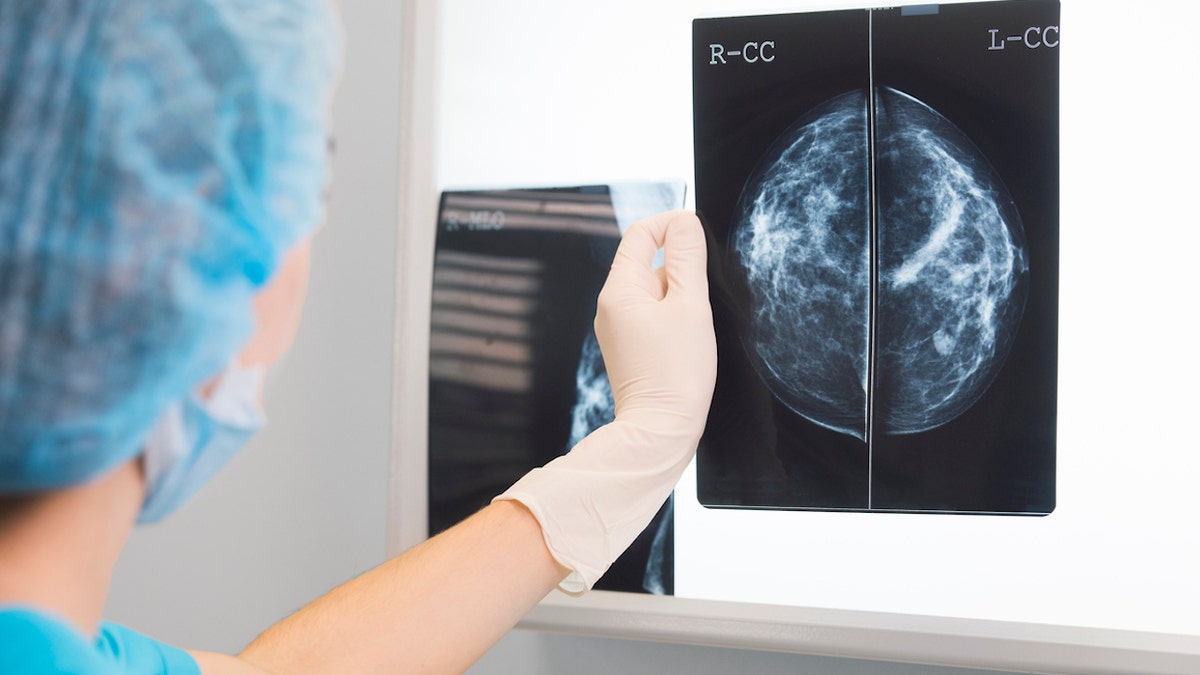
A new report found that 21.7% of U.S. women aged 50 to 74 — around one in five — are not getting mammogram screenings at the recommended frequency. (iStock)
“A shocking percentage of older women are not receiving mammograms at the recommended intervals,” said lead study author Christian Worstell, a senior Medicare and health insurance expert with HelpAdvisor.
5 COMMON MYTHS AND MISCONCEPTIONS ABOUT BREAST CANCER, ACCORDING TO A DOCTOR
“With one out of every five women in this age group leaving themselves exposed to risk, it really makes you worry,” he went on.
“These are your mothers, sisters, wives and friends.”
Reasons for skipped screenings
Dr. Ethan Cohen, a breast radiologist and an associate professor of Breast Imaging at the MD Anderson Cancer Center in Houston, Texas, who was not involved in the study, said there are multiple reasons for noncompliance with mammography.
“The most common are socioeconomic barriers to care, limited knowledge of the benefits of screening, geographic limitations, discomfort with mammography, anxiety from the exam or the possible results, confusion with recommended screening intervals and previous negative health care encounters,” he told Fox News Digital.

The United States Preventive Services Task Force (USPSTF) recommends mammograms every two years for women who are aged 50 to 74 to detect breast cancer. (iStock)
Study author Worstell believes that many people fall victim to the “it won’t happen to me” trap when it comes to health care.
“Or perhaps they feel like ignorance is bliss and they’d rather not know,” he said.
“We’re all probably guilty of that to some extent.”
Some people also may not know that mammograms are considered preventive care and are protected as a free service under most health insurance plans, he pointed out.
“Many people fail to realize that many types of preventive care, like mammograms, won’t cost a thing under the right circumstances.”
“We tend to assume that anytime we visit a doctor, we will have to reach into our pocket, and that keeps some of us away,” Worstell said.
“Many people fail to realize that many types of preventive care, like mammograms, won’t cost a thing under the right circumstances.”
Some people also may not know that mammograms are considered preventive care and are protected as a free service under most health insurance plans, the study author pointed out. (iStock)
There are still millions of uninsured women in the U.S., however, who do not have access to a covered mammogram and may not be able to afford to pay for one out of pocket, he noted.
“Lastly, many people may just not be aware of the recommended ages and frequencies at which mammograms should be done,” Worstell said.
Ways to boost compliance
While health agencies generally do a pretty good job of building awareness around breast cancer, Worstell said, they may be falling short in sharing that mammograms can be free of charge for most people.
BREAST CANCER DRUG COULD HAVE POTENTIALLY SERIOUS SIDE EFFECT, NEW RESEARCH REVEALS
“Doctors and other health care providers could also take more initiative in sending out yearly reminders about mammograms and communicating to their patients that it likely will not cost them anything,” he told Fox News Digital.
“We can all do our part by reminding our loved ones of the importance of mammograms and encouraging them to make an appointment.”
Benefits vs. risks of mammograms
The only people who should not follow the recommended screening schedule, said Cohen, are women who have had both breasts surgically removed and older women with multiple serious medical issues who, after a thorough discussion with their health care provider, have decided that the benefits of screening no longer apply.
Screening mammography saves lives, Cohen said, because it identifies early, asymptomatic breast cancer when it’s more easily treatable.
“Women who are not regularly screened are at higher risk of developing symptomatic cancer, which has a worse prognosis and is more difficult to treat.”
“Women who are not regularly screened are at higher risk of developing symptomatic cancer, which has a worse prognosis and is more difficult to treat,” he told Fox News Digital.
Data indicate that screening mammography reduces death from breast cancer by 20% to 50%, according to Cohen.

Screening mammography saves lives, Cohen said, because it identifies early, asymptomatic breast cancer when it’s more easily treatable. (iStock)
“The main risk of undergoing regular mammograms is what we call a false-positive result, which is where the mammogram identifies a finding that needs more testing and is ultimately found not to be breast cancer,” he said.
“In other words, the main risk of screening is identifying a benign finding (i.e., not cancer) that might need more testing.”
MOST WOMEN DIAGNOSED WITH EARLY BREAST CANCER WILL SURVIVE BEYOND 5 YEARS, STUDY FINDS
Some health care providers, however, are skeptical of the necessity of mammograms — or even question their safety.
Dr. Jenn Simmons, a functional medicine physician and integrative oncologist at Real Health MD in Pennsylvania, claims that mammograms are “painful, traumatic and deliver harmful, cancer-causing radiation to the breast.”

Mammograms are “painful, traumatic and deliver harmful, cancer-causing radiation to the breast,” according to one integrative oncologist in Pennsylvania who shared insights with Fox News Digital. (iStock)
Simmons also echoed Cohen’s point about the risk of false positives.
“As many as 50% of women will get called back from their screening mammogram for additional views, an ultrasound, an MRI and a biopsy,” she said.
“While screening mammograms are a free service, these additional studies are very expensive. This is especially problematic when we consider the fact that the vast majority of the time, these are false positives and there is no worrisome pathology.”
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
As a potential screening option, Simmons pointed out that QT imaging (quantitative transmission ultrasound) is poised to become available in the next few years.
“QT imaging is a novel imaging technique that is safe, fast, relatively inexpensive, has 40 times the resolution of MRI, and is poised to replace all the current breast imaging techniques,” Simmons predicted.
QT Imaging’s website, however, states that the technology is “not intended as a replacement for screening mammography.”
Jay Baker, M.D., a breast imaging specialist at Duke Health in North Carolina, said in June that regular screening can reduce lives lost by 25% to 40%, according to Duke’s website.
For more Health articles, visit www.foxnews.com/health.

Health
How Yvette Nicole Brown Lost Weight and Got Her Diabetes Under Control

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
As bird flu spreads, CDC recommends faster 'subtyping' to catch more cases

As cases of H5N1, also known as avian flu or bird flu, continue to surface across the U.S., safety precautions are ramping up.
The U.S. Centers for Disease Control and Prevention (CDC) announced on Thursday its recommendation to test hospitalized influenza A patients more quickly and thoroughly to distinguish between seasonal flu and bird flu.
The accelerated “subtyping” of flu A in hospitalized patients is in response to “sporadic human infections” of avian flu, the CDC wrote in a press release.
ONE STATE LEADS COUNTRY IN HUMAN BIRD FLU WITH NEARLY 40 CONFIRMED CASES
“CDC is recommending a shortened timeline for subtyping all influenza A specimens among hospitalized patients and increasing efforts at clinical laboratories to identify non-seasonal influenza,” the agency wrote.
The CDC now recommends accelerated subtyping of influenza A in response to “sporadic human infections” in the U.S. (iStock)
“Clinicians and laboratorians are reminded to test for influenza in patients with suspected influenza and, going forward, to now expedite the subtyping of influenza A-positive specimens from hospitalized patients, particularly those in an intensive care unit (ICU).”
LOUISIANA REPORTS FIRST BIRD FLU-RELATED HUMAN DEATH IN US
The goal is to prevent delays in identifying bird flu infections and promote better patient care, “timely infection control” and case investigation, the agency stated.
These delays are more likely to occur during the flu season due to high patient volumes, according to the CDC.
For more Health articles, visit www.foxnews.com/health
Health care systems are expected to use tests that identify seasonal influenza A as a subtype – so if a test comes back positive for influenza A but negative for seasonal influenza, that is an indicator that the detected virus might be novel.

Identifying bird flu infections will support better patient care and infection control, the CDC says. (iStock)
“Subtyping is especially important in people who have a history of relevant exposure to wild or domestic animals [that are] infected or possibly infected with avian influenza A (H5N1) viruses,” the CDC wrote.
In an HHS media briefing on Thursday, the CDC confirmed that the public risk for avian flu is still low, but is being closely monitored.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The agency spokesperson clarified that this accelerated testing is not due to bird flu cases being missed, as the CDC noted in its press release that those hospitalized with influenza A “probably have seasonal influenza.”
Niels Riedemann, MD, PhD, CEO and founder of InflaRx, a German biotechnology company, said that understanding these subtypes is an “important step” in better preparing for “any potential outbreak of concerning variants.”

The CDC recommends avoiding direct contact with wild birds or other animals that may be infected. (iStock)
“It will also be important to foster research and development of therapeutics, including those addressing the patient’s inflammatory immune response to these types of viruses – as this has been shown to cause organ injury and death during the COVID pandemic,” he told Fox News Digital.
Since 2022, there have been 67 total human cases of bird flu, according to the CDC, with 66 of those occurring in 2024.
The CDC recommends that people avoid direct contact with wild birds or other animals that are suspected to be infected. Those who work closely with animals should also wear the proper personal protective equipment (PPE).
Health
Sick Prisoners in New York Were Granted Parole but Remain Behind Bars

When the letter arrived at Westil Gonzalez’s prison cell saying that he had been granted parole, he couldn’t read it. Over the 33 years he had been locked up for murder, multiple sclerosis had taken much of his vision and left him reliant on a wheelchair.
He had a clear sense of what he would do once freed. “I want to give my testimony to a couple of young people who are out there, picking up guns,” Mr. Gonzalez, 57, said in a recent interview. “I want to save one person from what I’ve been through.”
But six months have passed, and Mr. Gonzalez is still incarcerated outside Buffalo, because the Department of Corrections has not found a nursing home that will accept him. Another New York inmate has been in the same limbo for 20 months. Others were released only after suing the state.
America’s elderly prison population is rising, partly because of more people serving long sentences for violent crimes. Nearly 16 percent of prisoners were over 55 in 2022, up from 5 percent in 2007. The share of prisoners over 65 quadrupled over the same time period, to about 4 percent.
Complex and costly medical conditions require more nursing care, both in prison and after an inmate’s release. Across the country, prison systems attempting to discharge inmates convicted of serious crimes often find themselves with few options. Nursing home beds can be hard to find even for those without criminal records.
Spending on inmates’ medical care is increasing — in New York, it has grown to just over $7,500 in 2021 from about $6,000 per person in 2012. Even so, those who work with the incarcerated say the money is often not enough to keep up with the growing share of older inmates who have chronic health problems.
“We see a lot of unfortunate gaps in care,” said Dr. William Weber, an emergency physician in Chicago and medical director of the Medical Justice Alliance, a nonprofit that trains doctors to work as expert witnesses in cases involving prison inmates. With inmates often struggling to get specialty care or even copies of their own medical records, “things fall through the cracks,” he said.
Dr. Weber said he was recently involved in two cases of seriously ill prisoners, one in Pennsylvania and the other in Illinois, who could not be released without a nursing home placement. The Pennsylvania inmate died in prison and the Illinois man remains incarcerated, he said.
Almost all states have programs that allow early release for inmates with serious or life-threatening medical conditions. New York’s program is one of the more expansive: While other states often limit the policy to those with less than six months to live, New York’s is open to anyone with a terminal or debilitating illness. Nearly 90 people were granted medical parole in New York between 2020 and 2023.
But the state’s nursing home occupancy rate hovers around 90 percent, one of the highest in the nation, making it especially hard to find spots for prisoners.
The prison system is “competing with hospital patients, rehabilitation patients and the general public that require skilled nursing for the limited number of beds available,” said Thomas Mailey, a spokesman for the New York Department of Corrections and Community Supervision. He declined to comment on Mr. Gonzalez’s case or on any other inmate’s medical conditions.
Parolees remain in the state’s custody until their original imprisonment term has expired. Courts have previously upheld the state’s right to place conditions on prisoner releases to safeguard the public, such as barring paroled sex offenders from living near schools.
But lawyers and medical ethicists contend that paroled patients should be allowed to choose how to get their care. And some noted that these prisoners’ medical needs are not necessarily met in prison. Mr. Gonzalez, for example, said he had not received glasses, despite repeated requests. His disease has made one of his hands curl inward, leaving his unclipped nails to dig into his palm.
“Although I’m sympathetic to the difficulty of finding placements, the default solution cannot be continued incarceration,” said Steven Zeidman, director of the criminal defense clinic at CUNY School of Law. In 2019, one of his clients died in prison weeks after being granted medical parole.
New York does not publish data on how many inmates are waiting for nursing home placements. One 2018 study found that, between 2013 and 2015, six of the 36 inmates granted medical parole died before a placement could be found. The medical parole process moves slowly, the study showed, sometimes taking years for a prisoner to even get an interview about their possible release.
Finding a nursing home can prove difficult even for a patient with no criminal record. Facilities have struggled to recruit staff, especially since the coronavirus pandemic. Nursing homes may also worry about the safety risk of someone with a prior conviction, or about the financial risk of losing residents who do not want to live in a facility that accepts former inmates.
“Nursing homes have concerns and, whether they are rational or not, it’s pretty easy not to pick up or return that phone call,” said Ruth Finkelstein, a professor at Hunter College who specializes in policies for older adults and reviewed legal filings at The Times’s request.
Some people involved in such cases said that New York prisons often perform little more than a cursory search for nursing care.
Jose Saldana, the director of a nonprofit called the Release Aging People in Prison Campaign, said that when he was incarcerated at Sullivan Correctional Facility from 2010 through 2016, he worked in a department that helped coordinate parolees’ releases. He said he often reminded his supervisor to call nursing homes that hadn’t picked up the first time.
“They would say they had too many other responsibilities to stay on the phone calling,” Mr. Saldana said.
Mr. Mailey, the spokesman for the New York corrections department, said that the agency had multiple discharge teams seeking placement options.
In 2023, Arthur Green, a 73-year-old patient on kidney dialysis, sued the state for release four months after being granted medical parole. In his lawsuit, Mr. Green’s attorneys said that they had secured a nursing home placement for him, but that it lapsed because the Department of Corrections submitted an incomplete application to a nearby dialysis center.
The state found a placement for Mr. Green a year after his parole date, according to Martha Rayner, an attorney who specializes in prisoner release cases.
John Teixeira was granted medical parole in 2020, at age 56, but remained incarcerated for two and a half years, as the state searched for a nursing home. He had a history of heart attacks and took daily medications, including one delivered through an intravenous port. But an assessment from an independent cardiologist concluded that Mr. Teixeira did not need nursing care.
Lawyers with the Legal Aid Society in New York sued the state for his release, noting that during his wait, his port repeatedly became infected and his diagnosis progressed from “advanced” to “end-stage” heart failure.
The Department of Corrections responded that 16 nursing homes had declined to accept Mr. Teixeira because they could not manage his medical needs. The case resolved three months after the suit was filed, when “the judge put significant pressure” on the state to find an appropriate placement, according to Stefen Short, one of Mr. Teixeira’s lawyers.
Some sick prisoners awaiting release have found it difficult to get medical care on the inside.
Steve Coleman, 67, has trouble walking and spends most of the day sitting down. After 43 years locked up for murder, he was granted parole in April 2023 and has remained incarcerated, as the state looks for a nursing home that could coordinate with a kidney dialysis center three times each week.
But Mr. Coleman has not had dialysis treatment since March, when the state ended a contract with its provider. The prison has offered to take Mr. Coleman to a nearby clinic for treatment, but he has declined because he finds the transportation protocol — which involves a strip search and shackles — painful and invasive.
“They say you’ve got to go through a strip search,” he said in a recent interview. “If I’m being paroled, I can’t walk and I’m going to a hospital, who could I be hurting?”
Volunteers at the nonprofit Parole Prep Project, which assisted Mr. Coleman with his parole application, obtained a letter from Mount Sinai Hospital in New York City in June offering to give him medical care and help him transition back into the community.
Still incarcerated two months later, Mr. Coleman sued for his release.
In court filings, the state argued that it would be “unsafe and irresponsible” to release Mr. Coleman without plans to meet his medical needs. The state also said that it had contacted Mount Sinai, as well as hundreds of nursing homes, about Mr. Coleman’s placement and had never heard back.
In October, a court ruled in the prison system’s favor. Describing Mr. Coleman’s situation as “very sad and frustrating,” Justice Debra Givens of New York State Supreme Court concluded that the state had a rational reason to hold Mr. Coleman past his parole date. Ms. Rayner, Mr. Coleman’s lawyer, and the New York Civil Liberties Union appealed the ruling on Wednesday.
Fourteen medical ethicists have sent a letter to the prison supporting Mr. Coleman’s release. “Forcing continued incarceration under the guise of ‘best interests,’ even if doing so is well-intentioned, disregards his autonomy,” they wrote.
Several other states have come up with a different solution for people on medical parole: soliciting the business of nursing homes that specialize in housing patients rejected elsewhere.
A private company called iCare in 2013 opened the first such facility in Connecticut, which now houses 95 residents. The company runs similar nursing homes in Vermont and Massachusetts.
David Skoczulek, iCare’s vice president of business development, said that these facilities tend to save states money because the federal government covers some of the costs through Medicaid.
“It’s more humane, less restrictive and cost-effective,” he said. “There is no reason for these people to remain in a corrections environment.”
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology1 week ago
Technology1 week agoMeta is highlighting a splintering global approach to online speech
-

 Science6 days ago
Science6 days agoMetro will offer free rides in L.A. through Sunday due to fires
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology1 week ago
Technology1 week agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 News1 week ago
News1 week agoPhotos: Pacific Palisades Wildfire Engulfs Homes in an L.A. Neighborhood
-

 Education1 week ago
Education1 week agoFour Fraternity Members Charged After a Pledge Is Set on Fire
-

 Politics1 week ago
Politics1 week agoTrump trolls Canada again, shares map with country as part of US: 'Oh Canada!'
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg) Technology6 days ago
Technology6 days agoAmazon Prime will shut down its clothing try-on program
-

 News1 week ago
News1 week agoMapping the Damage From the Palisades Fire














