Health
COVID-19 pandemic has caused ‘collective trauma’ among US adults, new poll says

Nearly four years after the start of the COVID-19 pandemic, the U.S. population is still experiencing “collective trauma,” a new survey suggests.
The American Psychological Association (APA), headquartered in Washington, D.C., has released the results of Stress in America 2023, its nationwide survey that polled more than 3,185 U.S. adults about their physical and mental well-being.
Adults between the ages of 35 and 44 reported the highest spike in chronic health conditions since the pandemic, rising from 48% in 2019 to 58% in 2023, according to an APA press release.
WOMEN MORE LIKELY TO SUFFER FROM ‘LONG COVID,’ BUT HEALTHY HABITS CAN LOWER THE RISK
That age group also saw the biggest increase in mental heath illnesses, led by anxiety and depression, rising from 31% in 2019 to 45% in 2023.
Even so, adults between 18 and 34 years old still had the highest rate of mental illness, at 50% in 2023.
Nearly four years after the start of the COVID-19 pandemic, the U.S. population is still experiencing “collective trauma,” a new survey suggests. (iStock)
Despite the fact that 66% of adults reported having a chronic illness, 81% of them said their physical health was “good, very good or excellent.”
The same dichotomy was shown for mental illness, with 37% of adults reporting a diagnosis but 81% saying their mental health was “good, very good or excellent.”
COVID PUBLIC HEALTH EMERGENCY IS OVER: HERE’S WHAT IT MEANS FOR YOU
“Although we appear to be back to normal since the COVID-19 pandemic, Americans are experiencing greater levels of stress and reporting higher levels of physical and mental health challenges,” said Arthur C. Evans Jr., PhD, APA’s chief executive officer, in a statement to Fox News Digital.
He added, “The survey shows that the nation continues to experience psychological distress post-COVID. The loss of more than one million Americans and massive disruptions in our workplaces, schools and the broader culture have taken their toll on the mental health of many.”

Adults between ages 35 and 44 reported the highest spike in chronic health conditions since the pandemic, rising from 48% in 2019 to 58% in 2023. (iStock)
The survey revealed that more people are reporting chronic health conditions such as high blood pressure, anxiety and depression than before the pandemic, Evans noted.
Financial and economic issues also rose for adults ages 35 to 44, with money-induced stress rising from 65% to 77% and economy-related concerns rising from 51% to 74% since the pandemic.
“Although we appear to be back to normal since the COVID-19 pandemic, Americans are experiencing greater levels of stress and reporting higher levels of physical and mental health challenges.”
Compared to pre-COVID, parents were more likely to experience financial strain in their households (46% compared to 34%) and fights about money increased by 28%, the survey results showed.
They also reported that they were more likely to “feel consumed” by money-related concerns, rising from 39% in 2019 to 66% in 2023.

“Americans are experiencing greater levels of stress and reporting higher levels of physical and mental health challenges” since the pandemic, said the CEO of the American Psychological Association. (iStock)
Despite the high stress levels, many survey respondents “downplayed” their stress, the release noted.
Sixty-seven percent of the adults said their problems aren’t “bad enough” to be stressed about, and another 62% said they don’t discuss their stress with others to avoid burdening them.
“The rise in chronic illness and mental illness among adults aged 35 to 44 is clearly due to the stress and anxiety provoked by lockdowns and mandates, fear of the virus and the rampant divisiveness.”
Parents of children under 18 seemed to experience the highest levels of stress, with 48% saying that their stress is “completely overwhelming” most days, compared to 26% in 2019.
The share of parents who said their stress keeps them from functioning rose from 20% pre-pandemic to 41% in 2023.
COVID HOSPITALIZATIONS ARE STILL A ‘PUBLIC HEALTH THREAT’ FOR AMERICA’S OLDER ADULTS, SAYS CDC
“Stress affects all systems of the body, so it is crucial that Americans know the serious impacts of stress and what they can do to reduce the effect of stressors in their life, as well as seek help from their health care providers and support systems to prevent further health conditions,” Evans said.
To help boost mental wellness, he said nurturing healthy and supportive relationships is key.
“Particularly during periods of prolonged stress, it’s important that we facilitate opportunities for social connection and support,” Evans said.

Adults ages 35 to 44 were likely most worried about their futures amid business closures and a faltering economy, said one physician. (iStock)
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, was not involved in the APA’s poll but said he did not find the results surprising.
“The rise in chronic illness and mental illness among adults aged 35 to 44 is clearly due to the stress and anxiety provoked by lockdowns and mandates, fear of the virus and the rampant divisiveness,” he told Fox News Digital.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
This particular age group was likely most worried about their futures amid business closures and a faltering economy, Siegel noted.
“On top of this, a sedentary lifestyle, less exercise, poor diet, more smoking and alcohol, and increased stress during the pandemic led to more [incidences of] high blood pressure, heart disease, strokes and cancer, as well as diabetes, lung disease and depression,” the doctor said.
Another potential factor is that long COVID can affect multiple organs, including the brain, said Siegel.
For more Health articles, visit www.foxnews.com/health.

Health
Elderberry Boosts Weight Loss and Improves Blood Sugar, New Study Shows

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Chicago's Lincoln Park Zoo loses flamingo, seal to bird flu
The Avian Influenza has claimed the lives of a Harbor Seal and a Chilean Flamingo at Chicago’s Lincoln Park Zoo.
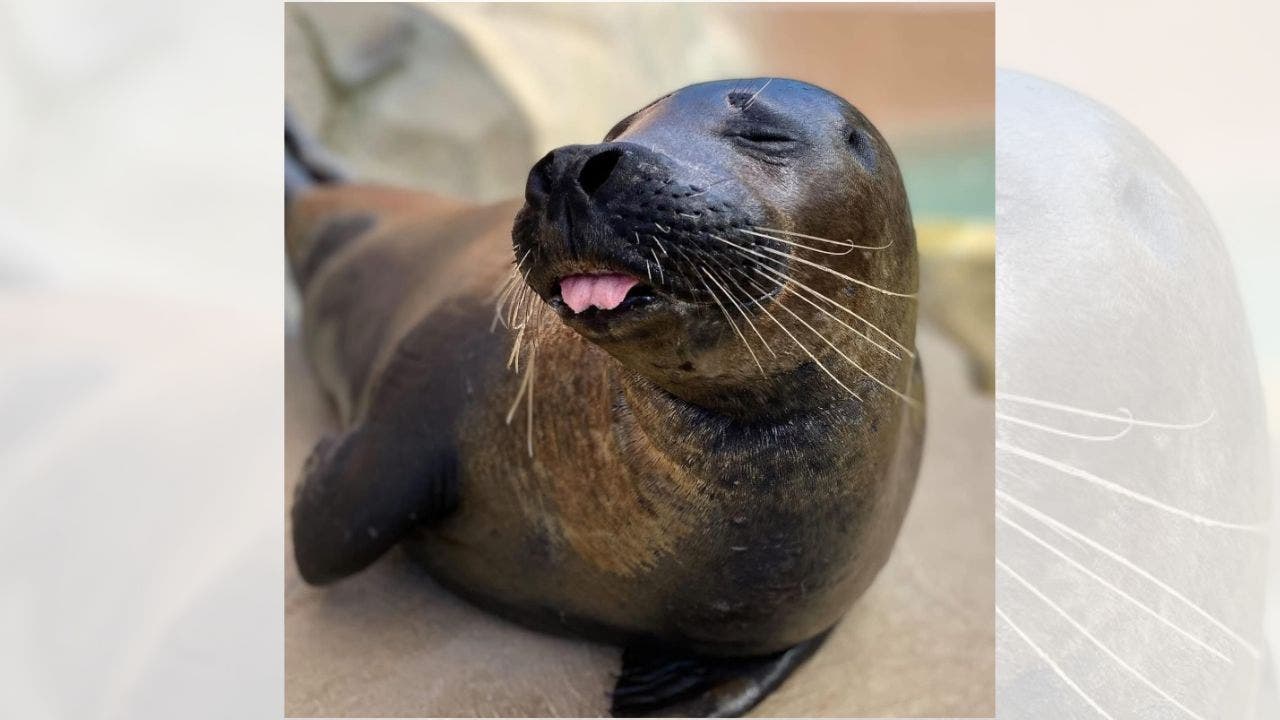
The zoo announced they received results that confirmed the highly pathogenic Avian Influenza was the cause of Teal, a Chilean Flamingo, and Slater, a Harbor Seal’s death.
“This is sad news for wildlife and for the zoo team. Not only are we facing the first known cases of HPAI in animals in our care, but we’ve lost two amazing animals,” said Director of Veterinary Services Lester E. Fisher and Dr. Kathryn Gamble in a statement. “While highly pathogenic avian influenza is a naturally occurring virus in free-ranging waterfowl, more mammal species have been reported to be susceptible to HPAI since 2022.”
ONE STATE LEADS COUNTRY IN HUMAN BIRD FLU WITH NEARLY 40 CONFIRMED CASES
The zoo announced they received results that confirmed the highly pathogenic Avian Influenza was the cause of Teal, a Chilean Flamingo, and Slater, a Harbor Seal’s death. (Lincoln Park Zoo)
The zoo was unable to confirm the source of the exposure, but the Centers for Disease Control say that HPAI is spread through saliva, nasal secretion and the feces of infected birds.
They did say that zoo visitors are not at risk of contracting the disease from the animals at Lincoln Park zoo.
“Because highly pathogenic avian influenza is spread by free-ranging birds, it is no riskier to visit Lincoln Park Zoo than to enjoy a walk outdoors,” said President & CEO and ornithologist Megan Ross. “The zoo remains a safe place to connect with the animals in our care.”
BIRD FLU LEADS TO SEVERE HUMAN ILLNESS AND STATE OF EMERGENCY; EXPERTS DISCUSS RISK

The zoo announced they received results that confirmed the highly pathogenic Avian Influenza was the cause of Teal, a Chilean Flamingo and Slater, a Harbor Seal’s death. (Lincoln Park Zoo)
The zoo has been monitoring HPAI, so there is a response plan in place. The plan addresses staff and animals. It includes personal protective equipment and removing cross contamination between species while monitoring individual animal behavior, according to a statement by the zoo. They have also closed the McCormick Bird House and will be closed until further notice.

The zoo announced they received results that confirmed the highly pathogenic Avian Influenza was the cause of Teal, a Chilean Flamingo and Slater, a Harbor Seal’s death. (Lincoln Park Zoo)
The zoo also said in their statement that it’s important to keep personal pets indoors and away from wildlife.
“Sharing this news of highly pathogenic avian influenza in the area is important for our community at large,” said Director of the Urban Wildlife Institute Seth Magle. “To protect yourself, do not handle wildlife. Additionally, keep your pets safe by keeping cats indoors and dogs on a leash away from wildlife.”
Health
Insulin Prices Dropped. But Some Poor Patients Are Paying More.

Maricruz Salgado was bringing her diabetes under control. Thanks to a federal program that allowed health clinics that serve poor people to buy drugs at steeply discounted prices, she was able to pay less than $75 for all five of her diabetes medications every three months.
But in July, the cost of three of those drugs soared. Ms. Salgado, who does not have health insurance, suddenly faced costs of hundreds of dollars per month. She could not afford it.
Her doctor switched her to cheaper medicines. Within days of taking one of them, she experienced dizzy spells so severe that she said could barely keep up with her hectic daily schedule as a phlebotomist and an in-home caregiver. By the time she returned to the doctor in September, her blood sugar levels had ticked up.
“We were in a good place,” said Dr. Wesley Gibbert, who treats Ms. Salgado at Erie Family Health Centers, a network of clinics in Chicago that serves patients regardless of their ability to pay. “And then all the medicines had to change.”
The price hikes at the clinic happened for a reason that is symptomatic of the tangled web of federal policies that regulate drug pricing. In 2024, drug makers lowered the sticker price of dozens of common medications, which allowed them to avoid massive penalties imposed by the American Rescue Plan, the Covid relief package passed three years earlier. But that change backfired for low-income people like Ms. Salgado.
The decision to make these medications more affordable for large swaths of patients has quietly created another problem: a severe financial hit to the clinics that are tasked by the federal government with caring for the country’s poorest people. These nonprofit clinics operate in every state and serve nearly 32.5 million people, or about 10 percent of the country’s population.
“It’s the law of unintended consequences,” said Beth Powell, the director of pharmacy at The Centers, which operates five community health clinics in the Cleveland area. Ms. Powell said that while many consumers benefited from the companies’ decision to lower prices, “for our folks, that is not the case.”
More than 1,000 community health clinics around the country rely on a decades-old federal program that requires drug companies to offer them deep discounts.
Under the 340B program, as it is called, companies typically sell their brand-name drugs to clinics at a discount, at 23 percent or more off the list price. The same discount scheme applies to state Medicaid plans. But if a company raises a drug’s list price above the rate of inflation, a penalty kicks in, forcing it to offer even deeper discounts to the clinics.
For years, that meant that every time a company raised a drug’s list price above inflation, community clinics paid less for it. Many drugs, including insulin, essentially became free.
But the American Rescue Plan made a major change that hit drug companies with even larger penalties for raising prices. In January 2024, companies that continued to raise a drug’s price would have to pay state Medicaid plans every time those drugs were used, potentially costing the industry billions of dollars.
“That was a bridge too far” for the companies, said Antonio Ciaccia, a drug-pricing researcher who advises state governments and employers.
Manufacturers lowered the price of at least 77 drugs in 2023 and 2024, according to an analysis by a nonprofit that Mr. Ciaccia leads. The list includes widely used asthma drugs like Advair and Symbicort, as well as diabetes treatments like Victoza, which Ms. Salgado used before the change.
Once the pharmaceutical companies lowered their list prices, the inflation penalties evaporated. That meant community clinics had to start paying the usual discounts of 23 percent or more off the list price — far more than the pennies they used to pay.
“Unfortunately, the complexities of the U.S. health care system can reduce access and affordability for many,” Jamie Bennett, a spokeswoman for Novo Nordisk, which makes Victoza, said in a statement. “Even when we lower our prices, too often people don’t receive the savings — this is a problem.” She said the company also has patient assistance programs to make its products more affordable.
David Bowman, a spokesman for the Health Resources and Services Administration, which oversees the 340B discounts, did not respond to questions about how community health clinics were affected by the lowered drug prices. He said that other recent policies, including directing Medicare to negotiate the price of drugs, had lowered drug costs for low-income patients.
Because of a six-month lag in the way that 340B discounts work, clinics were hit by the change last July. Some clinics began calling patients before their prescriptions expired, offering to switch them to less expensive medicines even though they sometimes had more serious side effects. Others decided to cover the higher out-of-pocket costs, which required dipping into already scarce reserves.
Ms. Salgado said a nurse from Erie called over the summer to tell her about the pricing changes. Until then, she had paid about $15 for a three-month supply of Victoza, which is injected daily to keep blood sugar down. After July, the cost rose to more than $300.
After a few weeks, Ms. Salgado adjusted to the replacement, Byetta, and her dizziness subsided. But the drug must be injected twice a day instead of once. And Ms. Salgado must now use a special pharmacy 20 minutes from her house to qualify for the federal discount on the two insulin drugs she was switched to, the result of increasingly strict rules that companies are imposing on health clinics.
Ms. Salgado, who is 39, said she is determined to avoid the fate of her mother, who died of diabetes complications at 54. But keeping up with frequent pharmacy visits and medication changes is tough. “Sometimes it does get to a point where it’s like, I just don’t want to do this anymore,” she said.
The changes are also making it harder for community clinics to offer other services.
Under the 340B program, clinics buy the discounted drugs on behalf of their patients. When those patients have insurance, the clinics can then bill insurers for the regular, higher price, pocketing the difference. But now that spread — the difference between how much they pay for the drug and what insurance will cover — has dwindled. That has left clinics with less money to spend on services that are not otherwise covered by government grants or insurance, such as helping patients find housing.
At Valley View Health Center, a network of clinics that serves patients in rural Washington, the 340B money once financed a mental health program that employed eight therapists. In September, the clinic halted the program, laying off the therapists.
“It was such an abrupt change for us that it has definitely affected our ability to care for our patients the way that we needed to,” said Gaelon Spradley, the clinic’s chief executive.
Some patients who have seen costs go up have qualified for patient-assistance programs offered by drug makers. That was the case for Lorena Sarmiento, another patient at Erie Health who uses Lantus, an insulin pen. Last fall, after the 340B discount changed, she was quoted $490 at her pharmacy — the retail price for a box of insulin pens. Erie Health sent her to another pharmacy, which helped her sign up for a manufacturer’s coupon that lowered her cost to $35 per month.
Doctors and pharmacists at several health clinics said such drug-company assistance programs can be hit or miss. Sometimes they last for a limited time or require that a patient reapply regularly. Patients often have to be legal residents of the United States or have a fixed address.
“It’s a lengthy process, and it’s a lot of hoop-jumping,” said Michael Lin, the chief of pharmacy operations at Family Health Centers in Louisville, Kentucky.
Ms. Sarmiento and her husband, Luis, spend about $500 per month on her medical needs, including special food, medications and a glucose monitor. They are no longer facing the highest insulin price, but their costs are still 10 times what they were just a few months ago, when they spent about $10 on three months’ worth of insulin.
Mr. Sarmiento said he tries not to complain. “You always have to look on the good side,” he said. “But lately, that’s been hard.”
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology1 week ago
Technology1 week agoMeta is highlighting a splintering global approach to online speech
-

 Science5 days ago
Science5 days agoMetro will offer free rides in L.A. through Sunday due to fires
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology1 week ago
Technology1 week agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 News1 week ago
News1 week agoPhotos: Pacific Palisades Wildfire Engulfs Homes in an L.A. Neighborhood
-

 Education1 week ago
Education1 week agoFour Fraternity Members Charged After a Pledge Is Set on Fire
-

 Business1 week ago
Business1 week agoMeta Drops Rules Protecting LGBTQ Community as Part of Content Moderation Overhaul
-

 Politics1 week ago
Politics1 week agoTrump trolls Canada again, shares map with country as part of US: 'Oh Canada!'
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg) Technology5 days ago
Technology5 days agoAmazon Prime will shut down its clothing try-on program















