ENNIS — It isn’t an emergency, it is a home name. Madison Valley Medical Heart first responder Corey Siders not too long ago knocked on the entrance door of an Ennis residence, simply to test on 91-year-old Robert Kensinger.
Kensinger sat together with his walker close to the kitchen desk as Siders took readings for coronary heart charge and blood stress.
“Generally within the morning, it begins to harm; the entire leg. My left foot is swollen,” Kesninger tells the medic.
Some Montana emergency responders, like these within the Madison Valley, are attempting one thing new. As an alternative of solely responding to 911 calls, they’re working with sufferers of their houses to forestall pointless medical emergencies.
Group paramedicine companies can vary from residence check-ins between physician visits to follow-up care with discharged hospital sufferers.
Based on the Montana Division of Public Well being and People Providers, there are 10 emergency medical service companies throughout the state doing this work as a part of a pilot program established by the 2019 Legislature.
The state obtained federal funding to assist arrange a coaching program at Missoula School that would provide its top notch later this yr. DPHHS additionally plans to make use of a separate $5 million federal grant to increase neighborhood paramedicine companies in Montana.
Nicole Steeneken, who works within the state well being division’s EMS and trauma part, says the brand new federal grant will practice practically 50 first responders across the state in neighborhood paramedicine companies. The grant may even pay for these emergency responders’ salaries for a yr and half.
“We’re attempting to hit no less than two suppliers inside every county after which construct upon that with bigger organizations that may fill within the gaps,” Steeneken stated.
Almost 30 EMS companies in Montana have submitted purposes to participate in this system.
Whereas native ambulance suppliers are pleased with the funding in neighborhood paramedicine jobs, it is unclear how they are going to pay for this program, or its workforce, within the long-term.
“Funding is at all times going to be the bane of those kind of applications,” St. Peter’s Well being EMS Supervisor David Webster stated. St. Peter’s has supplied neighborhood paramedicine companies in Helena for 2 years, whereas working it at a monetary loss.
Not like ambulance rides to the hospital, personal insurance coverage suppliers do not cowl the price of emergency responders proactively checking in with sufferers. Medicare and Medicaid do not cowl the price of these visits both.
Whereas these applications can minimize down on pointless medical prices, Webster advised Montana Public Radio that St. Peter’s program does not pay for itself.
“St. Peter’s has stepped as much as the plate. They’ve taken on the duty of subsidizing this program as a result of it is the best factor to do,” Webster stated.
Janet Coffman, a professor of well being coverage on the College of California San Francisco, present in a 2019 examine that 12 out of roughly 30 states with neighborhood paramedicine applications had satisfied insurance coverage suppliers to reimburse EMS companies for the work.
Based on Coffman, a part of the explanation insurers aren’t protecting the prices of this work is a scarcity of knowledge demonstrating its worth.
“The peer-reviewed literature on this isn’t as strong as one would hope that it might be given how widespread neighborhood paramedicine is,” Coffman stated.
The Montana well being division is gathering information on the fee advantage of neighborhood paramedicine applications with hopes of convincing well being protection suppliers to reimburse EMS companies.
The obtainable information in different states are combined.
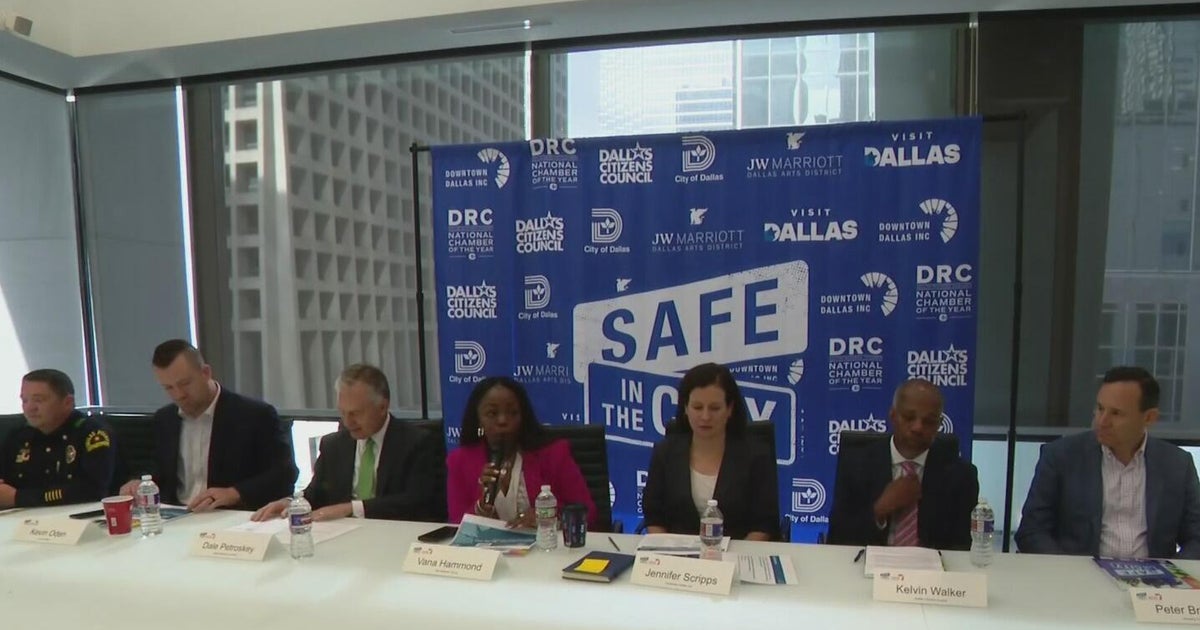
Medstar in Dallas says its neighborhood paramedicine program has saved hundreds of thousands of {dollars} by decreasing ER visits. In Maryland, one examine confirmed a neighborhood paramedicine program was in a position to scale back 911 calls by about 75% in the course of the first 30 days, however after 4 months these good points have been decreased to about 10%.
“Regardless of how good of care you get, in case you’ve received congestive coronary heart failure or COPD, in some unspecified time in the future you are going to get sick sufficient you are again within the hospital,” Coffman stated.
Group paramedicine applications aren’t a silver bullet to eradicate each pointless ER go to or hospital readmission, however they are often price the fee, Coffman stated.
Madison Valley Medical Heart Physician Maura Davenport has seen the worth of this work. One in every of her sufferers in Ennis regularly wound up within the native emergency room anxious about her blood stress. Now, native EMT Corey Siders frequently checks in.
“Simply by means of a few visits, he was in a position to not solely reassure her that she was doing effectively and was managing her hypertension appropriately, however we additionally prevented 1000’s of {dollars} in ER prices and clinic prices, which was improbable,” Davenport stated.
For sufferers like Kensinger, common check-ins by native EMTs assist him keep unbiased and out of a nursing residence.
“There is a chance I might must be within the residence up on the hill. I do not wish to do this,” Kensinger stated.