Science
Some California D.A.s are fighting fentanyl with murder charges. Why San Francisco will join them

County by county in California, as fentanyl overdoses escalate, local prosecutors are turning to a novel legal strategy to stem the spiraling death toll: charging drug dealers with murder.
In July, Placer County reached a landmark plea deal that sent a man to prison for 15 years-to-life on charges of second-degree murder after he provided a Roseville teenager with a fentanyl-contaminated pill that proved lethal.
A month later, a Riverside County jury issued a first-of-its-kind verdict against another man who supplied a lethal dose of a fentanyl-laced pill to a 26-year-old woman. He also was found guilty of second-degree murder and sentenced to at least 15 years in prison.
District attorneys in Sacramento, Fresno, San Joaquin, San Bernardino and San Diego counties are using similar blueprints: going after alleged fentanyl dealers for homicide rather than drug sales, in hopes that the threat of harsher criminal penalties will ease an opioid crisis that killed more than 7,300 Californians in 2022.
Many of the counties adopting the aggressive legal strategy are in “purple” or “red” areas of California, where more conservative law enforcement leaders have long embraced a tough-on-crime philosophy. Now, San Francisco city leaders — famous for their ultraliberal politics — are preparing to follow suit.
Mayor London Breed, police officials and Dist. Atty. Brooke Jenkins are in the final stages of forming a law enforcement task force charged with investigating opioid deaths and illicit drug dealing in the city as potential homicide cases. The effort is set to launch this spring.
In an October statement announcing the initiative, Breed said people selling the synthetic opioid are “on notice that pushing this drug could lead to homicide charges.” Jenkins said the effort would make it easier to hold dealers “accountable for the true dangerousness of their conduct.”
It’s a remarkable shift in rhetoric and strategy for a city regularly lambasted by right-wing pundits as an anything-goes sanctuary for drug dealers and users. The new approach marks a decided bow to mounting pressure from residents and business leaders for the city to rein in an illicit drug culture that has fed the ranks of homelessness and transformed some downtown neighborhoods into squalid open-air drug markets where people are using — and dying — in the streets.
The move toward tougher penalties for dealers comes after other high-profile public initiatives have failed to turn the tide in San Francisco’s drug deaths. In late 2021, Breed declared a state of emergency in the Tenderloin area that in theory made it easier to expand and connect users with treatment and detox services.
In May of last year, Democratic Gov. Gavin Newsom deployed the California National Guard and California Highway Patrol to San Francisco to assist with investigations and prosecution of drug trafficking networks supplying the Tenderloin and South of Market neighborhoods. As of late January, the operation had resulted in 460 arrests and the confiscation of 18,000 grams of fentanyl and 5,000 grams of methamphetamine, according to the governor’s office.
Breed also is sponsoring a controversial March ballot measure to require drug screening for certain people receiving welfare benefits, which she says will push more people into treatment.
Despite the attention, accidental overdose deaths have increased over the last year, surging to a record high of 806 in 2023. Most of those cases — at least 653 — involved fentanyl, according to preliminary data from the San Francisco chief medical examiner’s office.
“The reason why I’ve given clear direction to be much more aggressive in tackling this problem has a lot to do with the loss of life, and also the violence surrounding the drug market,” said Breed, who has shared her story of losing a sister to a drug overdose nearly 20 years ago.
“Because of the number of overdoses, and because it’s directly linked to the drugs, there needs to be a link to the people who are selling this poison that is actually killing people,” she said.
That doesn’t mean every overdose case will be prosecuted as a murder. Instead, investigators will take a “very targeted approach,” Jenkins said. Investigators will work closely with the medical examiner’s office and police to respond quickly to reported deaths and collect evidence that could tie the overdose to a specific drug sale.
Counties leading the charge on the new approach have found such cases tricky to prosecute. Prosecutors have to convince a jury that the person who provided the drug bears responsibility for the overdose, and knew the sale could result in death. District attorneys are treading cautiously and so far have filed only a handful of cases — even as some of these counties record hundreds of overdose deaths each year.
Riverside County has been among the most aggressive in employing the tactic, having filed 34 cases against alleged dealers. Still, that’s a fraction of the 572 opioid overdose deaths the county recorded in 2022, according to California Department of Public Health data. Dist. Atty. Michael Hestrin said his office targets cases where attorneys believe they can show that a dealer is clearly aware of the deadly risks associated with fentanyl and chose to “disregard that danger” in pursuit of profit.
By comparison, Placer County has filed five fentanyl-related homicide cases; Sacramento and San Bernardino, four; San Diego, eight; and Fresno, one.
“This should be used sparingly, and only in those instances where it’s warranted,” said Placer County Dist. Atty. Morgan Gire. “But when it’s warranted, we will do it.”
The tactic has not gained much traction in Los Angeles County, where Dist. Atty. George Gascón has focused resources on addiction prevention efforts and targeting high-level manufacturers and traffickers for prosecution. But some of the candidates running against him in the March primary appear to support the approach.
Such cases hinge on time-consuming investigations, district attorneys employing the strategy said. Investigators dig through cellphone records, text messages, social media accounts and other communications in search of evidence that a dealer knew the product was dangerous.
Gire said his office reviews a defendant’s background, sales history and communications with customers. How did they obtain the fentanyl? Have they been around people who died from an overdose? Have they experimented with the drug or overdosed themselves?
“To prove someone knows something, we have to prove what they’re thinking. We have to get inside their head,” Gire said. “And the best way for us to do that is through things they say and things they do.”
That model could be hard to replicate in San Francisco.
Many of the county prosecutors interviewed said they started filing murder charges after noticing an uptick in the number of seemingly healthy young people dying of overdoses in their community, usually after purchasing a drug online. Often, the cases involve teens experimenting with pills — who might not know the drug they bought was laced with fentanyl — rather than hard-core addicts.
San Francisco’s crisis, in comparison, is most visible and visceral within the homeless population, whose ranks include longtime addicts who obtain drugs from multiple sources.
“Many of the deaths, particularly on the street, are not going to lend themselves to us being able to track down who the seller was,” Jenkins said.
Jenkins’ team is seeking training from San Diego County, which shares some of San Francisco’s struggles with homeless drug deaths. The county has charged eight defendants with homicide in fentanyl-related deaths since 2017, said San Diego County Dist. Atty. Summer Stephan.
Opponents to San Francisco’s task force are quick to point out the lack of empirical data showing that prosecuting street dealers for homicide and sending them to prison for longer terms is proving an effective deterrent. Several of the prosecutors interviewed by The Times said they could point to only anecdotal evidence that the strategy is intimidating would-be dealers.
Keith Humphreys, a professor of psychiatry at Stanford who studies addiction, was skeptical that dangling murder charges over low-level dealers would cause a disruption in the drug supply chain.
“They’re very low-skilled labor. You can spend your half a million, million dollars per, to put them in a state prison system, but they’ll be replaced almost instantly,” Humphreys said. “It’s not out of sympathy that I say we can’t just continually arrest people on the corner. … It’s just futile.”
Instead, Humphreys advocates for more widespread availability of the overdose-reversing nasal spray known as Narcan and for insurance companies to cover substantive mental health and addiction treatment.
Several critics of the new effort say the city won’t make real headway until its leaders deal with the root causes of addiction, including a shortage of affordable housing and effective treatment options and a faltering social safety net.
“A purely punitive approach, it just doesn’t work. If it would have worked, it would have worked over the past 100 years,” said San Francisco Supervisor Hillary Ronen, whose district includes the Mission, another neighborhood struggling with open drug use.
And some speculated, cynically, that the task force is a calculated attempt to build goodwill among voters during an election year in which both Breed and Jenkins are up for reelection. Breed faces a particularly tough reelection bid against at least three other contenders.
Breed has held firm against the criticism. She agrees that encouraging more people to seek treatment is a laudable goal. But, she said, city leaders also have to be “willing to make the hard decisions to make change” and hold people accountable.
“Selling poison should not be protected,” Breed said. “I am frustrated with the criticism for taking too hard of a stance and saying that people have no other way, or no other option. I don’t agree with that.”
Jenkins also insists the initiative isn’t about politics or criminalizing drug users in the throes of addiction.
“I think that is an elementary argument that’s easy for them to make,” she said. “They aren’t responsible for saving the lives of the people that are dying on their streets. I am.”

Science
Q&A: Learn how Olympians keep their cool from Team USA's chief sports psychologist

Your morning jog or weekly basketball game may not take place on an Olympic stage, but you can use Team USA’s techniques to get the most out of your exercise routine.
It’s not all about strength and speed. Mental fitness can be just as important as physical fitness.
That’s why the U.S. Olympic & Paralympic Committee created a psychological services squad to support the mental health and mental performance of athletes representing the Stars and Stripes.
“I think happy, healthy athletes are going to perform at their best, so that’s what we’re striving for,” said Jessica Bartley, senior director of the 15-member unit.
Bartley studied sports psychology and mental health after an injury ended her soccer career. She joined the USOPC in 2020 and is now in Paris with Team USA’s 592 competitors, who range in age from 16 to 59.
Bartley spoke with The Times about how her crew keeps Olympic athletes in top psychological shape, and what the rest of us can learn from them. Her comments have been edited for length and clarity.
Why is exercise good for mental health?
It gets you moving. It gets the endorphins going. And there’s often a lot of social aspects that are really helpful.
There are a number of sports that stretch your brain in ways that can be really, really valuable. You’re thinking about hand-eye coordination, or you’re thinking about strategy. It can improve memory, concentration, even critical thinking.
What’s the best way to get in the zone when it’s time to compete?
When I work with athletes, I like to understand what their zone is. If a 0 or a 1 is you’re totally chilled out and a 10 is you’re jumping around, where do you need to be? What’s your number?
People will say, “I’m at a 10 and I need to be at an 8 or a 7.” So we’ll talk about ways of bringing it down, whether it’s taking a deep breath, listening to relaxing music, or talking to your coach. Or there’s times when people say they need to be more amped up. That’s when you see somebody hitting their chest, or jumping up and down.
If you make a mistake in the middle of a competition, how do you move on instead of dwelling on it?
I often teach athletes a reset routine. I played goalie, so I had a lot of time to think after getting scored on. I would undo my goalie gloves and put them back on, which to me was a reset. I would also wear an extra hairband on my wrist, and when I would snap it, that meant I needed to get out of my head.
It’s not just a physical reset — it helps with a mental reset. If you do the same thing every single time, it goes through the same neural pathway to where it’s going to reset the brain. That can be really impactful.
Do Olympic athletes have to deal with burnout?
Oh, yeah. Everybody has a day where they don’t want to do whatever it is. That’s when you have to ask, “What’s in my best interests? Do I need a recovery day, or do I really need to get in the pool, or get in the gym?”
Sometimes you really do need what we like to refer to as a mental health day.
How can you psych yourself up for a workout when you just aren’t feeling it?
It’s really helpful to think about why you’re doing this and why you’re pushing yourself. Do you have goals related to an activity or sport? Is there something tied to values around hard work or discipline, loyalty or dependability?
When you don’t want to get in the gym, when you don’t want to go for a run, think about something bigger. Tie it back to values.
Is sleep important for maintaining mental health?
Yes! We started doing mental health screens with athletes before the Tokyo Games. We asked about depression, anxiety, disordered eating and body image, drugs and alcohol, and sleep. Sleep was actually our No. 1 issue. It’s been a huge initiative for us.
How much sleep should we be getting?
It’s different for everyone, but generally we know seven to nine hours of sleep is good. Sometimes some of these athletes need 10 hours.
I highly recommend as much sleep as you need. If you didn’t get enough sleep, napping can be really valuable.
Is napping just for Olympic athletes or is it good for everybody?
Everybody! Naps are amazing.
What if there’s no time for a nap?
There are different ways of recharging. Naps could be one of them, but maybe you just need to get off your feet for 20 minutes. Maybe you need to do a meditation or mindfulness exercise and just close your eyes for five minutes.
How do you minimize the effects of jet lag?
We try to shift one hour per day. That’s the standard way of doing it. If you can, it’s super helpful. But it’s not always possible.
The thing we tell athletes is that our bodies are incredible, and you will even things out if you can get back on schedule. One or two nights of crummy sleep is not going to impact your overall performance.
What advice do you give athletes who have trouble falling asleep the night before a competition?
You don’t want to change much right before a competition, so I usually direct athletes to do what they would normally do.
Do you need to unwind by reading a book? Do you need to talk on the phone with somebody and get your mind off things? Can you put your mind in a really restful place and think about things that are really relaxing?
Are there any mindfulness or meditation exercises that you find helpful?
There are some athletes who benefit greatly from an hourlong meditation. I love something quick, something to reset my brain, maybe close my eyes for a minute.
If I’m feeling like I need to take a moment, I love mindful eating. You savor a bite and go, “Oh, my gosh, I have not been fully engaged with my senses today.” Or you could take a mindful walk and take in the sights, the smells, all of the things that are around you.
What do you eat when you need a quick nutrition boost?
Cashews. I tend to carry those with me. They’ve got enough energy to make sure I keep going, physically.
I’ve always got gummy bears on me too. There’s no nutritional value but they keep me going mentally. I’m a big proponent of both.
Is it OK to be superstitious in sports?
It depends how flexible you are. Maybe you put on your socks or shoes a certain way, or listen to certain music. Routines are really soothing. They set your brain up for success in a particular performance. It can be really, really helpful.
But I’ve also seen an athlete forget their lucky underwear or their lucky socks, and they’re all out of sorts. So your routine has to be flexible enough that you’re not going to completely fall apart if you don’t do it exactly.
Are Olympians made of stronger psychological stuff than the rest of us?
Not necessarily. There are some who don’t get feathers ruffled and have a high tolerance for the fanfare. There’s also a lot of regular human beings who just happen to be fantastic at a particular activity.
Science
‘Ready, Steady, Slow’: Championship Snail Racing at 0.006 M.P.H.

Earlier this month, the rural village of Congham, England, played host to a less likely group of athletes: dozens of garden snails. They had gathered to compete in the World Snail Racing Championships, where the world record time for completing the 13.5 inch course stands at 2 minutes flat. At that speed — roughly 0.006 miles per hour — it would take the snails more than six days to travel a mile.
Science
Caring for condor triplets! Record 17 chicks thrive at L.A. Zoo under surrogacy method

A new method of rearing California condors at the Los Angeles Zoo has resulted in a record-breaking 17 chicks hatched this year, the zoo announced Wednesday.
All of the newborn birds will eventually be considered for release into the wild under the U.S. Fish and Wildlife Service’s California Condor Recovery Program, a zoo spokesperson said.
“What we are seeing now are the benefits of new breeding and rearing techniques developed and implemented by our team,” zoo bird curator Rose Legato said in a statement. “The result is more condor chicks in the program and ultimately more condors in the wild.”
Breeding pairs of California condors live at the zoo in structures the staff “affectionately calls condor-miniums,” spokesperson Carl Myers said. When a female produces a fertilized egg, the egg is moved to an incubator. As its hatching approaches, the egg is placed with a surrogate parent capable of rearing the chick.
California condor eggs are cared for at L.A. Zoo. The animal is critically endangered.
(Jamie Pham / L.A. Zoo)
This bumper year of condor babies is the result of a modification to a rearing technique pioneered at the L.A. Zoo.
Previously, when the zoo found itself with more fertilized eggs than surrogate adults available, staff raised the young birds by hand. But condors raised by human caretakers have a lower chance of survival in the wild (hence the condor puppets that zookeepers used in the 1980s to prevent young birds from imprinting on human caregivers).
In 2017, the L.A. Zoo experimented with giving an adult bird named Anyapa two eggs instead of one. The gamble was a success. Both birds were successfully released into the wild.
Faced with a large number of eggs this year, “the keepers thought, ‘Let’s try three,’” Myers said. “And it worked.”
The zoo’s condor mentors this season ultimately were able to rear three single chicks, eight chicks in double broods and six chicks in triple broods. The previous record number of 15 chicks was set in 1997.
Condor experts applauded the new strategy.
“Condors are social animals and we are learning more every year about their social dynamics. So I’m not surprised that these chick-rearing techniques are paying off,” said Jonathan C. Hall, a wildlife ecologist at Eastern Michigan University. “I would expect chicks raised this way to do well in the wild.”
The largest land bird in North America with an impressive wingspan up to 9½ feet, the California condor could once be found across the continent. Its numbers began to decline in the 19th century as human settlers with modern weapons moved into the birds’ territory. The scavenger species was both hunted by humans and inadvertently poisoned by lead bullet fragments embedded in carcasses it ate. The federal government listed the birds as an endangered species in 1967.
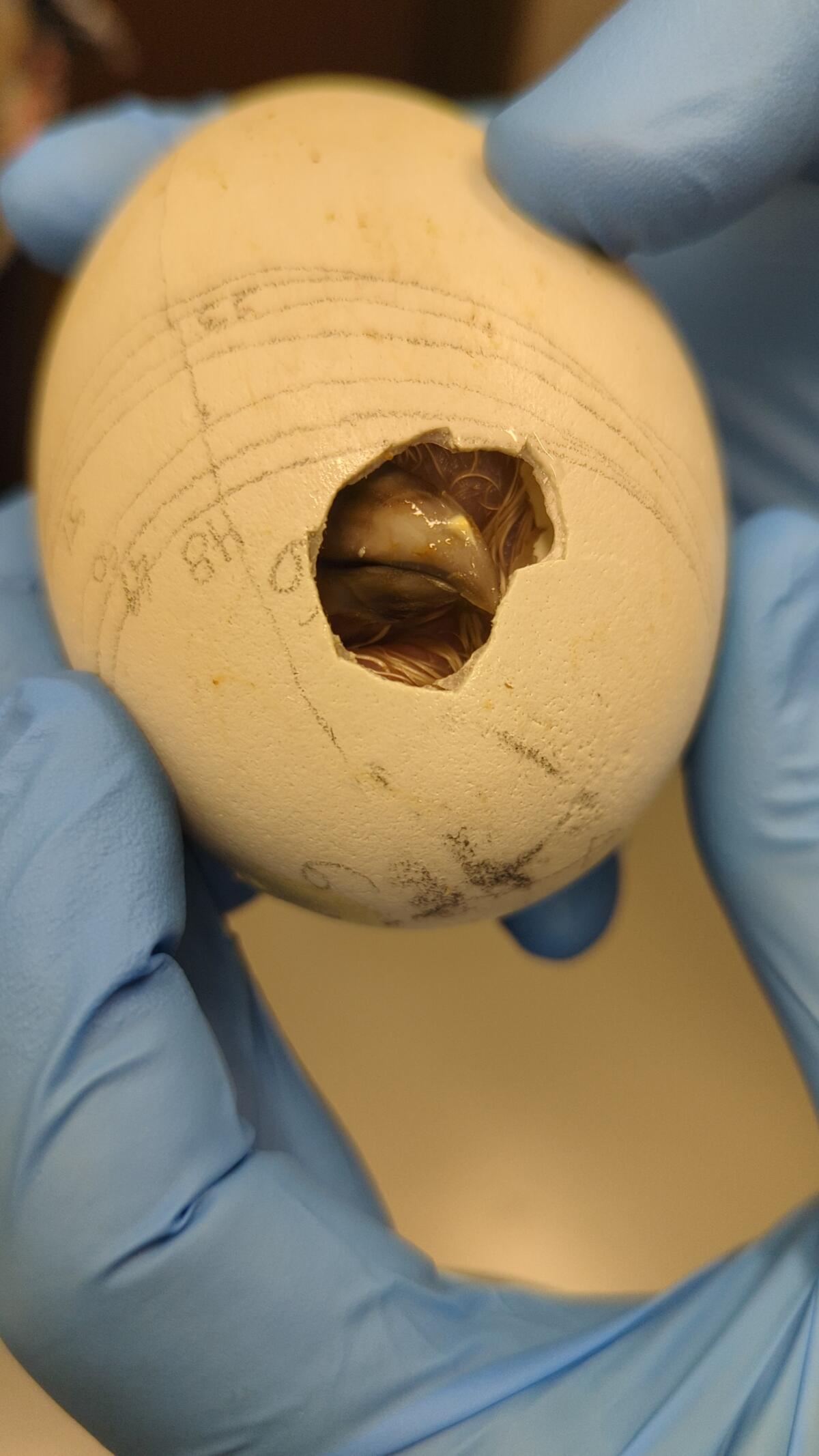
A condor, one of a record-breaking 17 at the zoo, makes its way out of its shell.
(Jamie Pham / L.A. Zoo)
When the California Condor Recovery Program began four decades ago, there were only 22 California condors left on Earth. As of December, there were 561 living individuals, with 344 of those in the wild. Despite the program’s success in raising the population’s numbers, the species remains critically endangered.
In addition to the ongoing threat of lead poisoning, the large birds are also at risk from other toxins. One 2022 study found more than 40 DDT-related compounds in the blood of wild California condors — chemicals that had made their way from contaminated marine life to the top of the food chain.
“Despite our success in returning condors to the wild, free-flying condors continue to face many obstacles with lead poisoning being the No. 1 cause of mortality,” said Joanna Gilkeson, spokesperson for Fish and Wildlife’s Pacific Southwest Region. “Innovative strategies, like those the L.A. Zoo is implementing, help us to produce more healthy chicks and continue releasing condors into the wild.”
The chicks will remain in the zoo’s care for the next year and a half before they are evaluated for potential release to the wild. Thus far, the zoo has contributed 250 condor chicks to Fish and Wildlife’s program, some of which the agency has redeployed to other zoos as part of its conservation efforts.
In a paper published earlier this year, a team of researchers found that birds born in captivity have slightly lower survival rates for their first year or two but then have equally successful outcomes to wild-hatched birds.
“Because condors reproduce slowly, releases of captive-bred birds are essential to the recovery of the species, especially in light of ongoing losses due to lead-related mortality,” said Victoria Bakker, a quantitative ecologist at Montana State University and lead author of the paper. “The team at the L.A. Zoo should be recognized for their innovative and important contributions to condor recovery.”
-

 World1 week ago
World1 week agoOne dead after car crashes into restaurant in Paris
-
 Midwest1 week ago
Midwest1 week agoMichigan rep posts video response to Stephen Colbert's joke about his RNC speech: 'Touché'
-

 News1 week ago
News1 week agoVideo: Young Republicans on Why Their Party Isn’t Reaching Gen Z (And What They Can Do About It)
-

 News1 week ago
News1 week agoIn Milwaukee, Black Voters Struggle to Find a Home With Either Party
-
 Politics1 week ago
Politics1 week agoFox News Politics: The Call is Coming from Inside the House
-

 News1 week ago
News1 week agoVideo: J.D. Vance Accepts Vice-Presidential Nomination
-

 Movie Reviews1 week ago
Movie Reviews1 week agoMovie Review: A new generation drives into the storm in rousing ‘Twisters’
-

 World1 week ago
World1 week agoTrump to take RNC stage for first speech since assassination attempt
















