Science
Q&A: Make the most of your workouts by training like the athletes of Team USA
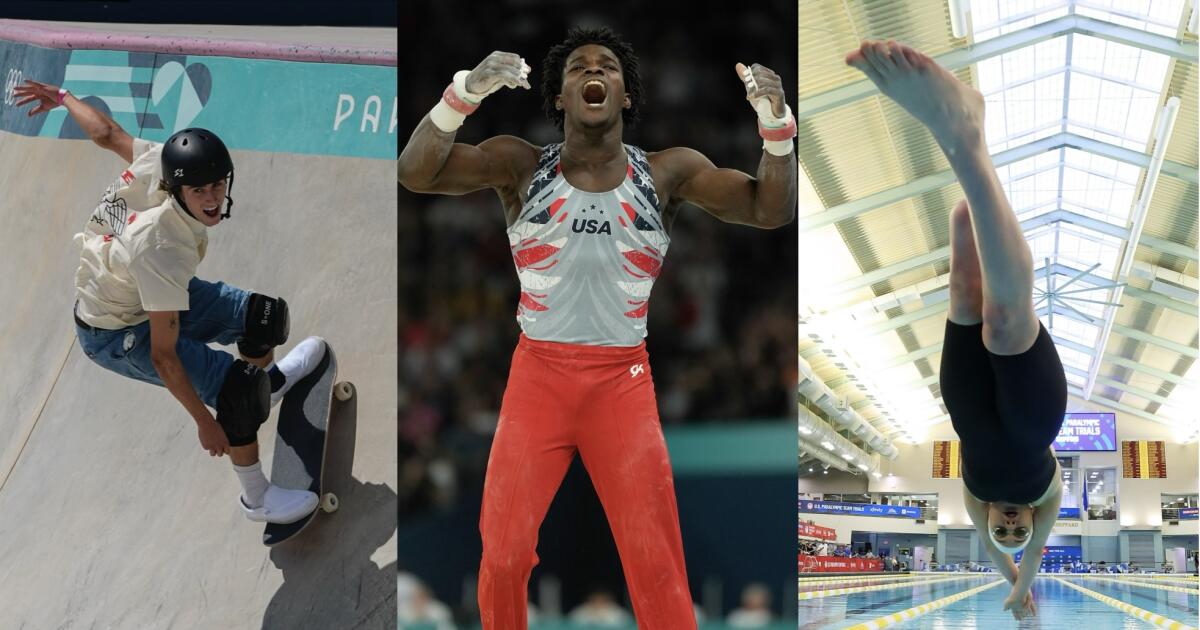
The past two weeks of Olympic competition in Paris have brought us amazing stories of athletic skill, speed, triumph and redemption.
Perhaps they’ve left you newly inspired to train for a 10K or win your weekend basketball league.
Even if you’re not destined to compete on a world stage, learning how to fuel your body and mind like some of the country’s Olympic and Paralympic athletes may help you boost your own game.
Frederick Richard helped the U.S. men’s gymnastics team win a bronze medal, their first Olympic hardware in 16 years. San Diegan Tate Carew finished fifth in the men’s skateboard park final, and swimmer Ali Truwit — who lost part of her leg in a shark attack last year — will hit the pool in the coming weeks.
All three told The Times about the habits that earned them their spots on Team USA. Their comments have been lightly edited for length and clarity.
How do you psych yourself up to work out on days when you just aren’t feeling it?
Frederick Richard: I have been in the gym since I was about 4 years old. I’m there because I love it but even so, there are days when I’m a little less inspired. On those days, I try to remember that it is the process that I enjoy and trust, which keeps me focused.
Ali Truwit: Knowing the deeper meaning of what I’m doing and why is my source of mental toughness on the days I’m not feeling like practicing. Right now, that larger purpose for me is turning trauma into hope and showing the world what people with disabilities are capable of. It drives me forward, even when I’m feeling sad or exhausted or in pain.
Is it OK to skip warming up or cooling down if you’re short on time?
Tate Carew: I rarely go into skating without stretching or warming up in some way. I’d rather have a shorter session knowing that I am preventing petty injuries.
FR: The warm-up and cool-down is not something to miss. You have to take care of your body.
What do you eat when you need a quick nutrition boost?
TC: A peanut butter and jelly sandwich.
FR: Celsius is my go-to drink when I need a little boost.
AT: I like to compete with a light stomach, so I like gluten-free pretzels or sometimes an apple. I love some mini Starbursts right before my race — a little sugar kick.
Do you have any tips about how to space out your meals and snacks?
FR: I definitely try not to eat too close to when I am going to bed.
TC: When I’m hungry, there is no such thing as a bad time to eat.
Any tips for staying properly hydrated? If you get sick of drinking water, is there anything you substitute instead?
AT: I carry a water bottle everywhere, all the time and try to just always be drinking. I also love Gatorade Zero!
TC: Watermelon has been a great substitute for me if I don’t feel like drinking water.
How do you get over jet lag when you travel for competitions?
FR: We generally try to get to places a day or two prior to the competition so that we can adjust to the time and the surroundings. For the Olympics we got to France about a week in advance.
AT: The way to handle conditions that aren’t ideal is to have handled them many times before in your practices. Then you know and believe you can do well anyway.
If you have trouble falling asleep the night before a high-stakes competition, what do you do?
AT: I’ve learned to put habits in place — like warm showers, relaxing mantras and funny shows — that take my mind to a more peaceful place.
FR: I try not to get too stressed, which I can do if I keep the big picture in mind. Trusting in the process is the key for me. I did bring my own mattress to Paris though!
Are there any mindfulness or meditation exercises that you find helpful?
TC: Whenever my mind feels extremely cluttered, I ask myself, “What problem do I have at this very moment?” Meaning, even if you are dealing with a lot in your home life, relationships, work, etc., what problems are you dealing with at that very moment?
AT: I love calm.com and Tamara Levitt! She has a very soothing voice, helpful big-picture insights, and breathwork. I also use progressive muscle relaxation as I’m trying to fall asleep, and I think that encourages the mind and body to let go.
How do you filter out distractions when it’s time to compete?
TC: I made my goals this year so clear that nothing would get in the way of me succeeding.
AT: I remind myself that work works and I’ve done the work. That helps a lot. One of the many reasons I train so hard is so that I can say that to myself before races.
I also just love racing so when I’m in a race, it’s often the only time of day for me that my mind is totally clear and focused.
If you make a mistake in the middle of a competition, how do you move forward instead of dwelling on it?
FR: I know that gymnastics is a judged sport so perfection is difficult. I also know that everyone is going to have some mistakes.
TC: Everything happens for a reason. In a way, it’s motivating for me.
Are there any other tips you’d like to share?
AT: Focus on what you love about competing — the people, the places, the habits you’ve ingrained in yourself, the joys of the process — and the rewards will be there no matter what.
These comments have been lightly edited for length and clarity.

Science
Commentary: My toothache led to a painful discovery: The dental care system is full of cavities as you age

I had a nagging toothache recently, and it led to an even more painful revelation.
If you X-rayed the state of oral health care in the United States, particularly for people 65 and older, the picture would be full of cavities.
“It’s probably worse than you can even imagine,” said Elizabeth Mertz, a UC San Francisco professor and Healthforce Center researcher who studies barriers to dental care for seniors.
Mertz once referred to the snaggletoothed, gap-filled oral health care system — which isn’t really a system at all — as “a mess.”
But let me get back to my toothache, while I reach for some painkiller. It had been bothering me for a couple of weeks, so I went to see my dentist, hoping for the best and preparing for the worst, having had two extractions in less than two years.
Let’s make it a trifecta.
My dentist said a molar needed to be yanked because of a cellular breakdown called resorption, and a periodontist in his office recommended a bone graft and probably an implant. The whole process would take several months and cost roughly the price of a swell vacation.
I’m lucky to have a great dentist and dental coverage through my employer, but as anyone with a private plan knows, dental insurance can barely be called insurance. It’s fine for cleanings and basic preventive routines. But for more complicated and expensive procedures — which multiply as you age — you can be on the hook for half the cost, if you’re covered at all, with annual payout caps in the $1,500 range.
“The No. 1 reason for delayed dental care,” said Mertz, “is out-of-pocket costs.”
So I wondered if cost-wise, it would be better to dump my medical and dental coverage and switch to a Medicare plan that costs extra — Medicare Advantage — but includes dental care options. Almost in unison, my two dentists advised against that because Medicare supplemental plans can be so limited.
Sorting it all out can be confusing and time-consuming, and nobody warns you in advance that aging itself is a job, the benefits are lousy, and the specialty care you’ll need most — dental, vision, hearing and long-term care — are not covered in the basic package. It’s as if Medicare was designed by pranksters, and we’re paying the price now as the percentage of the 65-and-up population explodes.
So what are people supposed to do as they get older and their teeth get looser?
A retired friend told me that she and her husband don’t have dental insurance because it costs too much and covers too little, and it turns out they’re not alone. By some estimates, half of U.S. residents 65 and older have no dental insurance.
That’s actually not a bad option, said Mertz, given the cost of insurance premiums and co-pays, along with the caps. And even if you’ve got insurance, a lot of dentists don’t accept it because the reimbursements have stagnated as their costs have spiked.
But without insurance, a lot of people simply don’t go to the dentist until they have to, and that can be dangerous.
“Dental problems are very clearly associated with diabetes,” as well as heart problems and other health issues, said Paul Glassman, associate dean of the California Northstate University dentistry school.
There is one other option, and Mertz referred to it as dental tourism, saying that Mexico and Costa Rica are popular destinations for U.S. residents.
“You can get a week’s vacation and dental work and still come out ahead of what you’d be paying in the U.S.,” she said.
Tijuana dentist Dr. Oscar Ceballos told me that roughly 80% of his patients are from north of the border, and come from as far away as Florida, Wisconsin and Alaska. He has patients in their 80s and 90s who have been returning for years because in the U.S. their insurance was expensive, the coverage was limited and out-of-pocket expenses were unaffordable.
“For example, a dental implant in California is around $3,000-$5,000,” Ceballos said. At his office, depending on the specifics, the same service “is like $1,500 to $2,500.” The cost is lower because personnel, office rent and other overhead costs are cheaper than in the U.S., Ceballos said.
As we spoke by phone, Ceballos peeked into his waiting room and said three patients were from the U.S. He handed his cellphone to one of them, San Diegan John Lane, who said he’s been going south of the border for nine years.
“The primary reason is the quality of the care,” said Lane, who told me he refers to himself as 39, “with almost 40 years of additional” time on the clock.
Ceballos is “conscientious and he has facilities that are as clean and sterile and as medically up to date as anything you’d find in the U.S.,” said Lane, who had driven his wife down from San Diego for a new crown.
“The cost is 50% less than what it would be in the U.S.,” said Lane, and sometimes the savings is even greater than that.
Come this summer, Lane may be seeing even more Californians in Ceballos’ waiting room.
“Proposed funding cuts to the Medi-Cal Dental program would have devastating impacts on our state’s most vulnerable residents,” said dentist Robert Hanlon, president of the California Dental Assn.
Dental student Somkene Okwuego smiles after completing her work on patient Jimmy Stewart, 83, who receives affordable dental work at the Ostrow School of Dentistry of USC on the USC campus in Los Angeles on February 26, 2026.
(Genaro Molina / Los Angeles Times)
Under Proposition 56’s tobacco tax in 2016, supplemental reimbursements to dentists have been in place, but those increases could be wiped out under a budget-cutting proposal. Only about 40% of the state’s dentists accept Medi-Cal payments as it is, and Hanlon told me a CDA survey indicates that half would stop accepting Medi-Cal patients and many others will accept fewer patients.
“It’s appalling that when the cost of providing healthcare is at an all-time high, the state is considering cutting program funding back to 1990s levels,” Hanlon said. “These cuts … will force patients to forgo or delay basic dental care, driving completely preventable emergencies into already overcrowded emergency departments.”
Somkene Okwuego, who as a child in South L.A. was occasionally a patient at USC’s Herman Ostrow School of Dentistry clinic, will graduate from the school in just a few months.
I first wrote about Okwuego three years ago, after she got an undergrad degree in gerontology, and she told me a few days ago that many of her dental patients are elderly and have Medi-Cal or no insurance at all. She has also worked at a Skid Row dental clinic, and plans after graduation to work at a clinic where dental care is free or discounted.
Okwuego said “fixing the smiles” of her patients is a privilege and boosts their self-image, which can help “when they’re trying to get jobs.” When I dropped by to see her Thursday, she was with 83-year-old patient Jimmy Stewart.
Stewart, an Army veteran, told me he had trouble getting dental care at the VA and had gone years without seeing a dentist before a friend recommended the Ostrow clinic. He said he’s had extractions and top-quality restorative care at USC, with the work covered by his Medi-Cal insurance.
I told Stewart there could be some Medi-Cal cuts in the works this summer.
“I’d be screwed,” he said.
Him and a lot of other people.
steve.lopez@latimes.com
Science
Diablo Canyon clears last California permit hurdle to keep running

Central Coast Water authorities approved waste discharge permits for Diablo Canyon nuclear plant Thursday, making it nearly certain it will remain running through 2030, and potentially through 2045.
The Pacific Gas & Electric-owned plant was originally supposed to shut down in 2025, but lawmakers extended that deadline by five years in 2022, fearing power shortages if a plant that provides about 9 percent the state’s electricity were to shut off.
In December, Diablo Canyon received a key permit from the California Coastal Commission through an agreement that involved PG&E giving up about 12,000 acres of nearby land for conservation in exchange for the loss of marine life caused by the plant’s operations.
Today’s 6-0 vote by the Central Coast Regional Water Board approved PG&E’s plans to limit discharges of pollutants into the water and continue to run its “once-through cooling system.” The cooling technology flushes ocean water through the plant to absorb heat and discharges it, killing what the Coastal Commission estimated to be two billion fish each year.
The board also granted the plant a certification under the Clean Water Act, the last state regulatory hurdle the facility needed to clear before the federal Nuclear Regulatory Commission (NRC) is allowed to renew its permit through 2045.
The new regional water board permit made several changes since the last one was issued in 1990. One was a first-time limit on the chemical tributyltin-10, a toxic, internationally-banned compound added to paint to prevent organisms from growing on ship hulls.
Additional changes stemmed from a 2025 Supreme Court ruling that said if pollutant permits like this one impose specific water quality requirements, they must also specify how to meet them.
The plant’s biggest water quality impact is the heated water it discharges into the ocean, and that part of the permit remains unchanged. Radioactive waste from the plant is regulated not by the state but by the NRC.
California state law only allows the plant to remain open to 2030, but some lawmakers and regulators have already expressed interest in another extension given growing electricity demand and the plant’s role in providing carbon-free power to the grid.
Some board members raised concerns about granting a certification that would allow the NRC to reauthorize the plant’s permits through 2045.
“There’s every reason to think the California entities responsible for making the decision about continuing operation, namely the California [Independent System Operator] and the Energy Commission, all of them are sort of leaning toward continuing to operate this facility,” said boardmember Dominic Roques. “I’d like us to be consistent with state law at least, and imply that we are consistent with ending operation at five years.”
Other board members noted that regulators could revisit the permits in five years or sooner if state and federal laws changes, and the board ultimately approved the permit.
Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
-

 World4 days ago
World4 days agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts4 days ago
Massachusetts4 days agoMother and daughter injured in Taunton house explosion
-

 Montana1 week ago
Montana1 week ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Denver, CO4 days ago
Denver, CO4 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Louisiana7 days ago
Louisiana7 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Technology1 week ago
Technology1 week agoYouTube TV billing scam emails are hitting inboxes
-

 Technology1 week ago
Technology1 week agoStellantis is in a crisis of its own making
-

 Politics1 week ago
Politics1 week agoOpenAI didn’t contact police despite employees flagging mass shooter’s concerning chatbot interactions: REPORT


















