Science
Opinion: The decline in American life expectancy harms more than our health

American life expectancy started dropping even before the pandemic. It’s a critical barometer of our nation’s health and a sign that all is not well in the U.S.
Much of the increase in preventable, premature death is attributable to drug overdose, which increased five-fold over the last couple decades. But this malaise is far broader, driven largely by growing chronic illness.
Rates of depression are reaching new highs. Obesity rates among adults have risen from 30% to 42% since the turn of the century, with severe obesity nearly doubling and driving up the risk of cardiovascular disease, diabetes and other serious health conditions. The return of vaccine-preventable illnesses has been a concern since the 2010s. Sexually transmitted infections have surged in the last decade. And for the first time since 1937, an infectious disease, COVID-19, became one of the top three causes of death in the country.
These health problems are alarming on their own. They also have a devastating impact on our economy. A one-year increase in life expectancy could boost economic output by 4%. On the other hand, as Americans’ health declines, our health expenditures continue to soar. As a country, we spend $4.5 trillion annually on health, representing 17% of GDP. Out-of-pocket healthcare costs have risen dramatically, straining workers’ finances and pushing people into bankruptcy. All this fuels a cycle of a sicker workforce and a weaker economy.
Policymakers acknowledged the link between the economy and public health at the height of the pandemic, providing federal relief programs such as cash assistance and paid sick leave designed to keep the nation’s workforce and economy as healthy as possible. But our abandonment of these efforts since getting COVID relatively under control sets our country up for mounting crises. We need to revive a historical source of support for public health measures: the business case for a healthy workforce.
In 1842, Edwin Chadwick argued in his landmark “Report on the Sanitary Conditions of the Labouring Population of Great Britian” that public health investments are crucial not only from a moral perspective, but also for economic productivity. Writing for the Atlantic in 1909, C.-E. A. Winslow, an American public health pioneer, wrote that employers who try welfare measures for workers “find that it pays.” And around that time, Wickliffe Rose, an American philanthropist, oversaw the Rockefeller Sanitary Commission to tackle hookworm disease as a controllable health problem, spurring economic productivity.
Hookworm, which can cause anemia and fatigue and impair development in children, was a significant problem in southern states in the late 1800s and early 1900s resulting from lack of access to clean water, poor sanitation and poor hygiene. Its symptoms were blamed on “laziness” — a stigma often attached today to symptoms of chronic illnesses, disabilities and mental health issues — and perpetuated cycles of poverty. Rose all-but-eradicated hookworm through education campaigns, expanding access to treatment and improving public sanitation.
Similarly, during World War II, the U.S. government invested in public health initiatives to curb the transmission of malaria in tropical and subtropical battlefronts; vaccinate against smallpox, typhoid fever and tetanus; and control sexually transmitted infections, which during World War I cost the U.S. Army more than 7 million workdays and 10,000 preventable discharges.
When it functions well, such public health infrastructure makes it easier for working people to lead healthy lives. The results have been dramatic, contributing in the last century to the average human lifespan doubling around the world.
Despite the impression given by COVID-19, public health has historically been about so much more than tracking disease outbreaks. It’s been about preventing disease. Access to healthcare and insurance play a role, but doctors and hospitals most often come into play after someone is already sick. Research shows that simple resources such as clean air and water, affordable healthy food, stable housing and safe workplaces are much better predictors of good health and longevity.
During the pandemic, programs addressing basic needs — eviction freezes, expanded food assistance and mandated paid sick and family leave for employees in smaller companies — enhanced housing stability, curbed COVID spread and protected Americans’ mental health. Since then, home affordability has plummeted; half of American renters spend more than 30% of their income on rent and utilities. In 2022, more than 40 million Americans lived in food-insecure households, adding to health issues in adults and children.
The U.S. is one of the only high-income nations that still lacks universal paid sick leave and family medical leave, forcing many people to go to work sick or risk losing a day’s wages. Interventions to improve workplace air quality, a vital component of a healthy workplace appreciated even by 19th and 20th century health reformers, have been overlooked.
The pandemic-era measures were dropped in part because of their cost. But what is much more expensive, and what is causing American workers needless suffering as our national health declines, is our current approach to health. Of our $4.5-trillion annual health spending in the U.S., the vast majority goes to treating people when they are already sick; only 4% supports programs to keep people and workers healthy in the first place. This focus on treating individuals after they have already fallen ill is much of the reason we pay dramatically more than other countries yet still have some of the worst health indicators in the world.
Once again treating public health as an economic imperative could help broaden support for the type of interventions that became polarizing during the pandemic — but have a long track record of improving wellbeing and productivity.
Céline Gounder (@CelineGounder), an infectious-disease physician and epidemiologist, is the senior fellow and editor-at-large for public health at KFF Health News. She is also the host of the podcast “Epidemic.” Craig Spencer (@Craig_A_Spencer) is an emergency medicine physician and professor of public health at Brown University.

Science
Q&A: Learn how Olympians keep their cool from Team USA's chief sports psychologist

Your morning jog or weekly basketball game may not take place on an Olympic stage, but you can use Team USA’s techniques to get the most out of your exercise routine.
It’s not all about strength and speed. Mental fitness can be just as important as physical fitness.
That’s why the U.S. Olympic & Paralympic Committee created a psychological services squad to support the mental health and mental performance of athletes representing the Stars and Stripes.
“I think happy, healthy athletes are going to perform at their best, so that’s what we’re striving for,” said Jessica Bartley, senior director of the 15-member unit.
Bartley studied sports psychology and mental health after an injury ended her soccer career. She joined the USOPC in 2020 and is now in Paris with Team USA’s 592 competitors, who range in age from 16 to 59.
Bartley spoke with The Times about how her crew keeps Olympic athletes in top psychological shape, and what the rest of us can learn from them. Her comments have been edited for length and clarity.
Why is exercise good for mental health?
It gets you moving. It gets the endorphins going. And there’s often a lot of social aspects that are really helpful.
There are a number of sports that stretch your brain in ways that can be really, really valuable. You’re thinking about hand-eye coordination, or you’re thinking about strategy. It can improve memory, concentration, even critical thinking.
What’s the best way to get in the zone when it’s time to compete?
When I work with athletes, I like to understand what their zone is. If a 0 or a 1 is you’re totally chilled out and a 10 is you’re jumping around, where do you need to be? What’s your number?
People will say, “I’m at a 10 and I need to be at an 8 or a 7.” So we’ll talk about ways of bringing it down, whether it’s taking a deep breath, listening to relaxing music, or talking to your coach. Or there’s times when people say they need to be more amped up. That’s when you see somebody hitting their chest, or jumping up and down.
If you make a mistake in the middle of a competition, how do you move on instead of dwelling on it?
I often teach athletes a reset routine. I played goalie, so I had a lot of time to think after getting scored on. I would undo my goalie gloves and put them back on, which to me was a reset. I would also wear an extra hairband on my wrist, and when I would snap it, that meant I needed to get out of my head.
It’s not just a physical reset — it helps with a mental reset. If you do the same thing every single time, it goes through the same neural pathway to where it’s going to reset the brain. That can be really impactful.
Do Olympic athletes have to deal with burnout?
Oh, yeah. Everybody has a day where they don’t want to do whatever it is. That’s when you have to ask, “What’s in my best interests? Do I need a recovery day, or do I really need to get in the pool, or get in the gym?”
Sometimes you really do need what we like to refer to as a mental health day.
How can you psych yourself up for a workout when you just aren’t feeling it?
It’s really helpful to think about why you’re doing this and why you’re pushing yourself. Do you have goals related to an activity or sport? Is there something tied to values around hard work or discipline, loyalty or dependability?
When you don’t want to get in the gym, when you don’t want to go for a run, think about something bigger. Tie it back to values.
Is sleep important for maintaining mental health?
Yes! We started doing mental health screens with athletes before the Tokyo Games. We asked about depression, anxiety, disordered eating and body image, drugs and alcohol, and sleep. Sleep was actually our No. 1 issue. It’s been a huge initiative for us.
How much sleep should we be getting?
It’s different for everyone, but generally we know seven to nine hours of sleep is good. Sometimes some of these athletes need 10 hours.
I highly recommend as much sleep as you need. If you didn’t get enough sleep, napping can be really valuable.
Is napping just for Olympic athletes or is it good for everybody?
Everybody! Naps are amazing.
What if there’s no time for a nap?
There are different ways of recharging. Naps could be one of them, but maybe you just need to get off your feet for 20 minutes. Maybe you need to do a meditation or mindfulness exercise and just close your eyes for five minutes.
How do you minimize the effects of jet lag?
We try to shift one hour per day. That’s the standard way of doing it. If you can, it’s super helpful. But it’s not always possible.
The thing we tell athletes is that our bodies are incredible, and you will even things out if you can get back on schedule. One or two nights of crummy sleep is not going to impact your overall performance.
What advice do you give athletes who have trouble falling asleep the night before a competition?
You don’t want to change much right before a competition, so I usually direct athletes to do what they would normally do.
Do you need to unwind by reading a book? Do you need to talk on the phone with somebody and get your mind off things? Can you put your mind in a really restful place and think about things that are really relaxing?
Are there any mindfulness or meditation exercises that you find helpful?
There are some athletes who benefit greatly from an hourlong meditation. I love something quick, something to reset my brain, maybe close my eyes for a minute.
If I’m feeling like I need to take a moment, I love mindful eating. You savor a bite and go, “Oh, my gosh, I have not been fully engaged with my senses today.” Or you could take a mindful walk and take in the sights, the smells, all of the things that are around you.
What do you eat when you need a quick nutrition boost?
Cashews. I tend to carry those with me. They’ve got enough energy to make sure I keep going, physically.
I’ve always got gummy bears on me too. There’s no nutritional value but they keep me going mentally. I’m a big proponent of both.
Is it OK to be superstitious in sports?
It depends how flexible you are. Maybe you put on your socks or shoes a certain way, or listen to certain music. Routines are really soothing. They set your brain up for success in a particular performance. It can be really, really helpful.
But I’ve also seen an athlete forget their lucky underwear or their lucky socks, and they’re all out of sorts. So your routine has to be flexible enough that you’re not going to completely fall apart if you don’t do it exactly.
Are Olympians made of stronger psychological stuff than the rest of us?
Not necessarily. There are some who don’t get feathers ruffled and have a high tolerance for the fanfare. There’s also a lot of regular human beings who just happen to be fantastic at a particular activity.
Science
‘Ready, Steady, Slow’: Championship Snail Racing at 0.006 M.P.H.

Earlier this month, the rural village of Congham, England, played host to a less likely group of athletes: dozens of garden snails. They had gathered to compete in the World Snail Racing Championships, where the world record time for completing the 13.5 inch course stands at 2 minutes flat. At that speed — roughly 0.006 miles per hour — it would take the snails more than six days to travel a mile.
Science
Caring for condor triplets! Record 17 chicks thrive at L.A. Zoo under surrogacy method

A new method of rearing California condors at the Los Angeles Zoo has resulted in a record-breaking 17 chicks hatched this year, the zoo announced Wednesday.
All of the newborn birds will eventually be considered for release into the wild under the U.S. Fish and Wildlife Service’s California Condor Recovery Program, a zoo spokesperson said.
“What we are seeing now are the benefits of new breeding and rearing techniques developed and implemented by our team,” zoo bird curator Rose Legato said in a statement. “The result is more condor chicks in the program and ultimately more condors in the wild.”
Breeding pairs of California condors live at the zoo in structures the staff “affectionately calls condor-miniums,” spokesperson Carl Myers said. When a female produces a fertilized egg, the egg is moved to an incubator. As its hatching approaches, the egg is placed with a surrogate parent capable of rearing the chick.
California condor eggs are cared for at L.A. Zoo. The animal is critically endangered.
(Jamie Pham / L.A. Zoo)
This bumper year of condor babies is the result of a modification to a rearing technique pioneered at the L.A. Zoo.
Previously, when the zoo found itself with more fertilized eggs than surrogate adults available, staff raised the young birds by hand. But condors raised by human caretakers have a lower chance of survival in the wild (hence the condor puppets that zookeepers used in the 1980s to prevent young birds from imprinting on human caregivers).
In 2017, the L.A. Zoo experimented with giving an adult bird named Anyapa two eggs instead of one. The gamble was a success. Both birds were successfully released into the wild.
Faced with a large number of eggs this year, “the keepers thought, ‘Let’s try three,’” Myers said. “And it worked.”
The zoo’s condor mentors this season ultimately were able to rear three single chicks, eight chicks in double broods and six chicks in triple broods. The previous record number of 15 chicks was set in 1997.
Condor experts applauded the new strategy.
“Condors are social animals and we are learning more every year about their social dynamics. So I’m not surprised that these chick-rearing techniques are paying off,” said Jonathan C. Hall, a wildlife ecologist at Eastern Michigan University. “I would expect chicks raised this way to do well in the wild.”
The largest land bird in North America with an impressive wingspan up to 9½ feet, the California condor could once be found across the continent. Its numbers began to decline in the 19th century as human settlers with modern weapons moved into the birds’ territory. The scavenger species was both hunted by humans and inadvertently poisoned by lead bullet fragments embedded in carcasses it ate. The federal government listed the birds as an endangered species in 1967.
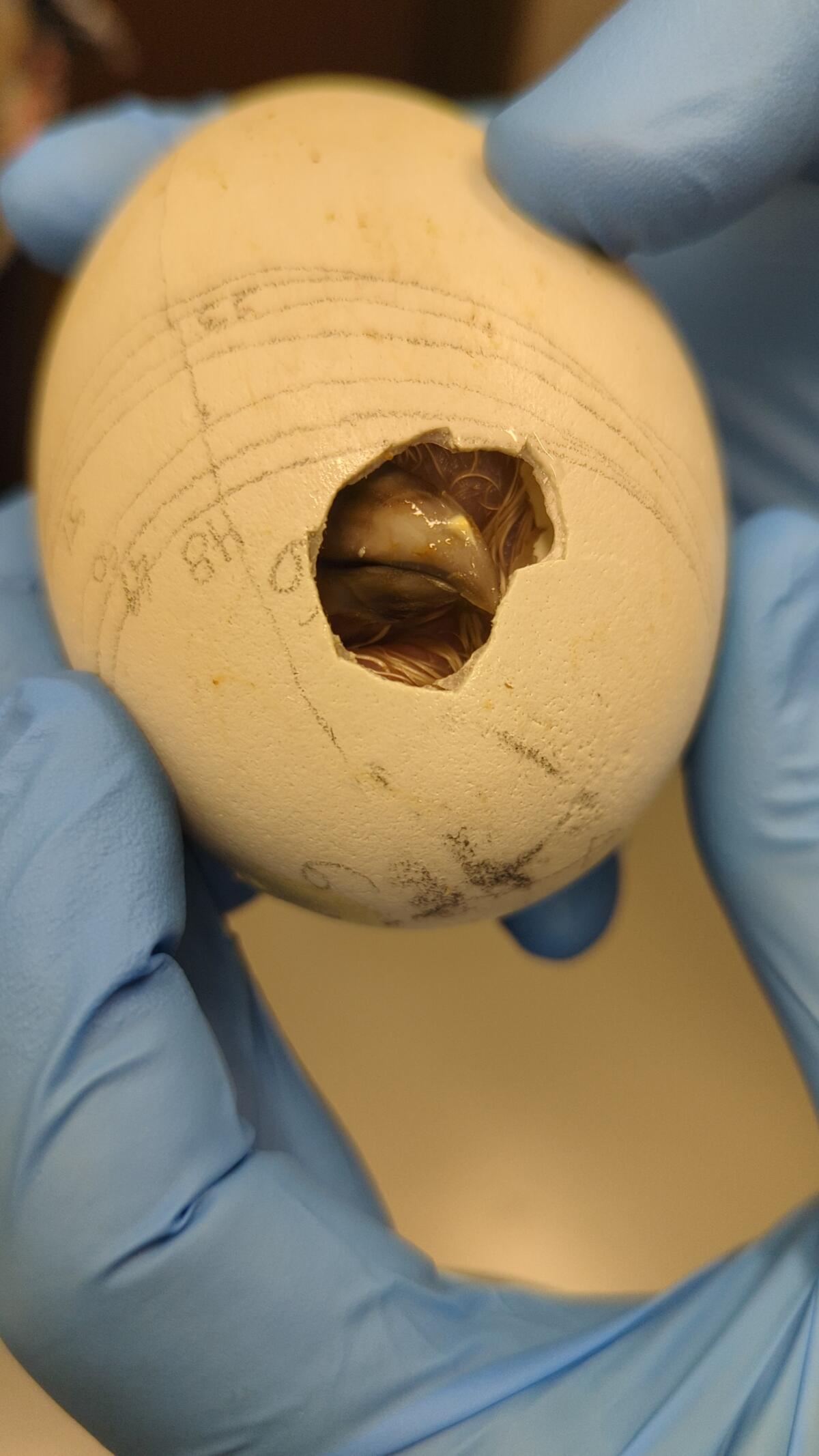
A condor, one of a record-breaking 17 at the zoo, makes its way out of its shell.
(Jamie Pham / L.A. Zoo)
When the California Condor Recovery Program began four decades ago, there were only 22 California condors left on Earth. As of December, there were 561 living individuals, with 344 of those in the wild. Despite the program’s success in raising the population’s numbers, the species remains critically endangered.
In addition to the ongoing threat of lead poisoning, the large birds are also at risk from other toxins. One 2022 study found more than 40 DDT-related compounds in the blood of wild California condors — chemicals that had made their way from contaminated marine life to the top of the food chain.
“Despite our success in returning condors to the wild, free-flying condors continue to face many obstacles with lead poisoning being the No. 1 cause of mortality,” said Joanna Gilkeson, spokesperson for Fish and Wildlife’s Pacific Southwest Region. “Innovative strategies, like those the L.A. Zoo is implementing, help us to produce more healthy chicks and continue releasing condors into the wild.”
The chicks will remain in the zoo’s care for the next year and a half before they are evaluated for potential release to the wild. Thus far, the zoo has contributed 250 condor chicks to Fish and Wildlife’s program, some of which the agency has redeployed to other zoos as part of its conservation efforts.
In a paper published earlier this year, a team of researchers found that birds born in captivity have slightly lower survival rates for their first year or two but then have equally successful outcomes to wild-hatched birds.
“Because condors reproduce slowly, releases of captive-bred birds are essential to the recovery of the species, especially in light of ongoing losses due to lead-related mortality,” said Victoria Bakker, a quantitative ecologist at Montana State University and lead author of the paper. “The team at the L.A. Zoo should be recognized for their innovative and important contributions to condor recovery.”
-

 World1 week ago
World1 week agoOne dead after car crashes into restaurant in Paris
-
 Midwest1 week ago
Midwest1 week agoMichigan rep posts video response to Stephen Colbert's joke about his RNC speech: 'Touché'
-

 News1 week ago
News1 week agoVideo: Young Republicans on Why Their Party Isn’t Reaching Gen Z (And What They Can Do About It)
-

 News1 week ago
News1 week agoIn Milwaukee, Black Voters Struggle to Find a Home With Either Party
-
 Politics1 week ago
Politics1 week agoFox News Politics: The Call is Coming from Inside the House
-

 News1 week ago
News1 week agoVideo: J.D. Vance Accepts Vice-Presidential Nomination
-

 Movie Reviews1 week ago
Movie Reviews1 week agoMovie Review: A new generation drives into the storm in rousing ‘Twisters’
-

 World1 week ago
World1 week agoTrump to take RNC stage for first speech since assassination attempt
















