Health
Illinois reports first measles case since 2019: ‘One of the most contagious diseases known’

The Illinois Department of Public Health (IDPH) recently reported its first case of measles since 2019.
This comes on the heels of a Centers for Disease Control and Prevention (CDC) warning for the public to get fully vaccinated against measles before traveling internationally this summer.
On Oct. 10, the Cook County Department of Public Health (CCDPH) reported a suspected case of measles for an unvaccinated patient who had international exposure.
MEASLES PROTECTION IS PARAMOUNT BEFORE TRAVELING OUTSIDE OF THE US, SAYS CDC
The public health departments are working together to identify potential locations in the U.S. where people may have been exposed, according to the IDPH statement.
One of the first warning signs of measles is a red rash that starts on the face and moves downward on the body, as stated on the CDC website.
The Illinois Department of Public Health (IDPH) recently reported its first case of measles since 2019. (iStock)
“Unfortunately, you can be infectious with measles before the rash appears, which in most cases means before diagnosis happens,” Dr. Anthony Moody, professor of pediatrics and immunology at Duke University School of Medicine in Durham, North Carolina, told Fox News Digital.
CDC ISSUES MEASLES ALERT AFTER CONFIRMED CASE AS ASBURY REVIVAL IN KENTUCKY
People are generally infectious in an eight-day window, he said — “up to four days before the rash appeared and then for four more days after the rash started.”
Since the rash in the Illinois case likely started around Oct. 9, the period of time that the patient could spread the infection was between Oct. 5-13, the statement added.
Key measles symptoms
Measles is a highly contagious virus that can lead to serious complications, such as pneumonia or swelling in the brain known as encephalitis, according to the CDC.
Someone susceptible to measles can develop symptoms anywhere from seven to 21 days after exposure to someone with the disease, the public health statement said.
“The classic symptoms of measles are fever and rash accompanied by the ‘three C’s’: cough, coryza and conjunctivitis,” Moody said.
“That is, cough, runny nose and red eyes.”

Someone susceptible to measles can develop symptoms anywhere from seven to 21 days after exposure to someone with the disease. (iStock)
The fever is often 104 degrees Fahrenheit or higher, while a classic appearance of the rash is “flat red spots that merge together,” Moody said.
“The rash starts on the head (around the ears) and then rapidly spreads to the face and the rest of the body,” he told Fox News Digital.
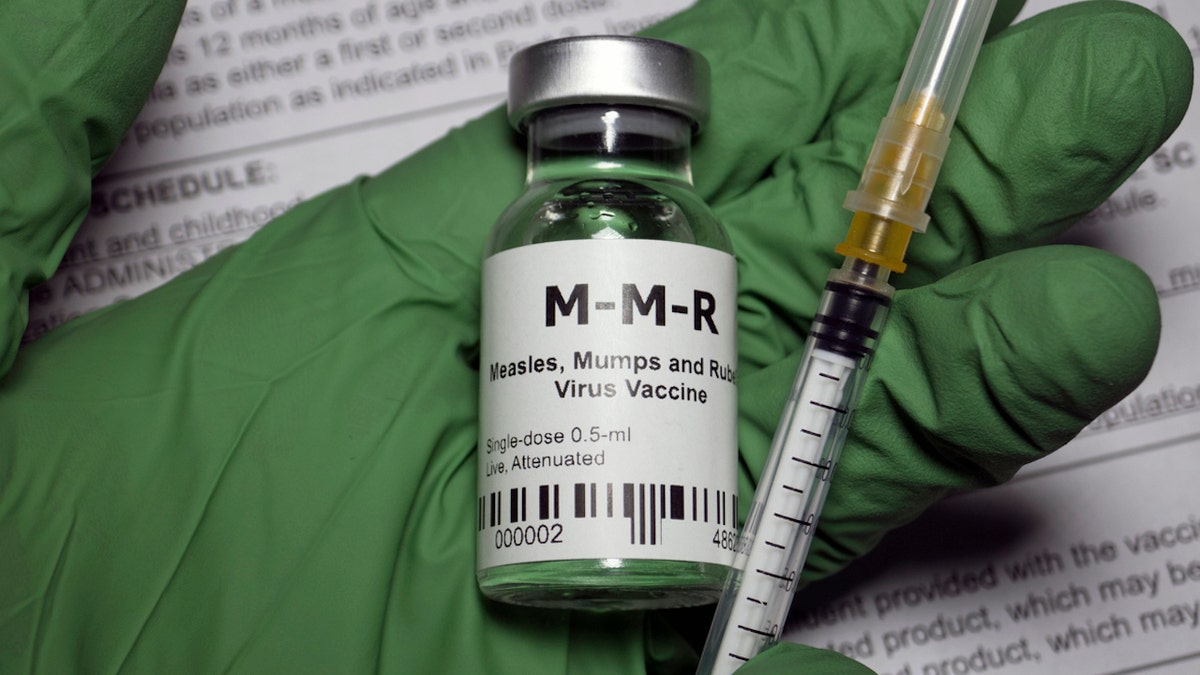
The measles vaccine is often combined with two other vaccines, mumps and rubella, which is collectively known as the MMR vaccine.
“Because there are lots of diseases that cause rash, and because few clinicians these days have seen active measles cases, the symptoms can be incorrectly diagnosed,” the doctor added.
Anyone who thinks they have measles should contact their health care provider before going to the emergency room or clinic, said the IDPH, so that special infection control precautions can be initiated to protect patients and staff.

Most children get the primary measles vaccine series, which consists of two vaccines given right after their first birthday and again around 4 to 6 years of age before they enter school. (Getty Images)
The disease was “eliminated” in the U.S. in 2000 based on an “absence of continuous disease transmission for greater than 12 months” — which means many practicing clinicians have never seen an active measles case, per the CDC.
What to know about the measles vaccine
Most children get the primary measles vaccine series, which consists of two vaccines given right after their first birthday and again around 4 to 6 years of age before they enter school, Moody explained.
The measles vaccine is often combined with two other vaccines, mumps and rubella, collectively known as the MMR vaccine.
The MMR vaccine contains a live “attenuated” virus — which is a weak form of the actual measles virus, per the CDC.

“One dose of MMR vaccine is 93% effective against measles, 78% effective against mumps and 97% effective against rubella,” the CDC noted on its website. “Two doses of MMR vaccine are 97% effective against measles and 88% effective against mumps.” (iStock)
The vaccine works by causing a harmless infection.
People generally will have very few symptoms or none at all as their immune system kicks into gear to fight the infection caused by the virus, the CDC explained.
“One dose of MMR vaccine is 93% effective against measles, 78% effective against mumps and 97% effective against rubella,” the CDC noted on its website. “Two doses of MMR vaccine are 97% effective against measles and 88% effective against mumps.”
COVID-19, FLU AND RSV VACCINES ARE ALL AVAILABLE THIS FALL: SEE WHAT SOME DOCTORS RECOMMEND AND WHY
Some people, or roughly three out of 100, who get fully vaccinated against measles may still get the infection after being exposed to someone with the virus, according to the CDC.
It is recommended that children 1 year or older who are traveling outside the U.S. receive two doses of the MMR vaccine separated by at least 28 days, according to the agency’s summer health alert.
“One dose of MMR vaccine is 93% effective against measles, 78% effective against mumps and 97% effective against rubella,” the CDC noted on its website. “Two doses of MMR vaccine are 97% effective against measles and 88% effective against mumps.” (iStock)
If people are unvaccinated, they should complete the MMR series at least two weeks prior to travel to ensure full immunity by the time they travel.
Transmission of measles
“Measles is one of the most contagious diseases known, rivaling the most aggressive SARS-CoV-2 variants,” Moody said.
“The rule is, if you are in a room with someone who has contagious measles, and you are susceptible, you will get it.”
The best way to prevent measles is to get vaccinated, Moody said.
“We know that 95% (or more) of people need to be vaccinated against measles to prevent outbreaks.”
“Based on how contagious it is, we know that 95% (or more) of people need to be vaccinated against measles to prevent outbreaks.”
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Moody credits the high levels of vaccine coverage starting in the 1960s for the fact that there have been very few cases per year for several decades.
Measles cases are rising, however, amid reduced vaccination rates in the population, Moody said.
“Measles is one of the most contagious diseases known, rivaling the most aggressive SARS-CoV-2 variants,” an expert said. (iStock)
When kids miss their regular appointments where they would typically get their vaccinations, this eventually leads to a larger susceptible population, with pockets of people falling below the critical 95% coverage level, he added.
“If people want to avoid getting sick, they need to get vaccinated,” Moody said.
Amy McGorry contributed reporting.
For more Health articles, visit www.foxnews.com/health.

Health
Sick Prisoners in New York Were Granted Parole but Remain Behind Bars

When the letter arrived at Westil Gonzalez’s prison cell saying that he had been granted parole, he couldn’t read it. Over the 33 years he had been locked up for murder, multiple sclerosis had taken much of his vision and left him reliant on a wheelchair.
He had a clear sense of what he would do once freed. “I want to give my testimony to a couple of young people who are out there, picking up guns,” Mr. Gonzalez, 57, said in a recent interview. “I want to save one person from what I’ve been through.”
But six months have passed, and Mr. Gonzalez is still incarcerated outside Buffalo, because the Department of Corrections has not found a nursing home that will accept him. Another New York inmate has been in the same limbo for 20 months. Others were released only after suing the state.
America’s elderly prison population is rising, partly because of more people serving long sentences for violent crimes. Nearly 16 percent of prisoners were over 55 in 2022, up from 5 percent in 2007. The share of prisoners over 65 quadrupled over the same time period, to about 4 percent.
Complex and costly medical conditions require more nursing care, both in prison and after an inmate’s release. Across the country, prison systems attempting to discharge inmates convicted of serious crimes often find themselves with few options. Nursing home beds can be hard to find even for those without criminal records.
Spending on inmates’ medical care is increasing — in New York, it has grown to just over $7,500 in 2021 from about $6,000 per person in 2012. Even so, those who work with the incarcerated say the money is often not enough to keep up with the growing share of older inmates who have chronic health problems.
“We see a lot of unfortunate gaps in care,” said Dr. William Weber, an emergency physician in Chicago and medical director of the Medical Justice Alliance, a nonprofit that trains doctors to work as expert witnesses in cases involving prison inmates. With inmates often struggling to get specialty care or even copies of their own medical records, “things fall through the cracks,” he said.
Dr. Weber said he was recently involved in two cases of seriously ill prisoners, one in Pennsylvania and the other in Illinois, who could not be released without a nursing home placement. The Pennsylvania inmate died in prison and the Illinois man remains incarcerated, he said.
Almost all states have programs that allow early release for inmates with serious or life-threatening medical conditions. New York’s program is one of the more expansive: While other states often limit the policy to those with less than six months to live, New York’s is open to anyone with a terminal or debilitating illness. Nearly 90 people were granted medical parole in New York between 2020 and 2023.
But the state’s nursing home occupancy rate hovers around 90 percent, one of the highest in the nation, making it especially hard to find spots for prisoners.
The prison system is “competing with hospital patients, rehabilitation patients and the general public that require skilled nursing for the limited number of beds available,” said Thomas Mailey, a spokesman for the New York Department of Corrections and Community Supervision. He declined to comment on Mr. Gonzalez’s case or on any other inmate’s medical conditions.
Parolees remain in the state’s custody until their original imprisonment term has expired. Courts have previously upheld the state’s right to place conditions on prisoner releases to safeguard the public, such as barring paroled sex offenders from living near schools.
But lawyers and medical ethicists contend that paroled patients should be allowed to choose how to get their care. And some noted that these prisoners’ medical needs are not necessarily met in prison. Mr. Gonzalez, for example, said he had not received glasses, despite repeated requests. His disease has made one of his hands curl inward, leaving his unclipped nails to dig into his palm.
“Although I’m sympathetic to the difficulty of finding placements, the default solution cannot be continued incarceration,” said Steven Zeidman, director of the criminal defense clinic at CUNY School of Law. In 2019, one of his clients died in prison weeks after being granted medical parole.
New York does not publish data on how many inmates are waiting for nursing home placements. One 2018 study found that, between 2013 and 2015, six of the 36 inmates granted medical parole died before a placement could be found. The medical parole process moves slowly, the study showed, sometimes taking years for a prisoner to even get an interview about their possible release.
Finding a nursing home can prove difficult even for a patient with no criminal record. Facilities have struggled to recruit staff, especially since the coronavirus pandemic. Nursing homes may also worry about the safety risk of someone with a prior conviction, or about the financial risk of losing residents who do not want to live in a facility that accepts former inmates.
“Nursing homes have concerns and, whether they are rational or not, it’s pretty easy not to pick up or return that phone call,” said Ruth Finkelstein, a professor at Hunter College who specializes in policies for older adults and reviewed legal filings at The Times’s request.
Some people involved in such cases said that New York prisons often perform little more than a cursory search for nursing care.
Jose Saldana, the director of a nonprofit called the Release Aging People in Prison Campaign, said that when he was incarcerated at Sullivan Correctional Facility from 2010 through 2016, he worked in a department that helped coordinate parolees’ releases. He said he often reminded his supervisor to call nursing homes that hadn’t picked up the first time.
“They would say they had too many other responsibilities to stay on the phone calling,” Mr. Saldana said.
Mr. Mailey, the spokesman for the New York corrections department, said that the agency had multiple discharge teams seeking placement options.
In 2023, Arthur Green, a 73-year-old patient on kidney dialysis, sued the state for release four months after being granted medical parole. In his lawsuit, Mr. Green’s attorneys said that they had secured a nursing home placement for him, but that it lapsed because the Department of Corrections submitted an incomplete application to a nearby dialysis center.
The state found a placement for Mr. Green a year after his parole date, according to Martha Rayner, an attorney who specializes in prisoner release cases.
John Teixeira was granted medical parole in 2020, at age 56, but remained incarcerated for two and a half years, as the state searched for a nursing home. He had a history of heart attacks and took daily medications, including one delivered through an intravenous port. But an assessment from an independent cardiologist concluded that Mr. Teixeira did not need nursing care.
Lawyers with the Legal Aid Society in New York sued the state for his release, noting that during his wait, his port repeatedly became infected and his diagnosis progressed from “advanced” to “end-stage” heart failure.
The Department of Corrections responded that 16 nursing homes had declined to accept Mr. Teixeira because they could not manage his medical needs. The case resolved three months after the suit was filed, when “the judge put significant pressure” on the state to find an appropriate placement, according to Stefen Short, one of Mr. Teixeira’s lawyers.
Some sick prisoners awaiting release have found it difficult to get medical care on the inside.
Steve Coleman, 67, has trouble walking and spends most of the day sitting down. After 43 years locked up for murder, he was granted parole in April 2023 and has remained incarcerated, as the state looks for a nursing home that could coordinate with a kidney dialysis center three times each week.
But Mr. Coleman has not had dialysis treatment since March, when the state ended a contract with its provider. The prison has offered to take Mr. Coleman to a nearby clinic for treatment, but he has declined because he finds the transportation protocol — which involves a strip search and shackles — painful and invasive.
“They say you’ve got to go through a strip search,” he said in a recent interview. “If I’m being paroled, I can’t walk and I’m going to a hospital, who could I be hurting?”
Volunteers at the nonprofit Parole Prep Project, which assisted Mr. Coleman with his parole application, obtained a letter from Mount Sinai Hospital in New York City in June offering to give him medical care and help him transition back into the community.
Still incarcerated two months later, Mr. Coleman sued for his release.
In court filings, the state argued that it would be “unsafe and irresponsible” to release Mr. Coleman without plans to meet his medical needs. The state also said that it had contacted Mount Sinai, as well as hundreds of nursing homes, about Mr. Coleman’s placement and had never heard back.
In October, a court ruled in the prison system’s favor. Describing Mr. Coleman’s situation as “very sad and frustrating,” Justice Debra Givens of New York State Supreme Court concluded that the state had a rational reason to hold Mr. Coleman past his parole date. Ms. Rayner, Mr. Coleman’s lawyer, and the New York Civil Liberties Union appealed the ruling on Wednesday.
Fourteen medical ethicists have sent a letter to the prison supporting Mr. Coleman’s release. “Forcing continued incarceration under the guise of ‘best interests,’ even if doing so is well-intentioned, disregards his autonomy,” they wrote.
Several other states have come up with a different solution for people on medical parole: soliciting the business of nursing homes that specialize in housing patients rejected elsewhere.
A private company called iCare in 2013 opened the first such facility in Connecticut, which now houses 95 residents. The company runs similar nursing homes in Vermont and Massachusetts.
David Skoczulek, iCare’s vice president of business development, said that these facilities tend to save states money because the federal government covers some of the costs through Medicaid.
“It’s more humane, less restrictive and cost-effective,” he said. “There is no reason for these people to remain in a corrections environment.”
Health
Surgeon shares story of insurance provider calling during patient's surgery

A surgeon in Austin, Texas, was in the middle of surgery when she was notified of a phone call from the patient’s insurance provider.
Dr. Elisabeth Potter is a board-certified plastic surgeon who specializes in reconstruction for women who have had breast cancer. Last year alone, she did about 520 surgeries for cancer patients.
She recently shared a video of herself talking about the experience.
HEALTH CARE COSTS UP TO 300% HIGHER FOR PRIVATELY INSURED PATIENTS THAN THOSE WITH MEDICARE, REPORT REVEALS
“I just performed two bilateral DIEP flap surgeries and two bilateral tissue expander surgeries,” she said in the now-viral video.
(In DIEP flap surgery reconstruction, skin, fat and blood vessels from the patient’s abdominal area are used to rebuild breasts.)
Dr. Elisabeth Potter, a Texas surgeon, recently shared a video of herself talking about a phone call that came in from an insurance company during a patient’s surgery. (Dr. Elisabeth Potter; @drelisabethpotter)
During one of the DIEP cases, while the patient was asleep on the operating table, the doctor was interrupted by a nurse supervisor informing her that a call had come in from UnitedHealthcare, the patient’s insurance company, Potter said.
The nurse who took the call said that Potter was in surgery and not available.
“And they said, I need to get her a message because we need to talk to her about this patient,” Potter told Fox News Digital. “So they wrote a note and brought it into the operating room and I took a picture of it, because I’m like, I can’t believe this is happening.”
HEALTH CARE IS ‘OVERWHELMINGLY COMPLEX’ FOR OLDER ADULTS, EXPERTS SAY: ‘EVER-INCREASING HURDLE’
The note indicated the name and number of the person to call at UnitedHealthcare, along with the patient’s name and Dr. Potter’s name. (The note did not state that the caller had requested an immediate response.)
“The nurse at the front desk of the OR who took the call and wrote this note said that the person on the phone first asked for the patient and then for me,” Potter told Fox News Digital.
“I made that judgment call and I stand by that — I think it was the right thing to do for the patient.”
“He was told I was scrubbed in[to the] OR and he asked the nurse that I be contacted in OR and given the message.”
Added Potter, “The nurse manager said she had never in her career received a call like that before. She thought it must be important and brought the message to the OR.”

Dr. Elisabeth Potter, a surgeon in Austin, Texas, was in the middle of surgery when she was notified of a phone call from the patient’s insurance provider. (Dr. Elisabeth Potter; @drelisabethpotter)
It was odd, Potter said, that the insurance company had called the front desk of the hospital, where she is not an employee.
“They didn’t call my office. They didn’t call my cell phone. They didn’t send me an email. This wasn’t the billing department of the hospital.”
Afraid that the insurance company might deny the patient’s service, Potter made the decision to scrub out mid-surgery to return the call to United.
BOY FACING BLINDNESS GETS LIFE-CHANGING EYE SURGERY: ‘SUCH A BLESSING’
The surgeon stated to Fox News Digital that UnitedHealthcare did not require her to leave the operating room or threaten to deny coverage.
The patient was safe with another surgeon and the anesthesia team, who were finishing up the procedure.

Dr. Elisabeth Potter is a board-certified plastic surgeon in Texas who specializes in breast reconstruction for women who have had breast cancer. (Dr. Elisabeth Potter)
Potter was “scared” that the patient would wake up and find out that the insurance company said they didn’t have the information they needed and would deny the claim, she said.
“I’ve seen it before, when people get stuck with bills that are $80,000 or $100,000,” she said to Fox News Digital. “And so I said to my partners, ‘I’m going to make this call real quick.’” (See her video here.)
“Dealing with insurance is a really important part of taking care of patients affected by breast cancer, because the diagnosis is financially devastating.”
“If it had been at a critical moment during the surgery, I wouldn’t have,” Potter clarified. “But I made that judgment call and I stand by that — I think it was the right thing to do for the patient.”
On the phone, the insurance company stated that they needed to know the patient’s diagnosis and the justification for the inpatient stay, something Potter had already communicated, she said.
WOMAN RECEIVES PIG KIDNEY TRANSPLANT, WALKS OUT OF HOSPITAL DAYS LATER: ‘SECOND CHANCE’
“And I was like, wait a minute, we got authorization for the surgery. We submitted all of our clinical documentation. We’ve done all the paperwork, the phone calls, all the stuff. You have her diagnosis codes, you have all of it,” she went on.
“And they said, ‘Actually, I don’t, another department has that, but I need this right now,’” Potter said. “There was a sense of entitlement to my time and to the information in that moment,” the surgeon added.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Potter also noted that the person on the line didn’t have access to the patient’s full medical information, despite the procedure already being pre-approved.
“I’m not sure that person even understood that they had an impact on those patients I was operating on,” Potter told Fox News Digital. “They were just thinking about money and numbers and were not understanding at all.”

Potter was “scared” that the patient would wake up and find out that the insurance company said they didn’t have the information they needed and would deny the claim, the surgeon told Fox News Digital. (iStock)
“It’s beyond frustrating and, frankly, unacceptable,” she told Fox News Digital. “Patients and providers deserve better than this. We should be focused on care, not bureaucracy.”
Potter noted that she has always been “devoted” to providing care in-network through insurance.
“Dealing with insurance is a really important part of taking care of patients affected by breast cancer, because the diagnosis is financially devastating,” she told Fox News Digital.
“I’ve found that I really have to engage directly and think about insurance and whether they’re covering treatments and what my patients are experiencing.”
Potter emphasized that she doesn’t think insurance is “evil,” noting that there are some “really good things” about businesses that take care of people.

It was odd, the surgeon felt, that the insurance company called the front desk of the hospital, where she was not an employee. (iStock)
“But this has developed into something that no longer is devoted to patient care. This is just a machine that’s running and making money, and they don’t care about me as a provider,” she said.
Many physicians have given up and refuse to deal with insurance companies, opting to stay out of network and let the patient pay upfront and deal with getting reimbursed, Potter noted.
“Patients and providers deserve better than this.”
“I’ve gone to Washington, D.C., I have fought to protect access to [breast] reconstruction,” she said. “I have testified in the state legislature about these issues.”
She added, “It’s just getting undoable. And this moment, this week, was like, we’ve crossed a line — they’re actually in the operating room.”
HEALTH CARE OR HOUSING? MORE STATES ARE USING MEDICAID FUNDS TO HELP THE HOMELESS
Fox News Digital contacted UnitedHealthcare for comment. The company sent the following statement.
“There are no insurance-related circumstances that would require a physician to step out of surgery and it would create potential safety risks if they were to do so.”
It went on, “We did not ask nor would ever expect a physician to interrupt patient care to answer a call and we will be following up with the provider and hospital to understand why these unorthodox actions were taken.”

Separately, the head of UnitedHealthcare group said on Thursday that the company remains “focused on making high-quality, affordable health care more available while making the health system easier to navigate for patients and providers.” (iStock)
Separately, the head of UnitedHealthcare group said on Thursday that the company is confident it will be able to grow its business in fiscal year 2025.
“The people of UnitedHealthcare remain focused on making high-quality, affordable health care more available to more people while making the health system easier to navigate for patients and providers, positioning us well for growth in 2025,” CEO Andrew Witty said in the company’s earnings report on Thursday.
For more Health articles, visit www.foxnews.com/health
His optimism comes shortly after the head of its insurance unit was gunned down in New York City, inciting a heated conversation about the role of the health insurance industry in the United States.
Fox News Digital’s Daniella Genovese contributed reporting.
Health
Elderberry Boosts Weight Loss and Improves Blood Sugar, New Study Shows

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology1 week ago
Technology1 week agoMeta is highlighting a splintering global approach to online speech
-

 Science6 days ago
Science6 days agoMetro will offer free rides in L.A. through Sunday due to fires
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology1 week ago
Technology1 week agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 News1 week ago
News1 week agoPhotos: Pacific Palisades Wildfire Engulfs Homes in an L.A. Neighborhood
-

 Education1 week ago
Education1 week agoFour Fraternity Members Charged After a Pledge Is Set on Fire
-

 Business1 week ago
Business1 week agoMeta Drops Rules Protecting LGBTQ Community as Part of Content Moderation Overhaul
-

 Politics1 week ago
Politics1 week agoTrump trolls Canada again, shares map with country as part of US: 'Oh Canada!'
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/23935558/acastro_STK103__01.jpg) Technology5 days ago
Technology5 days agoAmazon Prime will shut down its clothing try-on program