Science
The Ex-Patients’ Club

On a recent Friday morning, Daniel, a lawyer in his early 40s, was in a Zoom counseling session describing tapering off lithium. Earlier that week he had awakened with racing thoughts, so anxious that he could not read, and he counted the hours before sunrise.
At those moments, Daniel doubted his decision to wean off the cocktail of psychiatric medications which had been part of his life since his senior year in high school, when he was diagnosed with bipolar disorder.
Was this his body adjusting to the lower dosage? Was it a reaction to the taco seasoning he had eaten the night before? Or was it what his psychiatrist would have called it: a relapse?
“It still does go to the place of — what if the doctors are right?” said Daniel.
On his screen, Laura Delano nodded sympathetically.
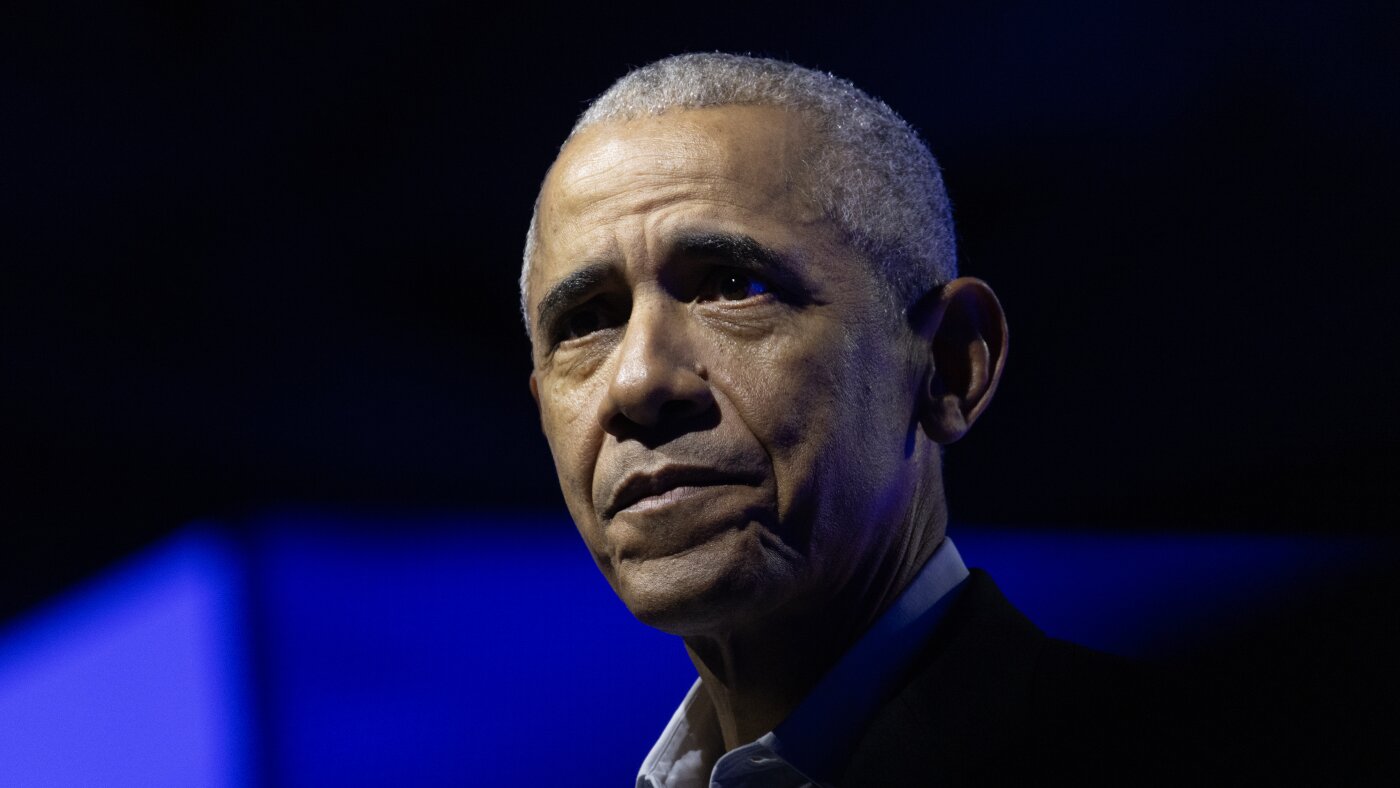
Ms. Delano is not a doctor; her main qualification, she likes to say, is having been “a professional psychiatric patient between the ages of 13 and 27.” During those years, when she attended Harvard and was a nationally ranked squash player, she was prescribed 19 psychiatric medications, often in combinations of three or four at a time.
Then Ms. Delano decided to walk away from psychiatric care altogether, a journey she detailed in a new memoir, “Unshrunk: A Story of Psychiatric Treatment Resistance.” Fourteen years after taking her last psychotropic drug, Ms. Delano projects a radiant good health that also serves as her argument — living proof that, all along, her psychiatrists were wrong.
Since then, to the alarm of some physicians, an online DIY subculture focused on quitting psychiatric medications has expanded and begun to mature into a service industry.
Ms. Delano is a central figure in this shift. From her house outside Hartford, Conn., she offers coaching to paying clients like Daniel. But her ambitions are grander. Through Inner Compass Initiative, the nonprofit she runs with her husband, Cooper Davis, she hopes to provide support to a large swath of people interested in reducing or quitting psychiatric medications.
“People are realizing, ‘I don’t actually need to go find a doctor who knows how to do this,’” she said. In fact, she added, they may not even need to tell their doctor.
“That sounds quite radical,” she allowed. “I imagine a lot of people would hear that and be, like, ‘That’s dangerous.’ But it’s just been the reality for thousands and thousands of people out there who have realized, ‘I have to stop thinking that psychiatry is going to get me out of this situation.’”
Increasingly, many psychiatrists agree that the health care system needs to do a better job helping patients get off psychotropic medications when they are ineffective or no longer necessary. The portion of American adults taking them approached 25 percent during the pandemic, according to government data, more than triple what it was in the early 1990s.
But they also warn that quitting medications without clinical supervision can be dangerous. Severe withdrawal symptoms can occur, and so can a relapse, and it takes expertise to tease them apart. Psychosis and depression may flare up, and the risk of suicide rises. And for people with the most disabling mental illnesses, like schizophrenia, medication remains the only evidence-based treatment.
“What makes tremendous sense for Laura” and “millions of people who are over-diagnosed and over-treated makes no sense at all for people who can’t get medicine,” said Dr. Allen Frances, a professor emeritus of psychiatry at Duke University School of Medicine.
“Laura does not generalize to the person with chronic mental illness and has a clear chance of ending up homeless or in the hospital,” he said. “Those people don’t wind up looking like Laura when they are taken off medication.”
It was hard to say what a life after psychiatric treatment would look like for Daniel, who asked to be identified by only his first name to discuss his mental health history. He has been tapering off lithium for nine months under the care of a nurse-practitioner, and settled, for the moment, at 450 milligrams, half his original dose.
He had become convinced that the drugs were harming him. And yet, when the waves of anxiety and insomnia hit him, he wavered. Daniel is a litigator. He had depositions coming up at work, and the way his thoughts were jumping around scared him.
“I can’t avoid that fear, you know, ‘I’m doing a lot better on less lithium, but it’s just going to fall apart again,’ ” he told Ms. Delano.
Ms. Delano listened quietly, and then told him a story from her own life.
It happened a few months after she quit the last of her medications. On a night walk, her senses built to a crescendo. Christmas lights seemed to be winking messages at her. She recognized hypomania, a symptom of bipolar disorder, and the thought crossed her mind: The doctors had been right. Then some kind of force moved through her, and she realized that these sensations were not a sign of mental illness at all.
“I was like, ‘This is you healing,’ ” she said. “This is you, coming alive.”
She told Daniel that she couldn’t promise he would never have another manic episode. But she could tell him that her own fear had dissipated, over time. “I get to write my own story from here on in,” she said. “And that takes an act of faith.”
Housewives and retirees
Peer support around withdrawing from psychiatric medications dates back 25 years, to the early days of digital social networks.
Adele Framer, a retired information architect from San Francisco, discovered such groups in 2005 while going through a difficult withdrawal from Paxil. At the time, Ms. Framer said, physicians dismissed severe withdrawal as “basically impossible.”
People circulated between the groups, comparing “tapers” in “a viral information-sharing process,” said Ms. Framer, who launched her own site, Surviving Antidepressants, in 2011. Users on her site exchanged highly technical tapering protocols, with dose reductions so tiny that they sometimes required syringes and precision scales.
Dr. Mark Horowitz, an Australian psychiatrist, discovered Ms. Framer’s site in 2015 and used the peer advice he found to taper off Lexapro himself.
“At that point, I understood who the experts were,” he said. “I have six academic degrees, I have a Ph.D., I know how antidepressants work, and I was taking advice from retired engineers and housewives on a peer support site to help come off the drugs.”
In recent years, mainstream psychiatry has begun to acknowledge the need for more support for patients getting off medications.
This is most visible in Britain, whose health service has updated its guidance for clinicians to acknowledge withdrawal and recommend regular reviews to discontinue unnecessary medications. In 2024, the Maudsley Prescribing Guidelines in Psychiatry, a respected clinical handbook, issued its first “de-prescribing” volume. Dr. Horowitz was one of its authors.
There are early signs of movement in the United States, as well. Dr. Jonathan E. Alpert, chairman of the American Psychiatric Association’s Council on Research, said that the group plans to issue its own de-prescribing guide.
The American Society of Clinical Psychopharmacology is working on a guide to help doctors identify when a medication should be discontinued. “There has never been an incentive in industry to tell people when to stop using their product,” said Dr. Joseph F. Goldberg, the group’s president. “So it really falls to the nonindustry community to ask those questions.”
Dr. Gerard Sanacora, the director of the Yale Depression Research Program, said there are practical reasons the current health care system “doesn’t provide much support” for patients seeking to reduce medications: Relapse prevention can be time-consuming, and many physicians are only reimbursed for 15-minute “med management” appointments.
But he said it was important that trained clinicians still have a role. In a “taper,” patients encounter difficulties of two kinds: withdrawal, and the relapse of underlying conditions. It takes skill to distinguish between them, he said, and a licensed practitioner guarantees “some level of minimum competency” during a period of especially high risk.
“The main thing is, they can worsen and kill themselves,” he said of patients.
A success story
Ms. Delano entered the conversation in 2010, when she began blogging about her life. She was 27 years old, living with her aunt and uncle and attending day treatment at McLean Hospital in Massachusetts. Her platform was Mad in America, a website where a range of former psychiatric patients exchanged stories about their treatment.
Within that subculture, Ms. Delano stood out for her eloquence and charisma. She had grown up in Greenwich, Conn., where she was a top student and standout athlete. A relative of Franklin D. Roosevelt, she was presented as a debutante on two successive nights at New York’s Waldorf Astoria and Plaza hotels.
On her blog, and later in a 10,000-word profile in The New Yorker, she described the shadow plot of her psychiatric treatment.
In ninth grade, she was diagnosed with bipolar disorder and prescribed Depakote and Prozac. In college, her pharmacologists added Ambien and Provigil. Over the years, this list expanded, but she still seemed to be getting worse. Four times she was so desperate that she checked herself into psychiatric hospitals. At 25, she made a harrowing attempt at suicide.
Then, at 27, she picked up a book by the journalist Robert Whitaker, “Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America.” In the book, Mr. Whitaker proposed that the increasing use of psychotropic medications was to blame for the rise in psychiatric disorders. In scientific journals, reviewers dismissed Mr. Whitaker’s analysis as polemical, cherry-picking data to support a broad, oversimplified argument.
But for Ms. Delano, it was an epiphany. She mentally reviewed her treatment history and came to a radical conclusion. “I’d been confronted with something I’d never considered,” she writes in “Unshrunk.”“What if it wasn’t treatment-resistant mental illness that had been sending me ever deeper into the depths of despair and dysfunction, but the treatment itself?”
She quit five drugs over the six months that followed, under the guidance of a psychopharmacologist. She describes a brutal withdrawal, complete with constipation, diarrhea, aches, spasms and insomnia, as “angsty energy that had lived in me for years began to scratch viciously beneath the surface of my skin.”
But she also experienced a kind of awakening. “I knew it as clear as day, the second it occurred to me,” she writes. “I was ready to stop being a psychiatric patient.”
Born in 1983, five years before Prozac entered the market, Ms. Delano was part of the first large wave of Americans to be prescribed medications in their teens. Many readers recognized, in her blog entries, elements of their own stories — the way a diagnosis had become part of their identities, the way a single prescription had expanded into a cocktail.
She also provided something the ex-patient community had lacked: an aspirational model. Her life had clearly flourished after quitting her medications. In 2019 she married Mr. Davis, an activist she met in the ex-patient movement; they are raising two boys in an airy, sun-drenched colonial-style house.
On the Surviving Antidepressants website, users sometimes invoked her name wistfully.
“I thought I’d be like a Laura Delano and others and heal right away,” a user from Kansas commented.
A French user, struggling to wean off Valium, returned to Ms. Delano’s videos as to a mantra.
“9.30 am: I manage to stop a panic attack with agitation, by breathing.
10:30 a.m.: It rains. I spend time on my smartphone. Laura Delano. Laura Delano. Laura Delano. On a loop. Maybe I’m in love.”
‘I feel for psychiatry’
Emails began to flow in to Ms. Delano as she blogged about quitting her medications. Most were from people who wanted her advice on tapering. Often, she said, they had tried to taper too fast and were spinning out.
She encouraged them, assuring “overwhelmed, exhausted partners and parents” that what they were witnessing was not relapse, but withdrawal. Ms. Delano found that she was spending 25 hours a week on these calls. And a coaching business was born.
“I saw the demand for what I had to offer and made the difficult decision to stop giving my time away for free,” she writes in her memoir.
The market for assisting withdrawal from psychiatric medications is becoming crowded these days, with some private clinics charging thousands of dollars a week. And a watershed moment arrived last month, when Health Secretary Robert F. Kennedy Jr. announced that the new “Make America Healthy Again” commission would examine the “threat” posed by antidepressants and stimulants.
Mr. Kennedy has long expressed skepticism about psychiatric medications; in his confirmation hearings, he suggested that selective serotonin reuptake inhibitors, or S.S.R.I.s, have contributed to a rise in school shootings, and that they can be harder to quit than heroin. There is no evidence to back up either of these statements. But Mr. Davis agreed.
“He might be the only person in the room who gets how serious it can be,” Mr. Davis wrote on X during the hearings.
Ms. Delano and Mr. Davis both offer coaching — for $595 a month, you can join a group support program. But the project that excites them more is the membership community hosted by their nonprofit, Inner Compass Initiative, which, for $30 a month, links up members via livestreams, Zoom gatherings and a private social network.
They dream of a national “de-prescribing” network along the lines of Alcoholics Anonymous, said Mr. Davis, who became the group’s executive director early this year. “We know there is a sea change coming,” he said. “It’s already beginning. In a lot of circles, it’s deeply unfashionable to take psych meds.”
Ms. Delano has tempered her language since her Mad in America Days, when she protested outside annual meetings of the American Psychiatric Association, denouncing the use of four-point restraints and electroshock machines.
In the early pages of her memoir, she assures readers that she is not “anti-medication” or “anti-psychiatry.”
“To be clear, I am neither of these things,” she writes. “I know that many people feel helped by psychiatric drugs, especially when they’re used in the short term.”
Still, there is no mistaking the bedrock of mistrust that underlies her project. “I feel for psychiatry,” she said. “It’s a big ask we’re putting on them, to basically step back and consider that their entire paradigm of care is inadvertently causing harm to a lot of people.”
An echo chamber
Earlier this month, Mr. Davis flew to Washington to hand-deliver copies of “Unshrunk” to elected officials and explore whether Inner Compass might find new sources of funding in the new, pharma-skeptical dispensation. He wanted to make sure, he said, “that the people working on policy are at least considering our ideas.”
The rollout of Mr. Kennedy’s agenda has raised hopes throughout “critical psychiatry” and “anti-psychiatry” communities that their critiques will, for the first time, be taken seriously.
Some in the medical world fear this augurs a deepening mistrust in science. And it is true — the written resources Inner Compass provides are overwhelmingly negative about every major class of psychiatric medications, which remain the only evidence-based treatment for severe mental illnesses.
A section on antipsychotics, for instance, cites studies that purport to show that people who take them fare worse than people who never take them or stop them. (This is misleading; people do not take them unless they have severe symptoms.) A section on antidepressants cites a study suggesting that they cause people to commit acts of violence. (The study was criticized for distorting its findings.)
Dr. Alpert, who is also chairman of psychiatry and behavioral sciences at Montefiore Einstein, reviewed Inner Compass’s resources and described them as “biased” and “frightening.” He said online peer communities risk becoming “echo chambers,” since they tend to attract people who have had bad experiences with medical treatment.
Because quitting psychiatric medications can be so risky, he said, a pervasive mistrust of medical care could have serious consequences.
“I mean, what happens when people taper their medications because of an echo chamber, and they’re more suicidal, or they get more psychotic, and they need to be hospitalized, or they lose their job?” he said. “Who cares about those people?”
This worry was shared even by some of Ms. Delano’s admirers in the world of patient advocacy. Mr. Whitaker recalled acquaintances who, after setting out to quit their medications, fell into “despair.”
“Once you start going down that road, it becomes your identity,” said Mr. Whitaker. “People want to come off, and the next thing you know, there’s no service provider, no science, and they’re moving into that void.”
Numerous people in withdrawal communities described members who struggled with suicidal thinking, or who had died by suicide.
“More often than not, at least from what I’ve seen, once people conclude that the medications hurt them, then it’s all-or-nothing, black-and-white thinking,” said Kate Speer, a strategist for the Harvard T.H.Chan School of Public Health’s Center for Health Communication “They can’t recognize the providers are there to help, even when what they have done is not helpful.”
Ms. Delano said the issue of suicide comes up regularly in withdrawal communities. “I know so many people who have killed themselves over the years, in withdrawal or even beyond” she said. In 2023, a young woman who joined Inner Compass died by suicide, she said.
Afterward, Ms. Delano and Mr. Davis consoled distraught community members, who worried that they should have taken some action to intervene.
Ms. Delano said she would call 911 if a member overdosed on pills, but, short of that, she doesn’t weigh in on treatment choices. She noted that many members come to withdrawal groups precisely because they feel they have been harmed by the medical system.
“We have given psychiatry and licensed mental health professionals this godlike power to keep people alive,” she said. “Speaking for myself — this is not an organizational belief, but for me personally — I don’t think anyone should have that power over another human being.”
A ‘better me’
In Inner Compass gatherings, many people describe tapering processes as so difficult that they had to stop and reinstate medications. Some were on their fifth or sixth attempt, and some wept, describing how challenging it was.
Ms. Delano tries to keep the pressure off. “You’re in the driver’s seat,” she told one coaching client, who had reinstated a low dose of Valium. “It doesn’t mean, quote unquote, giving up or losing or failing.”
Daniel seemed to be looking for some inspiration to stick it out. He was getting better, he was sure of it, accessing levels of emotion that had been blunted by medication for 15 years.
He credited Ms. Delano for getting him this far; it was reading her story in the New Yorker that made him see it was possible to “come off the medications and be OK.” On a recent Zoom session, he showed her the Post-it note that he sometimes pulls out as a reminder to himself.
“IT WAS THE DRUGS,” he had written
“It was the drugs!” Ms. Delano exclaimed. She welled up toward the end of their session, reflecting on how much he had already achieved.
“The trade-off is worth it,” she told him. “The more your life expands — the meaning, the connection, the beauty, the possibility, the more that continues to expand in your life, the more all these beautiful things come online, the less weight, the less power the hard stuff has.”
When they hung up, he was feeling certain of his path again.
She has this effect on him, making him imagine how he will feel when he is off medication — “this better, more complete me,” as he put it. He thinks it will take two or three years to taper off completely.
If it proves too difficult, “I just have to take 450 milligrams and consider myself lucky,” he said. “But there is a desire to, you know, just kind of be free. Free of it.”
If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline or go to SpeakingOfSuicide.com/resources for a list of additional resources.

Science
What a Speech Reveals About Trump’s Plans for Nuclear Weapons

Within hours of the expiration last week of the final arms control treaty between Moscow and Washington, the State Department sent its top arms diplomat, Thomas G. DiNanno, to Geneva to lay out Washington’s vision for the future. His public address envisioned a future filled with waves of nuclear arms buildups and test detonations.
The views of President Trump’s administration articulated in Mr. DiNanno’s speech represent a stark break with decades of federal policy. In particular, deep in the speech, he describes a U.S. rationale for going its own way on the global ban on nuclear test detonations, which had been meant to curb arms races that in the Cold War had raised the risk of miscalculation, and war.
This annotation of the text of his remarks aims to offer background information on some of the specialized language of nuclear policymaking that Mr. DiNanno used to make his points, while highlighting places where outside experts may disagree with his and the administration’s claims.
What remains unknown is the extent to which Mr. DiNanno’s presentation represents a fixed policy of unrestrained U.S. arms buildups, or more of an open threat meant to spur negotiations toward new global accords on ways to better manage the nuclear age.
Read the original speech.
New York Times Analysis
Next »
1
Established in 1979 as Cold War arsenals grew worldwide, the Conference on Disarmament is a United Nations arms reduction forum made up of 65 member states. It has helped the world negotiate and adopt major arms agreements.
2
In his State Department role, working under Secretary of State Marco Rubio, Mr. DiNanno is Washington’s top diplomat for the negotiation and verification of international arms accords. Past holders of that office include John Bolton during the first term of the George W. Bush administration and Rose Gottemoeller during Barack Obama’s two terms.
3
This appears to be referring to China, which has 600 nuclear weapons today. By 2030, U.S. intelligence estimates say it will have more than 1,000.
4
Here he means Russia, which is conducting tests to put a nuclear weapon into space as well as to develop an underwater drone meant to cross oceans.
New York Times Analysis
« Previous Next »
5
In this year’s federal budget, the Trump administration is to spend roughly $90 billion on nuclear arms, including basic upgrades of the nation’s arsenal and the replacement of aging missiles, bombers and submarines that can deliver warheads halfway around the globe.
6
A chief concern of many American policymakers is that Washington will soon face not just a single peer adversary, as in the Cold War, but two superpower rivals, China and Russia.
New York Times Analysis
« Previous Next »
7
The 1987 Intermediate-Range Nuclear Forces Treaty or I.N.F. banned all weapons capable of traveling between 500 and 5,500 kilometers, or 310 and 3,420 miles, whether armed with nuclear or conventional warheads. The Trump administration is now deploying a number of conventionally armed weapons in that range, including a cruise missile and a hypersonic weapon.
8
The destructive force of the relatively small Russian arms can be just fractions of the Hiroshima bomb’s power, perhaps making their use more likely. The lesser warheads are known as tactical or nonstrategic nuclear arms, and President Vladimir V. Putin of Russia has repeatedly threatened to use them in Ukraine.
9
Negotiators of arms control treaties have mostly focused on long-range weapons because the delivery vehicles and their deadly warheads are considered planet shakers that could end civilization.
New York Times Analysis
« Previous Next »
10
This underwater Russian craft is meant to cross an ocean, detonate a thermonuclear warhead and raise a radioactive tsunami powerful enough to shatter a coastal city.
11
The nuclear power source of this Russian weapon can in theory keep the cruise missile airborne far longer than other nuclear-armed missiles.
12
Russia has conducted test launches for placing a nuclear weapon into orbit, which the Biden administration quietly warned Congress about two years ago.
13
The term refers to the five permanent members of the United Nations Security Council—China, France, Russia, the United Kingdom and the United States.
New York Times Analysis
« Previous Next »
14
A top concern of American officials is that Beijing and Moscow might form an alliance to coordinate their nuclear forces. Their joint program to develop fuel for atom bombs is seen as an indication of this emerging threat.
15
This Trump administration plan is dated November but was made public in December.
16
Released last year, this Chinese government document sought to portray Beijing as a leader in reducing the global threat of nuclear weapons.
17
Typically, arms control treaties have not required countries to destroy warheads so their keepers put them into storage for possible reuse. The United States retains something on the order of 20,000 small atom bombs meant to ignite the larger blasts of hydrogen bombs.
18
An imminent surge centers on the nation’s Ohio-class submarines. The Trump administration has called for the reopening of submarine missile tubes that were closed to comply with the New START limits. That will add as many 56 long-range missiles to the fleet. Because each missile can hold multiple arms, the additional force adds up to hundreds more warheads.
19
This refers to weapons meant for use on a battlefield or within a particular geographic region rather than for aiming at distant targets. It is often seen as synonymous with intermediate-range weapons.
20
Here, the talk turns to the explosive testing of nuclear weapons for safety, reliability and devising new types of arms. The United States last conducted such a test in 1992 and afterwards adopted a policy of using such nonexplosive means like supercomputer simulations to evaluate its arsenal. In 1996, the world’s nuclear powers signed a global ban on explosive testing. A number of nations, including the United States and China, never ratified the treaty, and it never officially went into force.
21
In new detail, the talk addresses what Mr. Trump meant last fall when he declared that he had instructed the Pentagon “to start testing our Nuclear Weapons on an equal basis” in response to the technical advances of unnamed foreign states.
22
Outside experts say the central issue is not whether China and Russia are cheating on the global test ban treaty but whether they are adhering to the U.S. definition. From the treaty’s start in 1996, Washington interpreted “zero” explosive force as the compliance standard but the treaty itself gives no definition for what constitutes a nuclear explosion. Over decades, that ambiguity led to technical disputes that helped block the treaty’s ratification.
23
By definition, all nuclear explosions are supercritical, which means they split atoms in chain reactions that become self-sustaining in sufficient amounts of nuclear fuel. The reports Mr. DiNanno refers to told of intelligence data suggesting that Russia was conducting a lesser class of supercritical tests that were too small to be detected easily. Russian scientists have openly discussed such small experiments, which are seen as useful for assessing weapon safety but not for developing new types of weapons.
24
This sounds alarming but experts note that the text provides no evidence and goes on to speak of preparations, not detonations, except in one specific case.
New York Times Analysis
« Previous
25
The talk gave no clear indication of how the claims about Russian and Chinese nuclear testing might influence U.S. arms policy. But it repeated Mr. Trump’s call for testing “on an equal basis,” suggesting the United States might be headed in that direction, too.
26
The talk, however, ended on an upbeat but ambiguous note, giving no indication of what Mr. DiNanno meant by “responsible.” Even so, the remark came in the context of bilateral and multilateral actions to reduce the number of nuclear arms in the world, suggesting that perhaps the administration’s aim is to build up political leverage and spur new negotiations with Russia, China or both on testing restraints.
Science
Notoriously hazardous South L.A. oil wells finally plugged after decades of community pressure

California Gov. Gavin Newsom announced this week that state oil and gas regulators have permanently closed one of the most infamous drill sites in Los Angeles, bringing an end to a decades-long community campaign to prevent dangerous gas leaks and spills from rundown extraction equipment.
A state contractor plugged all 21 oil wells at the AllenCo Energy drill site in University Park, preventing the release of noxious gases and chemical vapors into the densely populated South Los Angeles neighborhood. The two-acre site, owned by the Archdiocese of Los Angeles, is located across the street from several multifamily apartment buildings and less than 1,000 feet from St. Vincent School.
For years, residents and students had repeatedly complained about acrid odors from the site, with many suffering chronic headaches and nosebleeds. The health concerns prompted a community-driven campaign to shut down the site, with some residents even pleading (unsuccessfully) with the late Pope Francis to intervene.
AllenCo, the site’s operator since 2009, repeatedly flouted environmental regulations and defied state orders to permanently seal its wells.
This month, the California Department of Conservation’s Geologic Energy Management Division (CalGEM) finished capping the remaining unplugged wells with help from Biden-era federal funding.
“This is a monumental achievement for the community who have endured an array of health issues and corporate stalling tactics for far too long,” Newsom said in a statement Wednesday. “I applaud the tireless work of community activists who partnered with local and state agencies to finish the job and improve the health and safety of this community. This is a win for all Californians.”
The land was donated to the Catholic Archdiocese of Los Angeles in the 1950s by descendants of one of the city’s early oil barons. Over the decades, the archdiocese leased the land to several oil companies including Standard Oil of California.
Much of the community outcry over the site’s management occurred after AllenCo took over the site in 2009. The company drastically boosted oil production, but failed to properly maintain its equipment, resulting in oil spills and gas leaks.
In 2013, U.S. Environmental Protection Agency officials became sick while inspecting the site. The federal investigators encountered puddles of crude oil on the facility grounds, as well as caustic fumes emanating from the facility, resulting in violations for air quality and other environmental infractions.
In 2020, CalGEM ordered AllenCo to plug the wells after if determined the company had essentially deserted the site, leaving the wells unplugged and in an unsafe condition. AllenCo ignored the order.
In perhaps the most remarkable events in the site’s history, CalGEM officials in 2022 arrived on the site with a court order and used bolt cutters to enter the site to depressurize the poorly maintained oil wells.
The AllenCo wells were prioritized and plugged this week as part of a CalGEM program to identify and permanently cap high-risk oil and gas wells. Tens of thousands of unproductive and unplugged oil wells have been abandoned across California — many of which continue to leak potentially explosive methane or toxic benzene.
Environmental advocates have long fought for regulators to require oil and gas companies to plug these wells to protect nearby communities and the environment.
However, as oil production declines and fossil fuel companies increasingly become insolvent, California regulators worry taxpayers may have to assume the costs to plug these wells. Federal and state officials have put aside funding to deal with some of these so-called “orphaned” wells, but environmental advocates say it’s not enough. They say oil and gas companies still need to be held to account, so that the same communities that were subjected to decades of pollution won’t have to foot the bill for expensive cleanups.
“This is welcome news that the surrounding community deserves, but there is much more work to be done at a much faster pace,” said Cooper Kass, attorney at the Center for Biological Diversity’s Climate Law Institute. “There are still thousands of unplugged and hazardous idle wells threatening communities across the state, and our legislators and regulators should force polluters, not taxpayers, to pay to clean up these dangerous sites.”
Science
Newsom tells world leaders Trump’s retreat on the environment will mean economic harm

SACRAMENTO — Gov. Gavin Newsom told world leaders Friday that President Trump’s retreat from efforts to combat climate change would decimate the U.S. automobile industry and surrender the future economic viability to China and other nations embracing the transition to renewable energy.
Newsom, appearing at the Munich Security Conference in Germany, urged diplomats, business leaders and policy advocates to forcefully stand up to Trump’s global bullying and loyalty to the oil and coal industry. The California governor said the Trump administration’s massive rollbacks on environmental protection will be short-lived.
“Donald Trump is temporary. He’ll be gone in three years,” Newsom said during a Friday morning panel discussion on climate action. “California is a stable and reliable partner in this space.”
Newsom’s comments came in the wake of the Trump administration’s repeal of the endangerment finding and all federal vehicle emissions regulations. The endangerment finding is the U.S. government’s 2009 affirmation that planet-heating pollution poses a threat to human health and the environment.
Environmental Protection Agency administrator Lee Zeldin said the finding has been regulatory overreach, placing heavy burdens on auto manufacturers, restricting consumer choice and resulting in higher costs for Americans. Its repeal marked the “single largest act of deregulation in the history of the United States of America,” he said.
Scientists and experts were quick to condemn the action, saying it contradicts established science and will put more people in harm’s way. Independent researchers around the world have long concluded that greenhouse gases released by the burning of gasoline, diesel and other fossil fuels are warming the planet and worsening weather disasters.
The move will also threaten the U.S.’s position as a leader in the global clean energy transition, with nations such as China pulling ahead on electric vehicle production and investments in renewables such as solar, batteries and wind, experts said.
Newsom’s trip to Germany is just his latest international jaunt in recent months as he positions himself to lead the Democratic Party’s opposition to Trump and the Republican-led Congress, and to seed a possible run for the White House in 2028. Last month Newsom traveled to the World Economic Forum in Davos, Switzerland, and in November to the U.N. climate summit in Belém, Brazil — mocking and condemning Trump’s policies on Greenland, international trade and the environment.
When asked how he would restore the world’s confidence in the United States if he were to become president, Newsom sidestepped. Instead he offered a campaign-like soliloquy on California’s success on fostering Tesla and the nation’s other top electric vehicle manufacturers as well as being a magnet for industries spending billions of dollars on research and development for the global transition away from carbon-based economies.
The purpose of the Munich conference was to open a dialogue among world leaders on global security, military, economic and environmental issues. Along with Friday’s discussion on climate action, Newsom is scheduled to appear at a livestreamed forum on transatlantic cooperation Saturday.
Andrew Forrest, executive chairman of the Australia-based mining company giant Fortescue, said during a panel Friday his company is proof that even the largest energy-consuming companies in the world can thrive without relying on the carbon-based fuels that have driven industries for more than a century. Fortescue, which buys diesel fuel from countries across the world, will transition to a “green grid” this decade, saving the company a billion dollars a year, he said.
“The science is absolutely clear, but so is the economics. I am, and my company Fortescue is, the industrial-grade proof that going renewable is great economics, great business, and if you desert it, then in the end, you’ll be sorted out by your shareholders or by your voters at the ballot box,” Forrest said.
Newsom said California has also shown the world what can be done with innovative government policies that embrace electric vehicles and the transition to a non-carbon-based economy, and continues to do so despite the attacks and regressive mandates being imposed by the Trump administration.
“This is about economic prosperity and competitiveness, and that’s why I’m so infuriated with what Donald Trump has done,” Newsom said. “Remember, Tesla exists for one reason — California’s regulatory market, which created the incentives and the structure and the certainty that allowed Elon Musk and others to invest and build that capacity. We are not walking away from that.”
California has led the nation in the push toward EVs. For more than 50 years, the state enjoyed unique authority from the EPA to set stricter tailpipe emission standards than the federal government, considered critical to the state’s efforts to address its notorious smog and air-quality issues. The authority, which the Trump administration has moved to rescind, was also the basis for California’s plan to ban the sale of new gasoline-powered cars by 2035.
The administration again targeted electric vehicles in its announcement on Thursday.
“The forced transition to electric vehicles is eliminated,” Zeldin said. “No longer will automakers be pressured to shift their fleets toward electric vehicles, vehicles that are still sitting unsold on dealer lots all across America.”
But the efforts to shut down the energy transition may be too little, too late, said Hannah Safford, former director of transportation and resilience at the White House Climate Policy Office under the Biden administration.
“Electric cars make more economic sense for people, more models are becoming available, and the administration can’t necessarily stop that from happening,” said Safford, who is now associate director for climate and environment at the Federation of American Scientists.
Still, some automakers and trade groups supported the EPA’s decision, as did fossil fuel industry groups and those geared toward free markets and regulatory reform. Among them were the Independent Petroleum Assn. of America, which praised the administration for its “efforts to reform and streamline regulations governing greenhouse gas emissions.”
Ford, which has invested in electric vehicles and recently completed a prototype of a $30,000 electric truck, said in a statement to The Times that it appreciated EPA’s move “to address the imbalance between current emissions standards and consumer choice.”
Toyota, meanwhile, deferred to a statement from Alliance for Automotive Innovation president John Bozzella, who said similarly that “automotive emissions regulations finalized in the previous administration are extremely challenging for automakers to achieve given the current marketplace demand for EVs.”
-

 Alabama1 week ago
Alabama1 week agoGeneva’s Kiera Howell, 16, auditions for ‘American Idol’ season 24
-

 Culture1 week ago
Culture1 week agoVideo: Farewell, Pocket Books
-

 Illinois7 days ago
Illinois7 days ago2026 IHSA Illinois Wrestling State Finals Schedule And Brackets – FloWrestling
-

 Technology1 week ago
Technology1 week agoApple might let you use ChatGPT from CarPlay
-

 Politics1 week ago
Politics1 week agoHegseth says US strikes force some cartel leaders to halt drug operations
-

 World1 week ago
World1 week ago‘Regime change in Iran should come from within,’ former Israel PM says
-

 Movie Reviews1 week ago
Movie Reviews1 week agoWith Love Movie Review: A romcom with likeable leads and plenty of charm
-
News1 week ago
Hate them or not, Patriots fans want the glory back in Super Bowl LX