Science
L.A. County has its first measles case since 2020: What to do if you're exposed
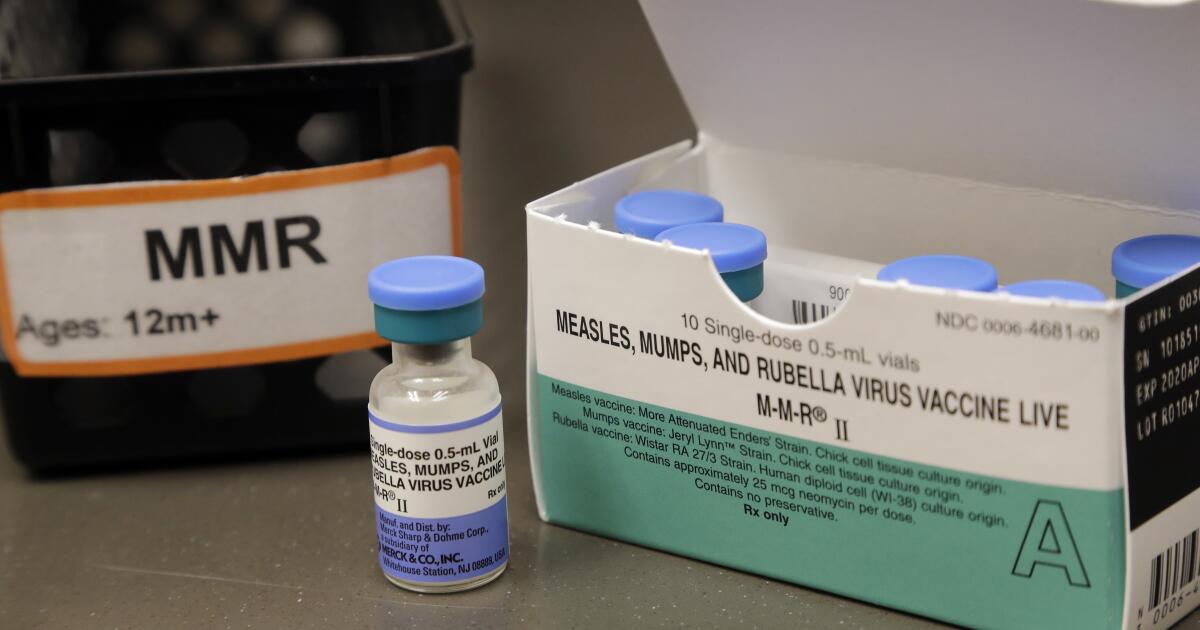
A recently arrived traveler at Los Angeles International Airport is the source of the first case of measles in L.A. County since 2020.
Measles is a highly infectious disease, and health experts say the best way to evade infection is immunization.
The Los Angeles resident was a passenger on a Turkish Airlines flight that arrived at 5 p.m. Jan. 25 at the Tom Bradley International Terminal, Gate 157. Anyone who was at Terminal B from 5 to 9 p.m. may have been exposed and could be at risk of developing measles.
L.A. public health officials are notifying Turkish Airlines passengers who sat close to this flier about possible measles exposure.
The measles virus can live in the air for up to two hours after an infected person has left the area, according to the U.S. Centers for Disease Control and Prevention, which works with the L.A. Department of Public Health to investigate communicable disease exposure on international flights to the U.S.
Following the flight, the infected person made a stop at a Northridge Chick-fil-A.
Patrons who were at the restaurant at 18521 Devonshire St. between 8 and 10:30 p.m. may be at risk of developing measles, county health officials said.
Additional locations where possible exposures may have occurred are being investigated by the health department.
“Measles is spread by air and by direct contact,” said Muntu Davis, Los Angeles County health officer, in a news release. “Even before you know it, you have it, and [it] can lead to severe disease.”
Those who haven’t been immunized against measles, or are not sure whether they’ve had the vaccine, and were at these sites during the date and times listed above are at risk of developing measles. Symptoms appear from seven to 21 days after exposure to the virus. Those who have been free of symptoms for more than 21 days are no longer at risk.
The CDC reported a recent rise in domestic measles cases. Between Dec. 1 and Jan. 23, the agency was notified of 23 confirmed U.S. cases of measles, including seven direct importations of measles by international travelers and two outbreaks with more than five cases each.
If you think you were exposed
Public health officials recommend:
- Review your immunization and medical records to determine whether you’re protected against measles. People who have not had measles infection or received the measles immunization previously may not be protected from the virus and should talk with a healthcare provider about receiving the measles, mumps and rubella immunization.
- Contact and notify your healthcare provider as soon as possible about a potential exposure if you’re pregnant, if you have an unvaccinated infant who may have been exposed or if you have a weakened immune system.
- Monitor yourself for illness: a fever and/or an unexplained rash from seven days to 21 days after exposure.
- If symptoms develop, stay at home and avoid school, work and any large gatherings. Call a healthcare provider immediately. Do not enter a healthcare facility before calling and making the provider aware of your measles exposure and symptoms.
Last month, the CDC released an alert for healthcare providers for measles cases after there were 23 confirmed cases throughout the U.S.
The best way to prevent measles infection is by getting the MMR vaccine, which covers measles, mumps and rubella. Children need two vaccine doses, one when they are 12 to 15 months old and the second between the ages of 4 and 6. Teenagers and adults who have not yet been immunized need one dose.
How measles can spread
The virus is highly contagious and lives in the nose and throat mucus of an infected person, according to the CDC. It can spread through coughing and sneezing.
The CDC says the virus is so contagious that if one person has it, up to 90% of the people who are not immune and are in close proximity to that person will also become infected.
Measles can also spread when other people breathe the contaminated air or touch an infected surface, then touch their eyes, nose or mouth.
The infection can be spread four days before symptoms begin or four days after signs of the virus.
Measles symptoms
The first symptoms of measles infection will appear in seven to 14 days of contracting the infection.
We know measles as a rash on the skin, but it can be dangerous especially for babies and young children. Measles typically begins with high fever (which could spike to more than 104 degrees), cough, runny nose and red, watery eyes.
Two to three days after symptoms begin, tiny white spots may appear inside the mouth.
In three to five days after having symptoms of measles infection, a rash breaks out. It usually begins as flat red spots that appear on the face and at the hairline, then spreads downward to the back, trunk, arms, legs and feet.

Science
Opinion: Most older Americans who need hearing aids don't use them. Here's how to change that

Having depended on hearing aids for nearly three decades, I’m astounded by the lack of Medicare coverage for devices that can solve a problem afflicting tens of millions of older Americans.
Nearly two-thirds of Americans over age 70 have some degree of hearing loss, and over half of those 75 and older experience impairment serious enough to be considered disabling. But most don’t wear hearing aids.
Because the legislation that created Medicare nearly 60 years ago specifically excluded hearing aids, those who rely on the program’s traditional coverage must pay for them out of pocket. That expense is among the chief barriers to wider use of the devices.
Age-related hearing loss impedes basic communication and the relationships that depend on it. Expanded access to hearing aids could therefore do no less than enable more older Americans to establish and maintain the social connections that are essential to a meaningful life.
Hearing loss is like an invisible, muffling curtain that falls in front of anyone speaking. Asking people to repeat themselves can yield irritated and hurtful responses. And it’s hopeless to ask a soft-spoken person to speak up. Sometimes it’s easier just to nod and smile.
Many older people I know choose to avoid social gatherings altogether because they can’t hear well. Without hearing aids, I’d stay home too.
Hearing loss can harm one’s health in other ways. For example, I’ve written about the need for a comprehensive approach to reducing cancer risk at older ages, including preventive services such as colorectal cancer screening. But these services rely on conversations between patients and their healthcare providers. An older patient’s ability to hear and understand such conversations shouldn’t be taken for granted or ignored.
The Food and Drug Administration did improve access to hearing aids by making some of them available without a prescription in 2022, but the over-the-counter devices are inadequate for serious hearing loss like mine. My private health insurance, meanwhile, started covering hearing aids a few years ago, providing up to $2,500 for them every five years. One hearing aid alone can cost that much or more, however.
Despite its limitations, my private coverage for hearing aids is better than nothing, which is what traditional Medicare provides.
Hearing loss is more common among lower-income people and those without advanced education. The toll from noisy workplaces compounds age-related hearing loss for some. One analysis found that most Americans with a serious hearing disability can’t afford the typical price of hearing aids.
Many of the older adults who can’t come up with these significant out-of-pocket expenses spent their working years in low-wage jobs that our country depends on. Denying them treatment for their hearing loss is a lousy way to treat people who gave years of service to our society.
Although some older adults with hearing loss won’t benefit from hearing aids, Medicare coverage for the devices might encourage more beneficiaries to get their hearing tested so they can get the treatment that’s right for them. And while Medicare coverage alone won’t address the stigma some people associate with hearing aids, the availability of newer, more comfortable and less obvious technology might win over some refuseniks.
Legislation reintroduced with bipartisan support last year would finally correct this glaring gap in Medicare coverage by removing the hearing aid exclusion from the law. There’s no reason to delay action on this any longer. Are our representatives listening?
Mary C. White is an adjunct professor of environmental health at Emory University’s Rollins School of Public Health, a Public Voices fellow at AcademyHealth in partnership with the OpEd Project and a former federal epidemiologist.
Science
Second human case of bird flu detected in Michigan dairy worker

A second human case of bird flu in a diary worker has been confirmed in Michigan, state and federal health officials announced Wednesday.
The symptoms were mild, consisting of conjunctivitis. The Texas dairy worker who contracted the virus in March also came down with pink eye.
At a press call on Wednesday, Nirav Shah, principal deputy director of the U.S. Centers for Disease Control and Prevention, said the finding was “not unexpected” and that it was a scenario “that we had been preparing for.”
He said that since the discovery of H5N1 in dairy cattle, state and federal health officials have been closely monitoring farmworkers and slaughterhouse workers and urging farmers and farmworker organizations to “be alert, not alarmed.”
Federal officials say they still believe the human health risk of bird flu is low; however, it underscores the need for people who are interacting with infected or potentially infected farm animals or birds to take precautions, including avoiding dead animals and wearing personal protective equipment (PPE) if there’s a need to be in close contact.
Though a nasal swab from the person in Michigan tested negative for influenza, an eye swab from the patient was shipped to the CDC and tested positive for influenza A(H5N1) virus.
This is the third case of H5N1 reported in the United States. A poultry worker in Colorado was identified in 2022.
Although the symptoms in the three farmworkers in the U.S. have been mild, people elsewhere in the world have suffered more severe illness, including death. According to the World Health Organization, between Jan. 1, 2003, and March 28, 2024, there have been 888 cases of human infection from 23 countries; 463 were fatal.
In preparation for a more widespread outbreak, the CDC updated its guidance for PPE in dairies and issued a nationwide order for healthcare providers to be on the lookout for novel influenza.
On Tuesday, the CDC asked clinical laboratories and health departments to increase the number of influenza samples being analyzed “to maximize the likelihood of catching a case of H5N1 in the community,” Shah said.
The US Department of Agriculture is also expanding its surveillance and support by providing $1500 to non-infected farms to beef up biosecurity, and $100 to producers who want to buy inline samplers to test their milk. The agency will also provide $2000 per farm to cover veterinary fees for testing, as well as shipping costs to send those tests to laboratories for analysis.
There have been no cases of H5N1 detected in California’s dairy herds.
Officials said ongoing analysis of the nation’s dairy supply suggests it is safe to consume, Despite the risk to human health being low, an official with the Administration for Strategic Preparedness and Response said it will make Tamiflu available upon request “to jurisdictions that do not have their own stockpile and are responding to pre-symptomatic persons with exposure to confirmed or suspected infected birds, cattle or other animal exposures.”
Dawn O’Connell, assistant secretary of the preparedness agency, said it started the “fill and finish” process for approximately 4.8 million doses of vaccine “that is well matched to the currently circulating strain of H5N1 through the national pre-pandemic influenza vaccine stockpile program.”
She said the decision to get started on H5N1 vaccines was not a response to any heightened concern, but since it takes several months to fill and finish vaccine doses, the agency “thought it made sense given what we were seeing.”
Science
Gas stoves may contribute to early deaths and childhood asthma, new Stanford study finds

Lung-irritating pollution created by cooking with gas stoves may be contributing to tens of thousands of premature deaths and cases of childhood asthma in the United States, according to a new study published in the journal Science Advances.
For decades, scientists have known the flames from a gas stovetop produce nitrogen dioxide, a pungent gas that can inflame a person’s lungs when inhaled. But for the first time, a team of researchers from Stanford University and Oakland-based research institute PSE Healthy Energy published a nationwide estimate of the long-term health consequences associated with cooking with natural gas and propane stoves.
Researchers concluded that exposure to nitrogen dioxide emissions alone may contribute to nearly 19,000 premature deaths in the United States each year. It has also resulted in as many as 200,000 current cases of pediatric asthma compared with cooking with electric stoves, which do not produce nitrogen dioxide.
Aggressive and impactful reporting on climate change, the environment, health and science.
Stanford researcher Yannai Kashtan noted higher levels of pollution were correlated with the amount of gas that was burned. But pollution also accumulated at higher levels inside smaller homes.
“If you live in a smaller house, you’re exposed to more pollution, and that can lead to income and racial disparities in exposure,” Kashtan said. “In general, folks living in neighborhoods with higher levels of outdoor pollution also tend to have higher indoor pollution. So this environmental injustice extends indoors as well.”
The American Gas Assn., a trade organization representing more than 200 local energy companies nationwide, dismissed the findings as “misleading and unsupported.”
“Despite the impressive names on this study, the data presented here clearly does not support any linkages between gas stoves and childhood asthma or adult mortality,” the association’s president and CEO, Karen Harbert said in a statement earlier this month.
The study is the latest examining the serious health effects associated with breathing fumes from gas stoves, which release planet-warming carbon emissions and a variety of air pollutants. In recent years, the popular household appliance has become a political hot-button issue as policymakers and regulators have weighed environmental impacts against consumer choice.
Many large cities in California, including Los Angeles, have moved toward phasing out gas stoves in newly constructed residences. Earlier this month, the California Assembly advanced a bill to the Senate that would require gas stoves to come with warning labels detailing the pollution and health effects that can arise from cooking with gas.
Gas stoves emit a variety of pollutants, including asphyxiating carbon monoxide, cancer-causing formaldehyde and benzene. The flame also creates nitrogen dioxide, a precursor to smog and a pollutant that can cause difficulty breathing.
Environmental groups say consumers should be notified about these pollutants and the potential harm they can cause.
“Gas stoves create pollution in our homes, increasing the risk of childhood asthma and other respiratory problems for our families,” said Jenn Engstrom, state director for California Public Interest Research Group. “However, this risk has largely been hidden from the public. Consumers deserve the truth when it comes to the danger of cooking with gas. Warning labels will give consumers what they need to make informed decisions when they purchase appliances for their homes.”
Kashtan and other researchers had previously discovered cooking with gas stoves presented a similar cancer risk as inhaling second-hand cigarette smoke. They also found some gas stoves leaked contaminants even when the burners were off.
The effects are especially devastating to children, whose smaller and still-developing lungs need to take more breaths than adults, Kashtan said. Older adults, especially those with cardiovascular or respiratory illness, are also more vulnerable to pollution from gas stoves.
To alleviate indoor air pollution, experts recommend using ventilation hoods and opening windows while cooking,
Starting in 2008, California required new and redeveloped homes to have ventilation that could prevent pollution from building up indoors. But during their research, measuring emissions in more than 100 households across the country, Yannai said they found many kitchens didn’t have ventilation hoods at all.
Although the health effects of breathing these pollutants are clear, researchers still wonder to what degree these conditions could be reversible. As communities take steps to mitigate their exposure or transition away, he said we could soon see the results.
“It’s never too late to stop breathing in pollution,” he said.
-

 Politics1 week ago
Politics1 week agoDem newcomer aims for history with primary win over wealthy controversial congressman
-

 Politics1 week ago
Politics1 week agoSouthern border migrant encounters decrease slightly but gotaways still surge under Biden
-

 World1 week ago
World1 week agoSlovakia PM Robert Fico in ‘very serious’ condition after being shot
-

 World1 week ago
World1 week agoCanadian Nobel-winning author Alice Munro dies aged 92
-

 Politics1 week ago
Politics1 week agoVulnerable Dem incumbents move to the center in key swing states as Biden panders to far-left base
-

 News1 week ago
News1 week agoDespite state bans, abortions nationwide are up, driven by telehealth
-

 World1 week ago
World1 week ago‘Monstrous crime’: World reacts to attack on Slovakia’s prime minister
-

 News1 week ago
News1 week agoSmall but mighty Nimble becomes first mixed-breed dog to win Westminster agility title