Health
Scientists Debut Lab Models of Human Embryos

In its first week, a fertilized human egg develops into a hollow ball of 200 cells and then implants itself on the wall of the uterus. Over the next three weeks, it divides into the distinct tissues of a human body.
And those crucial few weeks remain, for the most part, a black box.
“We know the basics, but the very fine details we just don’t know,” said Jacob Hanna, a developmental biologist at the Weizmann Institute of Science in Israel.
Dr. Hanna and a number of other biologists are trying to uncover those details by creating models of human embryos in the lab. They are coaxing stem cells to organize themselves into clumps that take on some of the crucial hallmarks of real embryos.
This month, Dr. Hanna’s team in Israel, as well as groups in Britain, the United States and China, all released reports on these experiments. The studies, while not yet published in scientific journals, have attracted keen interest from other scientists, who have been hoping for years that such advances could finally shed light on some of the mysteries of early human development.
Ethicists have long cautioned that the advent of embryo models would further complicate the already complicated regulation of this research. But the scientists behind the new work were quick to stress that they had not created real embryos and that their clusters of stem cells could never give rise to a human being.
“Our aims are never for the purpose of human reproduction,” said Tianqing Li, a developmental biologist at Kunming University of Science and Technology in China, who led one of the new studies.
Instead, Dr. Li and his fellow scientists hope that embryo models will lead to new treatments for infertility and even diseases such as cancer.
“We do it to save lives, not create it,” said Magdalena Zernicka-Goetz, a developmental biologist at the University of Cambridge and the California Institute of Technology, who led another effort.
For decades, the only human embryos that developmental biologists could study were specimens collected from miscarriages or abortions. As a result, scientists were left with profound questions about the start of human development. Thirty percent of pregnancies fail in the first week, and another 30 percent fail during implantation. Researchers have been at a loss to explain why a majority of embryos don’t survive.
After the development of in vitro fertilization in the 1970s, scientists began studying embryos donated from fertility clinics. Some countries banned the research, while others allowed it to proceed, typically with a 14-day limit. By then, the human embryo starts taking on some of its key features. A structure called the primitive streak, for example, organizes the head-to-foot arrangement that the body will take.
For years, the 14-day rule was a moot point because no one could keep embryos alive more than a few days after fertilization. Things became more complicated in 2016, when Dr. Zernicka-Goetz’s group and another team managed to keep embryos alive close to the 14-day mark. The embryos did not survive longer because the scientists destroyed them.
The accomplishment has led scientists to debate the possibility of allowing embryos to grow past 14 days. But even if those experiments were to become legal, they would still be hard to carry out because the supply of donated embryos is scarce.
In recent years, researchers have been looking for an easier way to study embryos: by making models of them in the lab. The scientists have taken advantage of the fact that stem cells, given the right environmental conditions, can turn into new kinds of tissues.
Adults have stem cells in only a few parts of the body. In the skin, for example, stem cells produce a range of new cells that heal wounds. In early embryos, on the other hand, all the cells have the potential to turn into a wide variety of tissues.
Last year, Dr. Zernicka-Goetz’s team and Dr. Hanna’s team used embryonic stem cells from mice to make models of embryos. Since then, they and other scientists have been trying to do the same with human embryonic stem cells.
Each team has used a different method, but they all take advantage of the same underlying biology. By the time a human embryo implants itself in the uterus, its cells have started to diverge into different types. One type of cell will go on produce the cells of the body. The other types will produce tissues that surround the embryo during development, such as the placenta. These cell types send out molecular signals to each other that are essential for their development.
The researchers coaxed stem cells to mimic some of these cell types and then mixed them together. The cells swarmed together and spontaneously organized into clusters. The cells destined to become the embryo huddled in the middle, while the other types migrated to the outside.
As the cells communicated to each other, they divided and formed new structures that resembled parts of embryos. Dr. Mo Ebrahimkhani, a developmental biologist at the University of Pittsburgh, and his colleagues observed the formation of a yolk sac in their experiment, for example. Out of the yolk sac, they even observed the development of progenitors of blood cells.
Dr. Zernicka-Goetz and her colleagues likewise watched the development of cells that resembled the precursors of eggs and sperm.
“This was absolutely thrilling,” Dr. Zernicka-Goetz said. “It’s sometimes hard to believe that these stem cells are growing into these structures.”
If scientists can create close, reliable models of embryos, they will be able to run large-scale experiments to test potential causes of pregnancy failures, such as viral infections and genetic mutations.
The models could lead to other medical advances too, noted Insoo Hyun, a member of the Harvard Medical School Center for Bioethics who was not involved in the new studies.
“Once you get the embryo models in place and you can rely on them, that can be an interesting way to screen drugs that women take when they’re pregnant,” he said. “That would be an enormous benefit.”
Dr. Hanna and Dr. Ebrahimkhani also saw a possibility of using embryo models as a new form of stem-cell treatment for diseases such as cancer.
In conventional stem-cell transplants, doctors remove blood stem cells from the bone marrow before killing cancer cells with radiation or chemotherapy. They then return the healthy cells to the body.
Unfortunately, this method does not have a high success rate. Some researchers have suggested that earlier forms of stem cells would be more likely to cure patients.
Embryo models might make it possible for doctors to turn back time. Researchers would take skin cells from a patient and douse them with chemicals to put them into a stem-cell-like state. With other chemical baths, those stem cells could then be turned into an embryo model, which could in turn develop into the early blood cells the patient needs after a transplant.
Alysson Muotri, a developmental biologist at the University of California San Diego who was not involved in the new studies, cautioned that the new studies demonstrated only a preliminary step. For one thing, while the techniques sometimes resulted in embryolike clusters, they often failed.
“The work is in very early stages, and the current methods are far from reliable,” Dr. Muotri said.

Health
Better Than Ozempic? Doctors Say These Medications Are Better for Weight Loss Than the Popular Semaglutide

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Forgot your password?
Get back to the Sign In
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Honeybees can detect lung cancer, researchers say
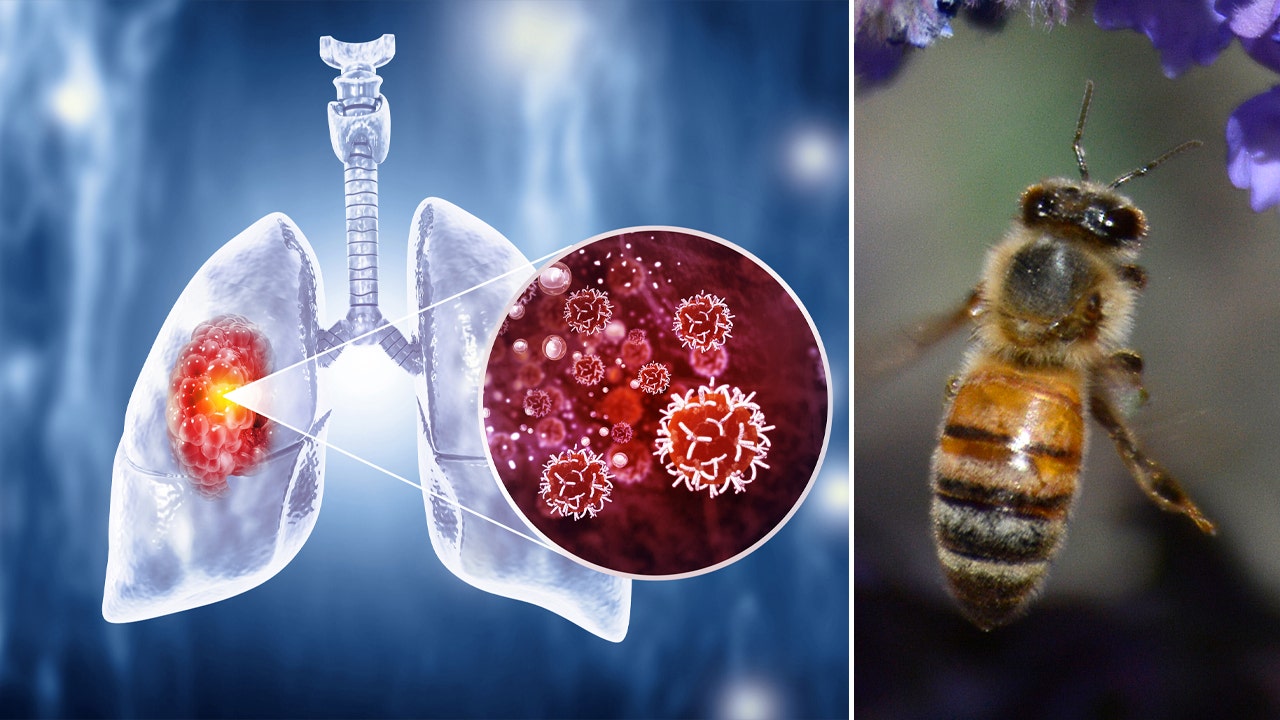
What happens when you pair honeybees and halitosis? Potentially a life-saving new method to screen for cancer, according to one study.
Researchers at Michigan State University have learned that honeybees can detect chemicals associated with lung cancer in human breath. The insects were able to sniff out human lung cancer biomarkers with a remarkable 82% success rate, according to a study published in the journal Biosensors and Bioelectronics.
“These results indicate that the honeybee olfactory system can be used as a sensitive biological gas sensor to detect human lung cancer,” the study authors wrote.
“Insects have an amazing sense of smell the same way dogs do,” said MSU professor Debajit Saha, according to an MSU news release.
YOUNG VAPER WHO REQUIRED DOUBLE LUNG TRANSPLANT SHARES WARNINGS AS E-CIGARETTE SALES RISE
A honeybee drinking nectar from a flower in Markham, Ontario, Canada. (Creative Touch Imaging Ltd./NurPhoto via Getty Images)
Saha, an assistant professor in the College of Engineering and MSU’s Institute for Quantitative Health Science and Engineering, sought to determine whether honeybees could distinguish chemicals in a healthy person’s breath from that of someone sick with lung cancer.
His team developed a “recipe” for a synthetic breath mixture that contained six compounds present in the breath of someone with cancer and a synthetic “healthy” breath mixture.
“It took a steady hand to create the recipe,” said Elyssa Cox, Saha’s former lab manager. “We tested the synthetic lung cancer versus healthy human breath mixtures on approximately 20 bees.”
The researchers placed each live bee in a custom 3D-printed harness and attached a tiny electrode to its brain to measure activity.
SOME BREAST CANCER PATIENTS COULD BE AT RISK OF ANOTHER TYPE OF CANCER, STUDY REVEALS

Lung cancer is the leading cause of cancer death worldwide. An estimated 235,580 people will be diagnosed with lung cancer in 2024 in the U.S., according to the Lung Cancer Research Foundation. (Mohammed Haneefa Nizamudeen/iStock)
“We pass those odors on to the antenna of the honeybees and recorded the neural signals from their brain,” said Saha. “We see a change in the honeybee’s neural firing response.”
The researchers found that the bees were able to detect the cancer-indicating compounds even in small amounts.
“The honeybees detected very small concentrations; it was a very strong result,” said Saha. “Bees can differentiate between minute changes in the chemical concentrations of the breath mixture, which is in the parts per 1 billion range.”
The bees also could tell the difference between the synthetic lung cancer breath and healthy breath.
UK TO INTRODUCE BILL TO PHASE OUT LEGAL SALE OF TOBACCO

A honey bee visits a blooming catmint plant growing in Santa Fe, New Mexico. (Robert Alexander/Getty Images)
Scientists hope this research will lead to the development of a sensor based on a honeybee brain that can be used to test human breath for the presence of lung cancer.
“What’s amazing is the honeybees’ ability to not only detect cancer cells, but also distinguish between cell lines of various types of lung cancer,” said Autumn McLane-Svoboda, a graduate student on Saha’s team. “The future implications for this are huge, as our sensor could allow for patients to receive specific cancer diagnoses quickly, which is imperative for correct treatment routes.”
Lung cancer is the leading cause of cancer death worldwide. An estimated 235,580 people will be diagnosed with lung cancer in 2024 in the U.S., according to the Lung Cancer Research Foundation.
Smoking is the leading risk factor for lung cancer and is responsible for 80% of lung cancer deaths.
Early detection of high-risk lung cancer can reduce the chance of death by up to 20%.
Health
COVID vaccine companies told to focus on KP.2 variant for fall shots, per FDA announcement

The U.S. Food and Drug Administration (FDA) has recommended that COVID vaccine manufacturers update their formulas for fall doses, in an attempt to target the KP.2 strain of the JN.1 variant.
The Thursday announcement came just a week after the agency’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) voted to recommend a “monovalent JN.1-lineage vaccine” at its June 5 meeting.
As of the end of March 2024, the KP.2 variant was responsible for just 4% of infections in the U.S., according to the COVID Data Tracker from the Centers for Disease Control and Prevention (CDC).
CDC WARNS OF ‘DUAL MUTANT’ FLU STRAIN THAT COULD EVADE ANTIVIRAL DRUGS: ‘NEED TO CLOSELY MONITOR’
Meanwhile, over 50% of infections at that time were attributed to its parental strain, JN.1.
Just a few weeks later, KP.2 is now the cause of around 28% of infections, while the JN.1 variants have largely dropped in prevalence, the tracker shows.
The U.S. Food and Drug Administration has recommended that COVID vaccine manufacturers update their formulas for fall doses, in an attempt to target the KP.2 strain of the JN.1 variant. (iStock)
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, recently spoke with Dr. Peter Marks, director of the Center for Biologics Evaluation and Research (CBER) at the Food and Drug Administration, about the new vaccine formulations.
“It makes sense to target the KP.2 strain because it is becoming the predominant strain — it is surging in California and will spread across the country,” Siegel told Fox News Digital.

KP.2 is now the cause of around 28% of infections, while the JN.1 variants have largely dropped in prevalence, CDC Tracker data shows. (iStock)
The KP.2 strain is “highly immunoevasive,” the doctor warned — which means that immunity from previous variants and subvariants don’t offer much protection.
COVID-FLU COMBO VACCINE SHOWS ‘POSITIVE’ RESULTS IN PHASE 3 TRIALS, MODERNA SAYS: A ‘TWO-FOR’ OPTION
“On the other hand, the vaccine will cause a production of immune cells and antibodies that will continue to protect you against previous variants and subvariants,” Siegel added.

The updated vaccine is especially important for high-risk groups, those who have chronic illnesses, the elderly and anyone who comes in contact with them, according to doctors. (iStock)
It is especially important for high-risk groups, those who have chronic illnesses, the elderly and anyone who comes in contact with them, according to the doctor.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
In a statement to Fox News Digital, vaccine maker Novavax — which makes protein-based vaccines — said the company “just filed” its application for a JN.1 COVID vaccine.
A vial of the Phase 3 Novavax coronavirus vaccine is seen ready for use in the trial at St. George’s University hospital in London, on Oct. 7, 2020. (AP Photo/Alastair Grant, File)
“Novavax’s updated JN.1 COVID-19 vaccine is active against current circulating strains, including KP.2 and KP.3,” the company said in a press release.
“The submission is in line with guidance from the U.S. FDA, European Medicines Agency (EMA) and the World Health Organization (WHO) to target the JN.1 lineage this fall.”
For more Health articles, visit www.foxnews/health.
Fox News Digital reached out to Pfizer and Moderna — both of which produce mRNA-based vaccines — requesting comment on their plans for fall formulations.
-

 News1 week ago
News1 week agoIsrael used a U.S.-made bomb in a deadly U.N. school strike in Gaza
-

 World1 week ago
World1 week agoWorld leaders, veterans mark D-Day’s 80th anniversary in France
-

 World1 week ago
World1 week agoFrance to provide Ukraine with its Mirage combat aircraft
-

 World1 week ago
World1 week agoRussia-Ukraine war: List of key events, day 833
-

 Movie Reviews1 week ago
Movie Reviews1 week agoInsane Like Me? – Review | Vampire Horror Movie | Heaven of Horror
-

 News1 week ago
News1 week agoNonprofit CFO Accused of 'Simply Astonishing' Fraud
-

 Politics1 week ago
Politics1 week agoGeorge Clooney called White House to complain about Biden’s criticism of ICC and defend wife’s work: report
-
 Politics1 week ago
Politics1 week agoNewson, Dem leaders try to negotiate Prop 47 reform off California ballots, as GOP wants to let voters decide















