Health
Is the New 988 Suicide Hotline Working?

The contestants on “Celebrity Jeopardy!” were stumped in the fall when asked about the new “3-digit national hotline phone number for suicide prevention” in the United States, which debuted last July.
“What is 311?” the comedian Iliza Shlesinger guessed, wrongly.
As it turns out, she was not alone. It has been one year since the National Suicide Prevention Lifeline underwent a transformation, recasting its 10-digit number as 988, yet many people are unaware of the change or what the hotline provides.
The new number is supposed to make it easier for callers to connect with help when they’re having suicidal thoughts, experiencing emotional distress or having a substance-use-related crisis, but only 17 percent of Americans say they are very or somewhat familiar with it, according to a survey released on Thursday by the National Alliance on Mental Illness. In addition, the survey found, people are still confused about what to expect when they call.
Many still assume that “you call 988 and — much like 911 — that means someone is going to be dispatched to you,” said Hannah Wesolowski, NAMI’s chief advocacy officer. “For the vast majority — almost all callers — that’s not actually the case.”
Here’s a look at what everyone should know about 988 and the challenges that lie ahead in continuing to fund and expand the network.
What should you know about 988?
The three-digit dialing code for the 988 Suicide and Crisis Lifeline became available in July of last year after receiving bipartisan support. (President Donald J. Trump signed the law establishing the new number in 2020.) Since then, more than five million calls, chats and texts have been routed to 988, a 66 percent increase from the previous 12 months, before the arrival of the new number.
Almost one million of those contacts were answered by Veterans Crisis Line, which is linked to 988.
According to the survey, most people either assume that calling 988 will automatically dispatch emergency services such as the police, or aren’t sure, but in reality, less than 2 percent of Lifeline calls require a connection to services like 911. In fact, 988 does not currently use geolocation, so those who call the hotline remain anonymous unless they choose to disclose identifying information. Part of the impetus behind creating 988 was to reduce the reliance on law enforcement or emergency departments to handle mental health crises, and instead to build an expanded group of services, the Substance Abuse and Mental Health Services Administration has said. In some areas, that includes mobile crisis teams and stabilization centers, which offer people a place to go that isn’t an emergency room.
But you don’t need to be in crisis or suicidal to call 988 and speak with a counselor. It is a free service available at all hours, day or night, for anyone who needs support.
“It’s our hope that people will come to us before they are in a mental health crisis,” said Tia Dole, chief officer of the 988 Suicide and Crisis Lifeline at Vibrant Emotional Health, the New York-based nonprofit that manages the Lifeline for SAMHSA.
Why do so few people know about it?
The NAMI survey found that most Americans did not know crucial facts about the Lifeline or what to expect if they call.
This is partly by design. Over the last year, none of the Lifeline’s nearly $1 billion in federal funding was allocated toward a public relations campaign. Initially, advocates and administrators alike worried that promoting 988 too early might cause it to become overwhelmed by demand.
But the time has come to raise broader awareness, Dr. Dole said. Vibrant is aiming to start a campaign in the fall that will not only get the word out but also attempt to decrease some of the disparities among those who understand and embrace 988.
According to NAMI, for example, Black people and adults 50 and older were the least likely to have heard of 988. A Pew study released in April found similar results, and uncovered disparities along economic lines as well: People who were more affluent or had higher levels of education were also more likely to be aware of 988.
What other hurdles remain?
Aside from increasing public awareness, one of the biggest problems facing the expanded network is long-term funding.
The national network has more than 200 call centers, mostly composed of nonprofits with small budgets. Many rely on volunteers and private contributions.
The law that established 988 gave state lawmakers the option of raising money for call centers by adding a monthly fee on phone bills. But so far only a handful of states have done so.
The Biden administration’s 2024 budget proposal includes $836 million for 988, an increase of more than $300 million from the amount allocated last year to get the Lifeline up and running. But experts say more is needed, particularly at the local and state levels.
In the coming year, the number of calls, texts and chats that come to 988 could be as high as nine million, almost double the number of contacts in the first year, said Bob Gebbia, the chief executive of the American Foundation for Suicide Prevention.
“That’s an enormous increase, and we want to make sure that there’s someone there to answer the calls and texts and chats,” he said. “We need to have additional funding.”
The expansion of the network is further complicated by a shortage in behavioral health professionals. When local centers cannot pick up, calls are pushed to national backup centers, which can result in higher wait times or cause callers to simply hang up.
Finally, the current method of routing callers by area code can be problematic if someone’s phone number doesn’t reflect where they currently live. Crisis counselors who assist people who live in other states may have more difficulty offering local referrals.
What is the Lifeline doing right?
The Lifeline encountered record demand in the last year, but it managed to reduce the wait time for a response from a counselor.
“This means that more people are getting help and they are getting help more quickly, which is crucial for a person in crisis,” Miriam E. Delphin-Rittmon, the leader of SAMHSA, said in a statement on Thursday.
Before 988 was implemented, it might take several minutes to reach someone. Now the average response time has decreased from 2 minutes and 39 seconds to 41 seconds, according to SAMHSA. The wait time can vary substantially, however, depending on the location or time of day.
Another big change: The new Lifeline has invested in answering texts and chats. In the past the Lifeline had the capacity to handle only 56 percent of text messages and 30 percent of chats. So far recent data indicates that the new Lifeline is answering a much higher proportion of chats and texts on average.
Overall, “I am convinced it is helping to save lives,” Mr. Gebbia said of 988.
What’s next?
Demand for the Lifeline is expected to surge in the years ahead as mental illness continues to be a large public health problem. Anxiety and depression are widespread, particularly among young adults: A KFF analysis of census data found that half of adults ages 18 to 24 reported anxiety and depression symptoms in 2023, compared with about a third of adults overall. And the suicide rate has increased by 35 percent over the last two decades.
In addition to serving the population at large, the 988 Lifeline also aspires to provide help tailored to specific groups. The Lifeline now offers an L.G.B.T.Q. “subnetwork” for those under the age of 25 and this month rolled out Spanish text and chat options.
Dr. Dole said that later this year the Lifeline is planning to add a video phone service for the deaf and hard of hearing.
If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline or go to SpeakingOfSuicide.com/resources for a list of additional resources. Go here for resources outside the United States.

Health
Americans breathe in carcinogenic chemicals found in cars: study

Researchers have found that a source of carcinogenic chemicals is in Americans’ cars – but there may be a way to reduce your risk.
Environmental Science and Technology, a peer-reviewed scientific journal, published a study called “Flame Retardant Exposure in Vehicles Is Influenced by Use in Seat Foam and Temperature” on Tuesday.
The study explains that Americans breathe in chemicals from the flame retardants in their vehicles. The chemicals can cause issues ranging from developmental neurotoxicity to thyroid hormone dysregulation and even cancer.
The types of chemicals found in flame retardants range from polybrominated diphenyl ethers (PBDEs), which were common in cars until the early 2000s, to alternative brominated flame retardants (BFRs) and organophosphate ester flame retardants (OPEs).
STUDY FINDS EVIDENCE OF MICROPLASTICS IN BRAINS AND OTHER ORGANS
Interior detail of an electric car, taken on August 4, 2015. (Neil Godwin/T3 Magazine/Future via Getty Images)
The federal government requires a level of flame retardants in vehicles. The National Highway Traffic Safety Administration (NHTSA) mandated the use of flame retardants in the 1970s.
“Flame retardant (FR) chemicals are intentionally used in electronics, furnishings, and building materials to meet flammability standards,” the study explains.
STD RATES SKYROCKET AMONG AMERICANS 55 AND OLDER: CDC
“Most [flame retardants] are used in an additive manner (i.e., not chemically bound), and many are semivolatile, indicating that they can be present in both the gas phase and partially in the condensed phase (e.g., particles and surfaces), depending on environmental conditions.”

A motorcycle officer weaves through traffic on a Los Angeles freeway during the evening rush hour on April 12, 2023 in Los Angeles, California. (FREDERIC J. BROWN/AFP via Getty Images)
Americans who drive professionally or face long commutes may be at a higher risk of harm from the chemicals.
“These findings highlight that commuters are likely to be exposed to [flame retardants], especially those with longer commutes or those who drive vehicles full time as part of their employment,” the paper read.
“In addition, children, who breathe a greater amount of air per kg body weight compared to adults, would also be at risk of greater exposures for equivalent commuting times.”
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER

An interior view of a vehicle on April 2, 2024 in Beijing, China (VCG/VCG via Getty Images)
Drivers and passengers in warmer states may face a greater risk of breathing in the flame retardant chemicals. But rolling down car windows, turning off the AC and parking in covered garages may help reduce exposure to the dangerous chemicals, researchers say.
“Increasing ventilation by opening vehicle windows and avoiding recirculating interior cabin air may also reduce exposures,” the study said. “However, the greatest reduction in exposure from vehicle air would come from significantly reducing the amount of FRs added to personal vehicles.”
For more Health articles, visit www.foxnews.com/health.
Health
Ask a doc: 'Is it dangerous to crack my neck or back?'

Cracking your back or neck might provide quick relief and a satisfying popping noise — but is it a safe practice?
“When you stretch or manipulate your spine, such as by twisting or bending, the pressure within the joint changes,” Dr. William Kemo, a neurosurgeon at the Virginia Spine Institute, told Fox News Digital.
“This can cause a sudden release of gas bubbles, leading to a cracking sound.”
BE WELL: KEEP YOUR BONES STRONG TO PREVENT OSTEOPOROSIS
People often crack their back or neck out of habit, or to temporarily relieve tension or stiffness, Kemo noted.
“Typically, they do this to loosen up their back or neck when it is feeling tight or stiff. The ‘cracking’ is the popping of a tight or stiff facet joint.”
People often crack their back or neck out of habit to temporarily relieve tension or stiffness, a doctor noted. (iStock)
While the act of cracking can release endorphins (feel-good chemicals) for temporary relief, it doesn’t address the source of the tension, according to Tori Hartline, a chiropractor at Sunlife Chiropractic in Frisco, Texas.
ASK A DOC: ‘HOW CAN I IMPROVE MY POSTURE?’
Popping or cracking can even lead to injury, she warned.
“Chiropractors are trained to look for restricted areas in the spine and perform specific adjustments to decrease tension and improve range of motion,” Hartline said.

Cracking your back or neck can cause a myriad of health issues, experts are warning. (iStock)
“When an individual tries to pop their own back or neck, the segments that release gas are hypermobile segments versus the area of restriction. The joints above and below the area of restriction will move too much to compensate.”
She added, “Therefore, these cracks do not address the problem and can instead lead to further injury.”
The impacts of cracking your back or neck can include joint hypermobility, sprains or strains due to taking the joint too far past its proper range of motion — and even a fracture if too much pressure is applied, Hartline noted.
FOR ACUTE LOWER BACK PAIN, THESE ARE THE BEST MEDICATIONS, NEW STUDY FINDS
Kemo agreed, warning that cracking your back can cause unnecessary wear and tear on your spine.
“It may lead to strain on the muscles and ligaments surrounding the spine, potentially causing injury or exacerbating existing issues,” he added.

One expert suggested seeing a licensed chiropractor to identify areas of restriction and prescribe therapeutic exercise and stretches. (iStock)
It’s especially dangerous to crack the neck, which could impede blood flow and, in very rare cases, could increase stroke risk, according to Dr. Todd Sinett, a chiropractor at Tru Whole Care in New York.
Alternatives to cracking
There are plenty of safe alternatives that will provide longer-term relief without exacerbating potential issues with the spine, Kemo said.
“Commit to a daily stretching routine, and engage in core muscle exercises to strengthen the muscles supporting the spine,” he recommended.
WHAT IS SCOLIOSIS? CAUSES AND SYMPTOMS OF THE SPINAL CONDITION, TREATMENT PLANS AND MORE
Regular physical activity can also be helpful.
“A body in motion stays in motion, and helps avoid stiffness and alleviates tension,” Kemo said.
The doctor also suggested optimizing your ergonomics at home, at work and in the car.

Committing to a daily stretching routine and engaging in core muscle exercises can help strengthen the muscles supporting the spine, one doctor said. (iStock)
“Examine your daily routines to see if there may be repetitive situations that leave you feeling stiff or experiencing tension/tightness,” Kemo suggested.
This might include hunching in your chair or seat in the car, holding your device and looking down for prolonged periods, or sleeping in a certain position.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Hartline also suggested seeing a licensed chiropractor, who can identify the areas of restriction and prescribe therapeutic exercise and stretches to give you the best results.
“If you’re experiencing persistent discomfort or pain, it’s best to consult with a medical specialist for proper evaluation and treatment.”
Overall, both experts agree that it’s important to listen to your body and avoid forceful manipulation of the spine.
“If you’re experiencing persistent discomfort or pain, it’s best to consult with a medical specialist for proper evaluation and treatment,” Kemo said.
“Remember, what works for one person may not be suitable for another — so personalized guidance is key.”
For more Health articles, visit www.foxnews.com/health.
Health
Seniors and breast cancer: Why aren’t older women told to get mammograms?

A major public health agency last week expanded its breast cancer screening guidelines to include younger women — but some people are concerned that one key age group has been excluded.
The U.S. Preventive Services Task Force (USPSTF) announced on April 30 that women between ages 40 and 74 should get mammograms every other year.
This is a significant change from previous guidelines, which said women should begin biennial mammograms at age 50, but could opt to begin as young as 40.
BREAST CANCER MAMMOGRAM SCREENINGS SHOULD START AT AGE 40 INSTEAD OF 50, SAYS HEALTH TASK FORCE
Some experts object to the fact that the agency doesn’t include official screening recommendations for women older than 74.
“The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of screening mammography in women 75 years or older,” the agency stated in the guidance.
The U.S. Preventive Services Task Force (USPSTF) announced on April 30 that women between the ages of 40 and 74 should get mammograms every other year. (iStock)
Dr. Denise Pate, medical director with Medical Offices of Manhattan and contributor to LabFinder, voiced her disagreement with the lack of mammogram recommendations for older women.
“I think it is an antiquated view that sells short the potential of women older than 75,” she told Fox News Digital.
SOME BREAST CANCER PATIENTS COULD BE AT RISK OF ANOTHER TYPE OF CANCER, STUDY REVEALS
“The recommendations consider that the older population may be over-diagnosed, potentially with slow-growing breast cancers — but this does not take into account the increase in life expectancy for American women.”
A woman who is 75 right now has a life expectancy of 87, according to the U.S. Centers for Disease Control and Prevention (CDC).
Lack of research
One of the main reasons that women over 74 were excluded is that the age group was not included in clinical trials.
“When the major randomized controlled trials were performed in the 1970s and 1980s to show how effective mammograms are, they didn’t include enough women in those age groups to confirm their necessity,” Dr. Jacqueline Holt, medical director of women’s imaging for national radiology provider RadNet in Wilmington, Delaware, told Fox News Digital.

One of the main reasons that women over age 74 were excluded is that the age group was not included in clinical trials. (iStock)
“Cancer risk doesn’t drop off at 74 — the risk increases,” she said.
“It’s misinformation that cancers grow slower in this age group and that women will die of something else first.”
Risks vs. benefits
The primary risk noted for screening older women is the potential for false positives.
“The potential harms of breast cancer screening in older women include false positive results and overdiagnosis,” said one study published in the Journal of the American Board of Family Medicine.
“Cancer risk doesn’t drop off at 74 — the risk increases.”
Among women 75 years and older, 200 out of 1,000 who are screened over a 10-year period will experience a “false alarm,” the researchers noted, “which can cause pain, anxiety and distress.”
Pate acknowledged that this risk does exist.
“Of course, with continued screening, there is the continued risk of finding breast cancer in an earlier stage or finding a suspicious image that prompts recommendations for biopsy, proving to be a false positive — and this can cause a lot of anxiety,” she said.

The risks of not screening are “leaving these women in the dark about their status,” a doctor said. (iStock)
The risks of not screening, however, are “leaving these women in the dark about their status,” the doctor said.
“As I always explain to my patients, knowledge is power,” Pate told Fox News Digital.
“I would rather choose anxiety about a biopsy that may or may not prove breast cancer versus anxiety of surgery, radiation and chemotherapy for a cancer that is found too late due to lack of screening.”
AN OVERVIEW OF BREAST CANCER, SYMPTOMS TO LOOK OUT FOR, WHEN TO START THINKING ABOUT ROUTINE SCREENINGS
Holt agrees the benefits outweigh the risks.
“The primary risk that the USTF focuses on is anxiety due to false positives or callbacks that don’t lead to a diagnosis of cancer,” she told Fox News Digital.
“The death rate has decreased by at least 40% since 1995, thanks to mammographic screenings finding the cancer earlier and better treatment.”

“The death rate has decreased by at least 40% since 1995, thanks to mammographic screenings finding the cancer earlier and better treatment,” a doctor said. (iStock)
Women do have the option to continue screening beyond the age of 74 if they choose, the doctors noted — and this should be covered by their insurance plan.
“There is no cut-off for age,” Holt noted. “Medicare will still cover the cost of a mammogram.”
The American College of Obstetricians and Gynecologists (ACOG), the American Cancer Society (ACS) and the National Comprehensive Cancer Network (NCCN) all recommend mammograms starting at age 40.
“Age alone should not be the basis to continue or discontinue screening.”
“Each of these three groups bases its stop age on a woman’s life expectancy and not simply on their age,” Pate noted.
The ACS has stated that women should continue receiving mammograms as long as they are in overall good health and expect to live for another 10 years or more.
More than one-quarter of cases of breast cancer are diagnosed in women 75 years and older, according to ACOG.
MISSING MAMMOGRAMS: OVER 20% OF WOMEN DON’T FOLLOW BREAST CANCER SCREENING GUIDELINES, STUDY SAYS
“Age alone should not be the basis to continue or discontinue screening,” according to a statement from ACOG.
“Beyond age 75 years, the decision to discontinue screening mammography should be based on a shared decision-making process informed by the woman’s health status and longevity.”

More than one-quarter of cases of breast cancer are diagnosed in women 75 years and older, according to the American College of Obstetricians and Gynecologists. (iStock)
Dr. Wanda Nicholson, chair of the USPSTF, sent a statement to Fox News Digital about the decision to omit women over age 74 in the recommendations.
“Women deserve to know what the science says about how they can best stay healthy as they age,” she said.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“We looked carefully at all the available evidence about whether women who are 75 and older should be screened for breast cancer, but unfortunately, the available research was limited.”

“Women deserve to know what the science says about how they can best stay healthy as they age,” a doctor said. (iStock)
“None of the studies of breast cancer screening included women in this age group, so we are urgently calling for more evidence on this important population.”
She added, “In the meantime, we encourage women who are 75 and older to talk with a trusted health care professional about what preventive care is right for them, given their specific health circumstances.”
Fox News Digital reached out to the ACOG and the ACS requesting additional comment.
For more Health articles, visit www.foxnews.com/health.
-

 World1 week ago
World1 week agoRussian forces gained partial control of Donetsk's Ocheretyne town
-
Movie Reviews1 week ago
Challengers Movie Review
-

 Politics1 week ago
Politics1 week agoDems disagree on whether party has antisemitism problem
-

 Politics1 week ago
Politics1 week agoHouse Republicans brace for spring legislative sprint with one less GOP vote
-

 World1 week ago
World1 week agoAt least four dead in US after dozens of tornadoes rip through Oklahoma
-
 Politics1 week ago
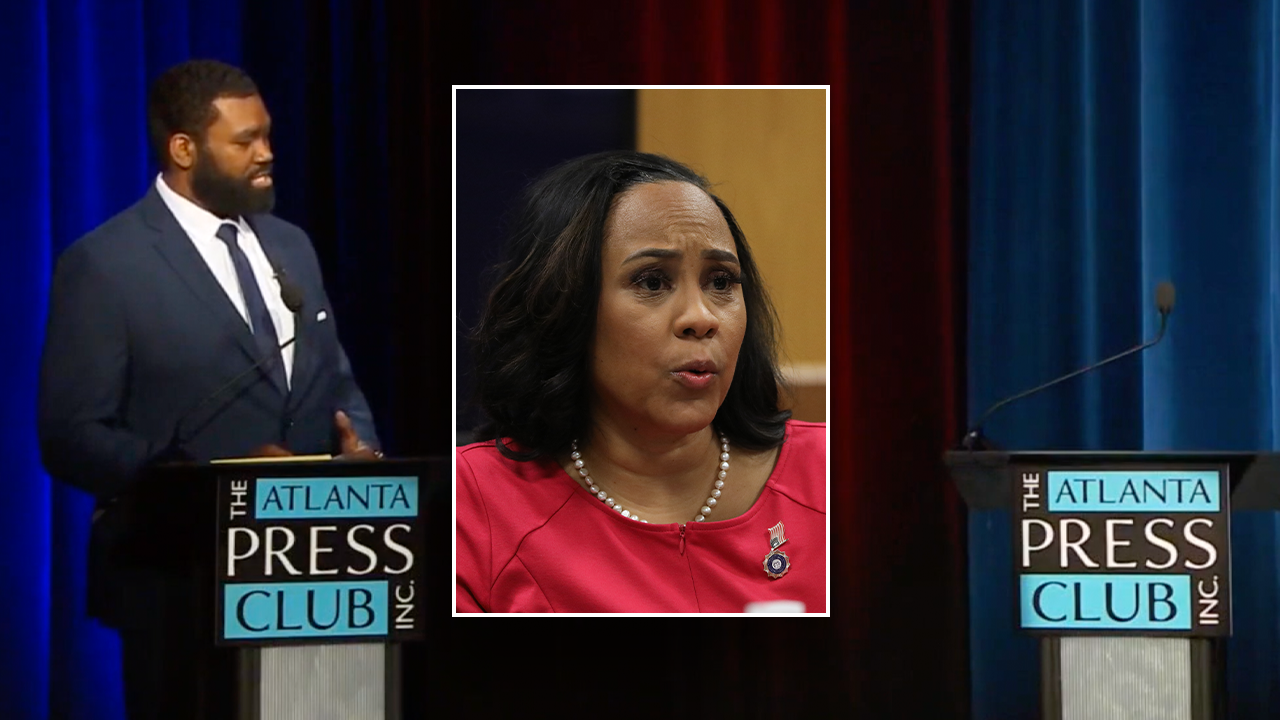
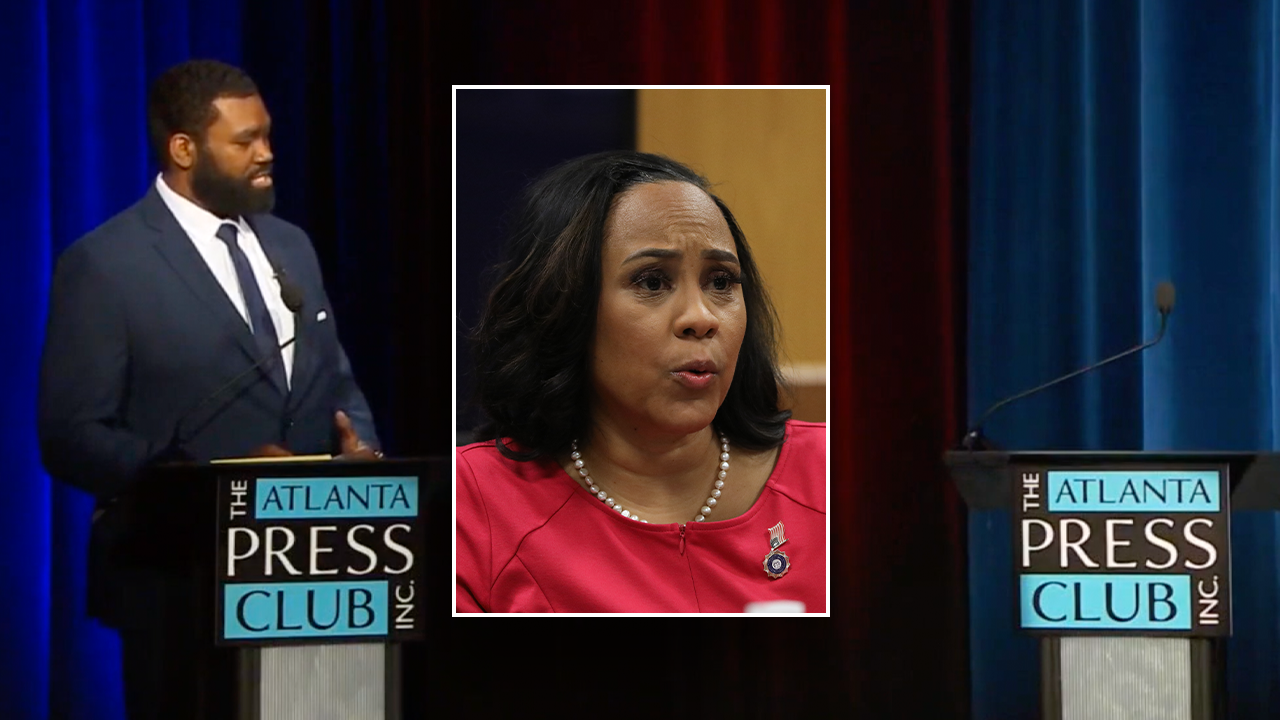
Politics1 week agoAnti-Trump DA's no-show at debate leaves challenger facing off against empty podium
-
 Politics1 week ago
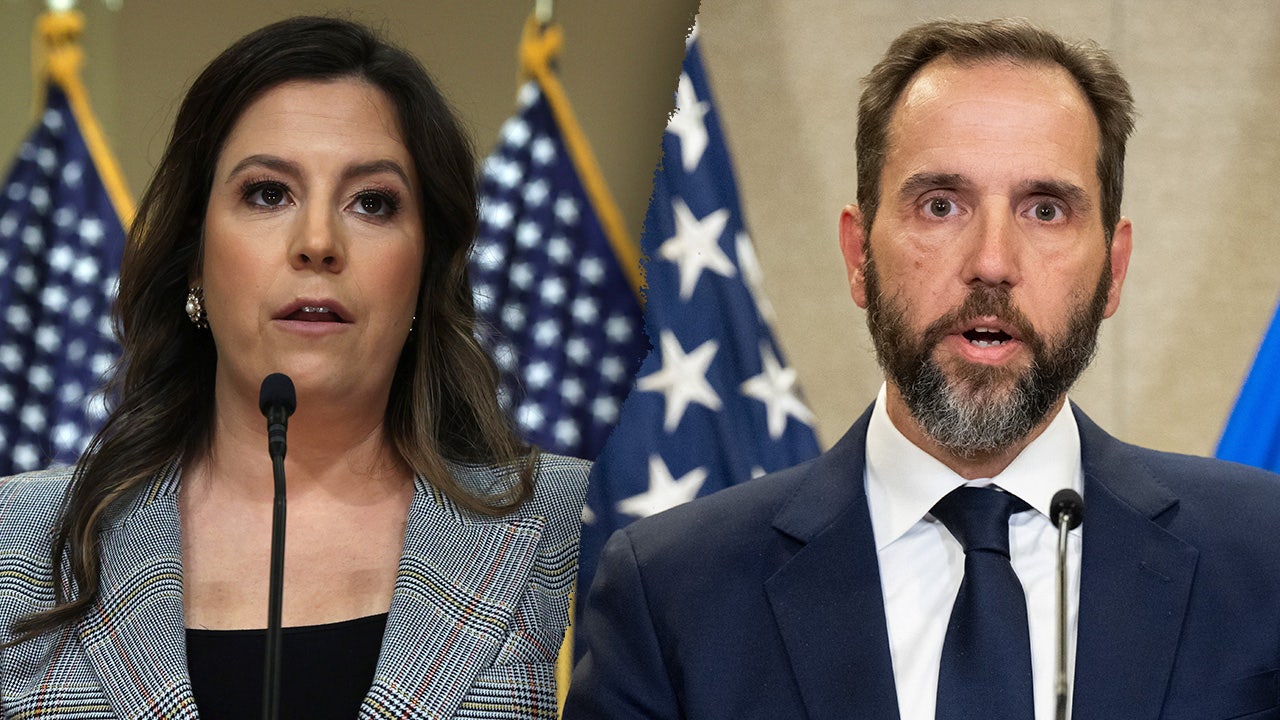
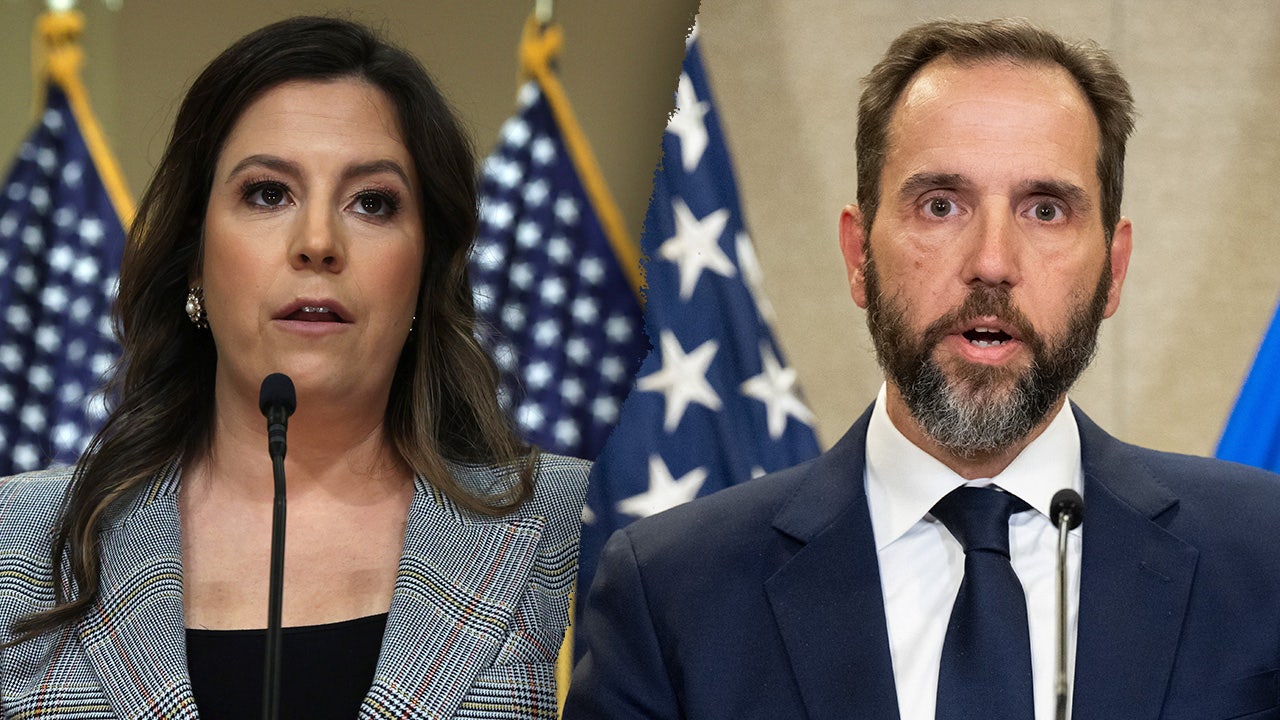
Politics1 week agoStefanik hits special counsel Jack Smith with ethics complaint, accuses him of election meddling
-

 News1 week ago
News1 week agoAs student protesters get arrested, they risk being banned from campus too