Science
Tuberculosis cases rising in California, and state officials are sounding the alarm

Tuberculosis cases are rising again in California, and health officials are urging those at higher risk, as well as doctors, to be alert for the disease, which can lurk in people’s bodies for years before becoming potentially deadly.
The number of tuberculosis cases in 2023 rose by 15% in California compared with the previous year, the state Department of Public Health said. That’s the highest year-over-year increase since 1989, when it was tied to people co-infected with HIV.
There were 2,113 cases across California last year; that’s about the same amount reported in 2019, before the COVID-19 pandemic. Seniors 65 and older had the highest percentage increase in cases from 2022 to 2023.
Tuberculosis rates also are rising nationally, up 16% in 2023 compared with the previous year, the U.S. Centers for Disease Control and Prevention said Thursday. The 9,615 cases provisionally reported last year were the highest since 2013 and were 8% higher than the tally of 8,895 cases reported in 2019.
Those at major risk for tuberculosis include people who have lived outside the U.S. where the TB rate is high, including most nations in Asia, the Middle East, Africa, Eastern Europe and Latin America.
Nationally in 2023, TB cases increased among all age groups and those born inside or outside the U.S., the CDC said.
Caused by bacteria Mycobacterium tuberculosis, tuberculosis disease is spread through the air. Unlike COVID-19 — in which infection can occur in minutes — a person would typically need to be exposed for hours to inhale enough TB bacteria to get infected, said Dr. Julie Higashi, director of the L.A. County tuberculosis control program.
Most active cases in California are from people with latent TB who picked up the bacteria decades ago but weren’t contagious or showing symptoms. “Then something happens. Either they age … and their immune system actually becomes weaker … and then they progress” to acute TB, Higashi said.
On the flip side, an estimated 18% of TB cases in L.A. County occur from recent transmission.
California officials said that 13% of people with tuberculosis died in 2020. That’s up from 8% in 2010. Generally, more than 200 Californians die from tuberculosis every year, state officials say.
TB has afflicted humanity since before the dawn of recorded history, and at one point in the 17th and 18th centuries, caused one-quarter of all deaths in Europe.
It was only on March 24, 1882 — 142 years ago Sunday — that a scientist announced the discovery of the bacteria that causes TB. (Decades earlier, TB was thought to be hereditary, and in New England, inspired “vampire panics” because people thought the first family member to die of TB would come back as a vampire to infect the rest of them, according to the CDC.)
By the start of the 20th century, tuberculosis was one of the leading causes of death in the United States.
Governments in the early part of the last century began making serious progress in preventing infectious diseases. According to the CDC, housing improvements reduced overcrowding — a risk factor for TB spread — and programs were launched to control TB. By 1940, the TB death rate was one-fourth what it had been at the turn of the century. Further progress was made with the discovery of TB treatments in the middle of the 20th century.
TB cases have generally been declining in California since the early 1990s but continue to take a significant toll, a tragedy given the disease is detectable and treatable.
“Not only can you treat the active disease, you can also treat the latent disease, which is much easier to treat — fewer drugs, much shorter time — and then prevent that progression to the active form of disease,” Higashi said.
The CDC estimates 13 million people in the U.S. have a latent tuberculosis infection — meaning they have no symptoms and can’t spread the bacteria. Without treatment, 5% to 10% will develop active disease that can turn contagious and potentially deadly later in life.
Outbreaks can happen locally. In Contra Costa County last year, 11 confirmed cases were linked to staff and customers of the California Grand Casino in Pacheco. At least 10 cases were genetically linked.
According to the most recent data, California counties with the highest per capita rates of tuberculosis are generally along populous coastal areas. In Southern California, those with the highest rates were Los Angeles, San Diego, Orange and Imperial counties. In Northern California, they were Santa Clara, Alameda, Sacramento, Contra Costa, San Francisco, San Mateo, San Joaquin, Solano, Monterey and Napa counties.
Officials noticed a substantial drop in TB cases in 2020, tied to stay-at-home orders and reduced travel during the early phase of the pandemic. Since then, case rates have increased 4% to 5% each year before jumping by 15% in 2023.
The rise in TB cases in Orange County, California’s third most populous, has been especially pronounced, jumping 20% between 2022 and 2023; in L.A. County, cases rose by about 4% over the same time, according to local data.
According to state data, Orange County’s per capita TB case rate is 10% higher than L.A. County’s.
“We have a lot of people who travel, and also have family members who come from other countries with higher rates of TB,” Dr. Regina Chinsio-Kwong, Orange County’s health officer, said.
Cities in Orange County with TB case rates higher than the overall county rate are Laguna Hills, Westminster, Garden Grove, Buena Park, Santa Ana, Fountain Valley, Anaheim, Costa Mesa and Lake Forest, according to county data.
Those at highest risk in Orange County are people born outside the U.S., Asian Americans, males, and seniors age 65 and up. Having diabetes, HIV or smoking cigarettes increases the risk of having latent TB develop into full-blown TB, Chinsio-Kwong said.
With “latent TB, when someone’s immune system is nice and strong, you have no symptoms, it doesn’t affect your organs,” Chinsio-Kwong said. “But it can develop into active TB when you’re immunosuppressed. So that’s where diabetes, smoking or any infectious disease, like HIV, can really put you at higher risk of developing an active TB case.”
Routine testing for higher-risk people, such as healthcare workers, can be helpful. Chinsio-Kwong said she was diagnosed with a case of latent TB earlier in her career, prompting her to take a nine-month regimen of treatment.
“If we can appropriately treat all the latent TB cases, we can really reduce the number of active TB cases,” she said. “The hope is that you detect latent TB before you develop symptoms — because by the time you have symptoms, you’re an active TB case, spreading your germs and possibly even spreading the infection to others.”
In Los Angeles County, 91% of tuberculosis cases were among Latino or Asian American residents. The top seven countries of birth of people with TB were Mexico, the Philippines, Guatemala, China, Vietnam, El Salvador and South Korea.
Areas with the highest tuberculosis case rates in regions monitored by the L.A. County Department of Public Health were in central L.A., which the agency defines as including downtown, Echo Park, Silver Lake and the Hollywood Hills; South L.A.; and an area of the western San Gabriel Valley that includes Alhambra, Monterey Park and San Gabriel.
Other areas with TB rates above the L.A. County average include the neighborhoods covering Hollywood, northeast L.A., El Monte, East L.A., Inglewood, Torrance and Bellflower.
Of the regions with L.A. County’s highest TB cases, those with the highest mortality rates were in the Alhambra-Monterey Park-San Gabriel area, where 15.4% of tuberculosis cases resulted in death; and Central L.A., where 20.5% of cases resulted in death.
A large problem with TB is that it’s possible for doctors to miss a diagnosis, as TB is relatively rare. The California Department of Public Health last month urged healthcare providers to consider tuberculosis as a potential cause of respiratory illness among higher-risk people.
There are situations in which doctors can misdiagnose people with TB. While the disease typically grows in the lungs — leading to symptoms such as chronic cough, chest pain and coughing up blood — the bacteria also can grow in other areas of the body, including the gastrointestinal tract or the nervous system, and doctors might miss a TB diagnosis in that atypical presentation.
Instances of misdiagnosed TB cases previously documented by The Times include a San Fernando Valley businessman, who was raised in Chile and suffered for 11 years until a TB diagnosis was made; and a Shanghai-born UC Berkeley Mandarin lecturer who was misdiagnosed with Crohn’s disease and given a steroid to suppress her immune system, allowing her TB to spread. It was only when she lay gravely ill in a hospital that a doctor seriously considered TB.
One prominent misdiagnosis occurred in 2004, when Dr. Claudia Lacson — pregnant with her first child — fell into a coma in Georgia after complaining of severe headaches and a persistent fever. Doctors initially suspected bacterial meningitis, but by the time doctors began TB treatment, it was too late, and she died at age 38, weeks after giving birth to a daughter, who also did not survive.
“What we want providers to know is that when any individual comes to them presenting with respiratory symptoms, they need to start thinking about is: Is this potentially a person who is at risk of having TB?” Chinsio-Kwong said. “Even if you weren’t born [in] another country, if you’re in close proximity to those who are coming from out of the United States, there’s a risk.”

Science
Diablo Canyon clears last California permit hurdle to keep running

Central Coast Water authorities approved waste discharge permits for Diablo Canyon nuclear plant Thursday, making it nearly certain it will remain running through 2030, and potentially through 2045.
The Pacific Gas & Electric-owned plant was originally supposed to shut down in 2025, but lawmakers extended that deadline by five years in 2022, fearing power shortages if a plant that provides about 9 percent the state’s electricity were to shut off.
In December, Diablo Canyon received a key permit from the California Coastal Commission through an agreement that involved PG&E giving up about 12,000 acres of nearby land for conservation in exchange for the loss of marine life caused by the plant’s operations.
Today’s 6-0 vote by the Central Coast Regional Water Board approved PG&E’s plans to limit discharges of pollutants into the water and continue to run its “once-through cooling system.” The cooling technology flushes ocean water through the plant to absorb heat and discharges it, killing what the Coastal Commission estimated to be two billion fish each year.
The board also granted the plant a certification under the Clean Water Act, the last state regulatory hurdle the facility needed to clear before the federal Nuclear Regulatory Commission (NRC) is allowed to renew its permit through 2045.
The new regional water board permit made several changes since the last one was issued in 1990. One was a first-time limit on the chemical tributyltin-10, a toxic, internationally-banned compound added to paint to prevent organisms from growing on ship hulls.
Additional changes stemmed from a 2025 Supreme Court ruling that said if pollutant permits like this one impose specific water quality requirements, they must also specify how to meet them.
The plant’s biggest water quality impact is the heated water it discharges into the ocean, and that part of the permit remains unchanged. Radioactive waste from the plant is regulated not by the state but by the NRC.
California state law only allows the plant to remain open to 2030, but some lawmakers and regulators have already expressed interest in another extension given growing electricity demand and the plant’s role in providing carbon-free power to the grid.
Some board members raised concerns about granting a certification that would allow the NRC to reauthorize the plant’s permits through 2045.
“There’s every reason to think the California entities responsible for making the decision about continuing operation, namely the California [Independent System Operator] and the Energy Commission, all of them are sort of leaning toward continuing to operate this facility,” said boardmember Dominic Roques. “I’d like us to be consistent with state law at least, and imply that we are consistent with ending operation at five years.”
Other board members noted that regulators could revisit the permits in five years or sooner if state and federal laws changes, and the board ultimately approved the permit.
Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
Science
When slowing down can save a life: Training L.A. law enforcement to understand autism
Kate Movius moved among a roomful of Los Angeles County sheriff’s deputies, passing out a pop trivia quiz and paper prism glasses.
She told them to put on the vision-distorting glasses, and to write with their nondominant hand. As they filled out the tests, Movius moved about the City of Industry classroom pounding abruptly on tables. Then came the cowbell. An aide flashed the overhead lights on and off at random. The goal was to help the deputies understand the feeling of sensory overwhelm, which many autistic people experience when incoming stimulation exceeds their capacity to process.
“So what can you do to assist somebody, or de-escalate somebody, or get information from someone who suffers from a sensory disorder?” Movius asked the rattled crowd afterward. “We can minimize sensory input. … That might be the difference between them being able to stay calm and them taking off.”
Movius, founder of the consultancy Autism Interaction Solutions, is one of a growing number of people around the U.S. working to teach law enforcement agencies to recognize autistic behaviors and ensure that encounters between neurodevelopmentally disabled people and law enforcement end safely.
She and City of Industry Mayor Cory Moss later passed out bags filled with tools donated by the city to aid interactions: a pair of noise-damping headphones to decrease auditory input, a whiteboard, a set of communication cards with words and images to point to, fidget toys to calm and distract.
“The thing about autistic behavior when it comes to law enforcement is a lot of it may look suspicious, and a lot of it may feel very disrespectful,” said Movius, who is also the parent of an autistic 25-year-old man. Responding officers, she said, “are not coming in thinking, ‘Could this be a developmentally disabled person?’ I would love for them to have that in the back of their minds.”
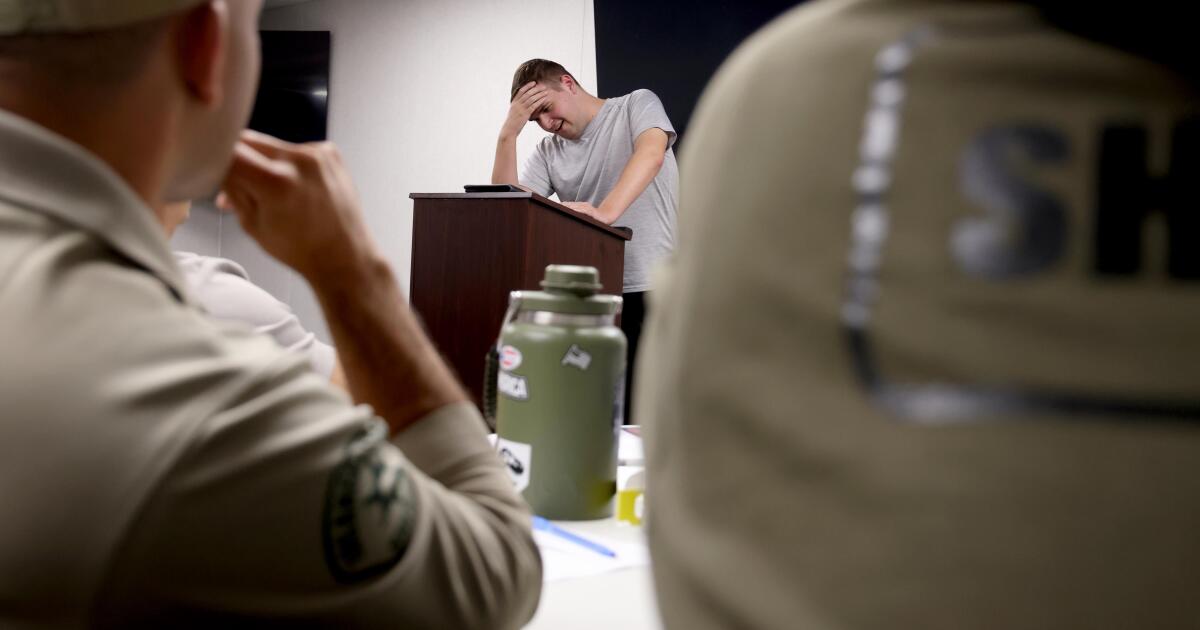
A sheriff’s deputy reads a pamphlet on autism during the training program.
(Genaro Molina / Los Angeles Times)
Autism spectrum disorder is a developmental condition that manifests differently in nearly every person who has it. Symptoms cluster around difficulties in communication, social interaction and sensory processing.
An autistic person stopped by police might hold the officer’s gaze intensely or not look at them at all. They may repeat a phrase from a movie, repeat the officer’s question or temporarily lose their ability to speak. They might flee.
All are common involuntary responses for an autistic person in a stressful situation, which a sudden encounter with law enforcement almost invariably is. To someone unfamiliar with the condition, all could be mistaken for intoxication, defiance or guilt.
Autism rates in the U.S. have increased nearly fivefold since the Centers for Disease Control began tracking diagnoses in 2000, a rise experts attribute to broadening diagnostic criteria and better efforts to identify children who have the condition.
The CDC now estimates that 1 in 31 U.S. 8-year-olds is autistic. In California, the rate is closer to 1 in 22 children.
As diverse as the autistic population is, people across the spectrum are more likely to be stopped by law enforcement than neurotypical peers.
About 15% of all people in the U.S. ages 18 to 24 have been stopped by police at some point in their lives, according to federal data. While the government doesn’t track encounters for disabled people specifically, a separate study found that 20% of autistic people ages 21 to 25 have been stopped, often after a report or officer observation of a person behaving unusually.
Some of these encounters have ended in tragedy.
In 2021, Los Angeles County sheriff’s deputies shot and permanently paralyzed a deaf autistic man after family members called 911 for help getting him to a hospital.
Isaias Cervantes, 25, had become distressed about a shopping trip and started pushing his mother, his family’s attorney said at the time. He resisted as two deputies attempted to handcuff him and one of the deputies shot him, according to a county report.
In 2024, Ryan Gainer’s family called 911 for support when the 15-year-old became agitated. Responding San Bernardino County sheriff‘s deputies shot and killed him outside his Apple Valley home.
Last year, police in Pocatello, Idaho, shot Victor Perez, 17, through a chain-link fence after the nonspeaking teenager did not heed their shouted commands. He died from his injuries in April.

Sheriff’s deputies take a trivia quiz using their non-writing hands, while wearing vision-distorting glasses, as Kate Movius, standing left, and Industry Mayor Cory Moss, right, ring cowbells. The idea was to help them understand the sensory overwhelm some autistic people experience.
(Genaro Molina / Los Angeles Times)
As early as 2001, the FBI published a bulletin on police officers’ need to adjust their approach when interacting with autistic people.
“Officers should not interpret an autistic individual’s failure to respond to orders or questions as a lack of cooperation or as a reason for increased force,” the bulletin stated. “They also need to recognize that individuals with autism often confess to crimes that they did not commit or may respond to the last choice in a sequence presented in a question.”
But a review of multiple studies last year by Chapman University researchers found that while up to 60% of officers have been on a call involving an autistic person, only 5% to 40% had received any training on autism.
In response, universities, nonprofits and private consultants across the U.S. have developed curricula for law enforcement on how to recognize autistic behaviors and adapt accordingly.
The primary goal, Movius told deputies at November’s training session, is to slow interactions down to the greatest extent possible. Many autistic people require additional time to process auditory input and verbal responses, particularly in unfamiliar circumstances.
If at all possible, Movius said, wait 20 seconds for a response after asking a question. It may feel unnaturally long, she acknowledged. But every additional question or instruction fired in that time — what’s your name? Did you hear me? Look at me. What’s your name? — just decreases the likelihood that a person struggling to process will be able to respond at all.
Moss’ son, Brayden, then 17, was one of several teenagers and young adults with autism who spoke or wrote statements to be read to the deputies. The diversity of their speech patterns and physical mannerisms showed the breadth of the spectrum. Some were fluently verbal, while others communicated through signs and notes.
“This population is so diverse. It is so complicated. But if there’s anything that we can show [deputies] in here that will make them stop and think, ‘Hey, what if this is autism?’ … it is saving lives,” Moss said.

Mayor Cory Moss, left, and Kate Movius hug at the end of the training program last November. Movius started Autism Interaction Solutions after her son was born with profound autism.
(Genaro Molina / Los Angeles Times)
Some disability advocates cautioned that it takes more than isolated training sessions to ensure encounters end safely.
Judy Mark, co-founder and president of the nonprofit Disability Voices United, says she trained thousands of officers on safe autism interactions but stopped after Cervantes’ shooting. She now urges families concerned about an autistic child’s safety to call an ambulance rather than law enforcement.
“I have significant concern about these training sessions,” Mark said. “People get comfort from it, and the Sheriff’s Department can check the box.”
While not a panacea, supporters argue that a brief course is better than no preparation at all. Some years ago, Movius received a letter from a man whose profoundly autistic son slipped away as the family loaded their car at the beach. He opened the unlocked door of a police vehicle, climbed into the back and began to flail in distress.
Though surprised, the officer seated at the wheel de-escalated the situation and helped the young man find his family, the father wrote to Movius. He had just been to her training.
-

 World2 days ago
World2 days agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts3 days ago
Massachusetts3 days agoMother and daughter injured in Taunton house explosion
-

 Montana1 week ago
Montana1 week ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Louisiana5 days ago
Louisiana5 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Denver, CO2 days ago
Denver, CO2 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Technology7 days ago
Technology7 days agoYouTube TV billing scam emails are hitting inboxes
-

 Technology7 days ago
Technology7 days agoStellantis is in a crisis of its own making
-

 Politics7 days ago
Politics7 days agoOpenAI didn’t contact police despite employees flagging mass shooter’s concerning chatbot interactions: REPORT


















