Science
How the body’s immune system tries to fight off COVID-19
Vaccines have proven themselves to be one of the best protection towards a critical case of COVID-19: Based on the Facilities for Illness Management and Prevention, unvaccinated adults had been about 13 instances extra more likely to be hospitalized with the illness than vaccinated adults as of late November.
However vaccines and the antibodies they generate are only one piece of the puzzle with regards to preventing off the coronavirus. The immune system has different units of defenders that discover and kill contaminated cells, then protect a residing file of the virus, micro organism or different infectious agent so the physique can reply sooner the subsequent time it’s underneath assault.
And velocity is important, stated E. John Wherry, director of the College of Pennsylvania’s Institute for Immunology.
“Throughout an an infection, it’s a race,” with the immune system urgent to cease the virus earlier than it has multiplied to a debilitating stage, Wherry defined. That’s notably true for the Omicron variant, which replicates at an alarming charge.
Right here‘s a breakdown of how the physique’s immune system works and the way it’s been examined by Omicron:
B cells, T cells, NKs and DCs
Consider the immune system as having three layers of protection. One tries to maintain hostile molecules — pathogens — on the surface, trying in. That job is carried out by the pores and skin, the physique’s largest organ, whose cells can defeat invaders and warn the remainder of the immune system that hassle is at hand.
The second layer tries to cease the attackers as soon as they’ve entered the physique, however earlier than they’ve contaminated cells. That is the place the bone marrow is available in. It produces “pure killer” or NK cells in addition to B cells, those that generate antibodies. Each are kinds of white blood cells, or lymphocytes.
We’ve got “pure killer” or NK cells within the tonsils, lymph nodes and spleen, able to struggle any attackers.
(Nationwide Institute of Allergy and Infectious Ailments)
NKs earned their title as a result of they aren’t produced in response to an attacker; they’re already current and able to kill cells that don’t belong within the physique, similar to tumor cells. NKs are a part of what scientists name the innate immune system. Based on researchers at Rockefeller College, NKs hand around in the tonsils, lymph nodes and spleen, then rush to confront attackers the place they emerge.
Antibodies, alternatively, are generated after an attacker is found, making them a part of what’s generally known as the adaptive immune system. They connect themselves to particular pathogens, which then get devoured up and destroyed by different members of the immune system‘s crew.
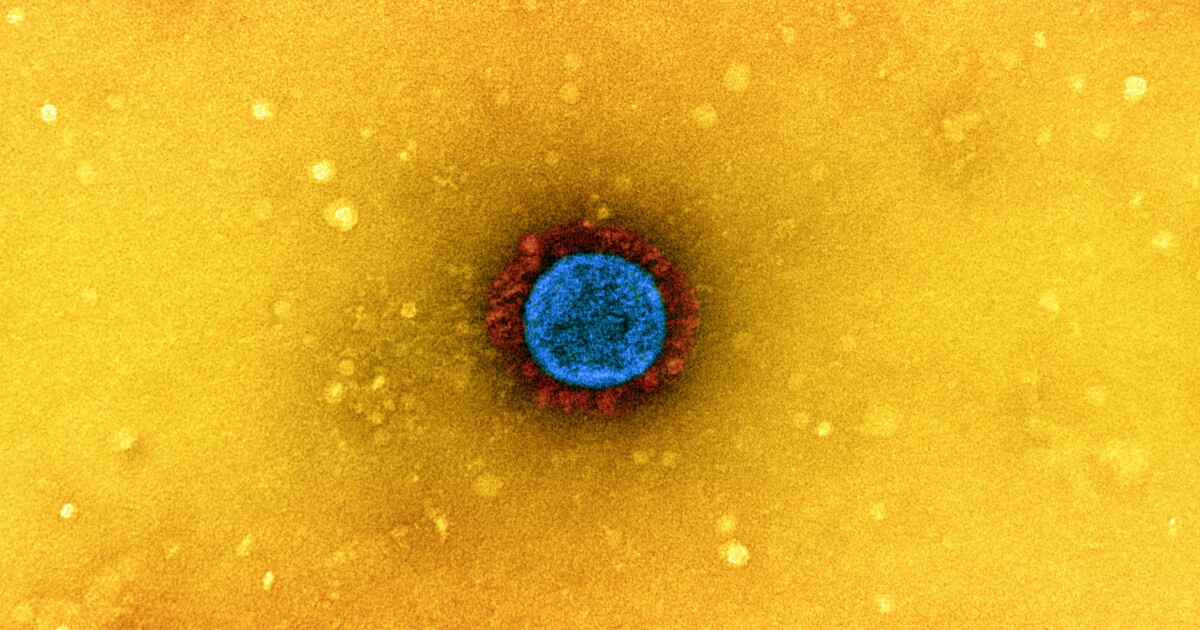
Within the case of SARS-CoV-2, the coronavirus that causes COVID-19, completely different antibodies bind to completely different components of the virus, together with the spike protein the virus makes use of to enter a wholesome cell and replicate itself again and again. If the spike protein is gummed up by an antibody, the virus can’t infect a cell.
It’s conceivable that when you’re freshly vaccinated or boosted, you could possibly have so many antibodies able to assault that you simply gained’t turn out to be contaminated, stated Trudy U. Rey, a virologist and science communicator. That is known as “sterilizing immunity,” though within the case of COVID-19, it will be merely non permanent. However that’s not the purpose of a COVID-19 vaccination. (Extra on that later.)
A extra frequent state of affairs is that some amount of invading coronaviruses get previous the antibodies. Cells have some innate defenses that may defeat the invaders, however SARS-CoV-2 has proven itself able to evading them. Fortunately, there’s a third line of protection: T cells.
T cells within the higher chest’s thymus gland can detect pathogens after they’ve gotten inside a cell, the place antibodies can’t discover them.
(Nationwide Institute of Allergy and Infectious Ailments)
Like B cells and NKs, T cells are white blood cells that originate within the bone marrow, however they develop in and emanate from the thymus gland within the higher chest. Their particular energy is their capacity to detect viruses and different germs after they’ve gotten inside a cell, the place they’re hidden from antibodies.
T cells are available in two primary flavors: killers and messengers. The deadly model detects cells which were contaminated with a virus, then kills them (by releasing a poisonous model of a granule known as a cytokine) to cease the virus from replicating. Wherry known as this “destroying the village to avoid wasting the nation.” The messengers alert B cells to the brand new risk, and so they reply by making antibodies designed to satisfy that risk.
It’s a posh molecular dance with many different very important components, together with dendritic cells or DCs, which act as sentinels and couriers throughout the immune system. Amongst different issues, the DCs inform the T cells which particular risk to seek out and kill.
As soon as an an infection is overcome, the immune system naturally winds down and sheds some antibodies and T cells. However some T cells dwell on as reminiscence T cells, prepared to reply by killing contaminated cells and stimulating the manufacturing of latest antibodies if the identical attacker returns. And a few B cells stay as reminiscence cells to deal with antibody manufacturing.
How vaccines prime the pump
Daniela Weiskopf, an immunologist on the La Jolla Institute for Immunology, stated the physique’s adaptive immune system could be very particular. That’s good, she stated, as a result of “in any other case you’d be in a relentless state of irritation.” However it additionally signifies that antibodies and T cells are restricted in what they will bind to or acknowledge. They should be taught their enemy earlier than they will defend towards it.
Vaccines assist us create antibodies and reminiscence T cells that acknowledge a virus and contaminated cells so our immune techniques react extra rapidly. Booster photographs reinforce this course of.
(Gary Coronado / Los Angeles Instances)
Vaccination, Weiskopf stated, “is nothing however coaching the immune system with out getting sick.” COVID-19 vaccines create antibodies that acknowledge the spike protein and different traits of SARS-CoV-2, together with reminiscence T cells that may acknowledge cells which were contaminated with the virus.
The extra typically your immune system sees a risk, Weiskopf stated, “the extra detailed it makes the response.” The faster, too — as soon as your system has these reminiscence cells, she stated, it could possibly react “a lot, a lot, a lot sooner” the subsequent time the identical pathogen comes knocking. Therefore the worth of booster photographs.
As viruses mutate, the components that antibodies connect themselves to might change. If they modify an excessive amount of, the antibodies gained’t be pretty much as good at binding to them and stopping them from coming into cells. That seems to be the case with the Omicron variant, which has a number of mutations that have an effect on its spike protein.
However Omicron’s mutations haven’t tempered the response of reminiscence T cells, Weiskopf, Rey and Wherry stated. That’s as a result of the mutations haven’t had a lot impact on the components of the virus that T cells acknowledge.
Past that, Weiskopf stated, every individual has a number of completely different T cells, and their T cells are completely different from everybody else’s. If by some uncommon misfortune a brand new variant managed to dodge your whole reminiscence T cells, she stated, it will nonetheless encounter loads of efficient T cells in the remainder of the inhabitants.
Rey added that a lot of the discuss “waning immunity” is predicated on the declining presence of what are generally known as neutralizing antibodies, which might block the virus from attaching to a cell and replicating. However different kinds of antibodies stay within the system.
“There have even been research which have proven that simply because an antibody doesn’t neutralize, it doesn’t imply it could possibly’t do something,” Rey stated. For instance, she stated, by binding simply to some components of the spike protein, it might immediate different immune cells to affix the struggle.
COVID-19 and the unvaccinated
In the event you’ve by no means been uncovered to SARS-CoV-2 or to COVID-19 vaccines, the coronavirus gained’t encounter any custom-made antibodies or T cells on its approach to your respiratory system. Even when your immune system is wholesome, it takes every week to 10 days to remodel undifferentiated T cells into killers and get them in place to confront contaminated cells, Wherry stated. Throughout that point, the virus is replicating exponentially and spreading via the physique.
However when you’ve been immunized, you possibly can have killer T cells prepared in 4 days or fewer, Wherry stated. That head begin makes an enormous distinction in holding an an infection from raging uncontrolled.
Unvaccinated folks might however have some T cells able to defend on the first signal of an an infection, Weiskopf stated. Researchers discovered some T cells that responded to SARS-CoV-2 in samples taken from individuals who’d by no means been uncovered to the virus, she stated. These cells — created in response to the frequent chilly, which will be attributable to other forms of coronaviruses — helped velocity up and strengthen the immune response, she stated.
Not everybody who’s caught a chilly may have T cells with this type of versatility, she added. However the discovery suggests to some researchers that scientists would possibly be capable of devise a vaccine able to attacking any coronavirus variant by prompting the immune system to make T cells like these. (Dr. Patrick Quickly-Shiong, proprietor of The Instances, has one other firm that’s exploring this risk.)
At any charge, the extra a virus replicates within the physique, the larger the response from killer T cells. That raises a second situation, Wherry stated: T cells can’t go on killing tissue perpetually; in some unspecified time in the future, the system has to shift into restore mode. That’s why there are regulatory T cells to “act as a counterweight on this entire system,” serving to to rein within the killer cells, he stated.
Typically, nonetheless, the system doesn’t throw the “off” swap quickly sufficient. Wherry stated that for some significantly unwell COVID-19 sufferers, the virus spreads to many locations inside their our bodies, and an enormous variety of killer T cells flood their techniques with “very damaging” cytokines. Clinicians assist these sufferers by suppressing their immune techniques to tamp down this response, he stated.
Unvaccinated individuals who get better from COVID-19 may have antibodies and reminiscence cells to assist defend towards the subsequent encounter with SARS-CoV-2. However Rey stated an individual’s immune response is a lot better after vaccination than with the “pure immunity” conferred by an an infection. The reinfection charge for unvaccinated individuals who solely have pure immunity is twice as excessive because the an infection charge for individuals who’ve been vaccinated, she stated.
Immunological age
Over the course of the pandemic, aged folks have tended to endure way more critical penalties from COVID-19 than kids have. There seem like at the very least a few causes for that.
Rey pointed to a research led by researchers on the Charité-Universitätsmedizin Berlin, who discovered sure innate defenses in kids’s nasal passages that will assist them clobber the virus earlier than it could possibly replicate wildly.
“Any such innate immune response appears to be delayed in older adults, and in an effort to ‘catch up,’ might end in extreme irritation, thereby finally inflicting extra extreme harm,” she wrote in a weblog put up.
Wherry stated the immune system is prone to the results of ageing, identical to the remainder of the physique.
“One of many key issues is you lose manufacturing of those new, what we name ‘naive,’ T cells,” he stated. These act as clean slates, able to be taught new threats. Late in life, Wherry stated, “they turn out to be a a lot smaller portion of the cells you possibly can name into motion.”
As we age, issues emerge in different parts of the immune system as properly, he stated. Altogether, he stated, these points “make it more durable for the immune system to get out of the gate.”

Science
Blue Origin Scrubs New Glenn Rocket’s Debut Launch

Blue Origin’s New Glenn rocket is poised upright at Launch Complex 36 at Cape Canaveral Space Force Station in Florida.
Preparations began in earnest several hours before launch when liquid hydrogen started flowing into New Glenn’s propellant tanks.
At 10 minutes before liftoff time, the launch director will conduct a “go poll,” asking people whether the rocket’s systems are ready and whether the weather conditions are favorable.
The last four minutes before launch are the “terminal count” when the rocket’s computer takes over the countdown process.
The seven engines in the booster will ignite 5.6 seconds before liftoff. That gives the computer a chance to check the performance of the engines before committing to liftoff. If anything is not quite right, it will shut down the engines.
If everything is good, the clamps holding the rocket will let go, and New Glenn will rise into the sky.
A crucial moment will come one minute, 39 seconds after launch as the rocket passes through what is known as max-Q, when atmospheric pressure on the rocket is greatest.
If it passes through that moment intact, the booster during the third minute of the flight will be done pushing the rocket upward and the engines will shut down. Twelve seconds later, it will drop away, and nine seconds after that, the second-stage engine will fire up.
Not long afterward, the fairing — the two halves of the nose cone protecting the payload — will jettison. At that altitude, the atmosphere is thin enough that the fairing is no longer needed.
Over the next few minutes, the booster will light up twice as it tries to land on a floating platform named Jacklyn, after Jeff Bezos’ mother, in the Atlantic Ocean.
Meanwhile, the second-stage engine will continue to fire until nearly 13 minutes after launch and then shut down.
Blue Origin will then switch on a prototype of its Blue Ring space tug, testing the communications, power and computer systems. It will remain attached to the rocket’s second stage.
About an hour after launch, the second stage will perform another engine burn to push it into a high elliptical orbit, coming as close as 1,500 miles from Earth and swinging out as far away as 12,000 miles. That is much higher than launches to low-Earth orbit, a few hundred miles up.
In an interview on Sunday, Jeff Bezos, the founder of Blue Origin, said that orbit will allow testing of the communications systems at a wide variety of altitudes. “And it puts the vehicle in a very harsh radiation environment, which we also want to test,” he said.
Then, almost six hours after launch, the mission will be over. The systems on the rocket stage and Blue Ring will be made safe and turned off, and they will continue their elliptical orbiting. Few other satellites occupy that region, making the chances slim that it will collide with anything else.
“It gets disposed in place,” Mr. Bezos said.
Science
Some Raw Truths About Raw Milk

Today, however, a small but growing number of Americans prefer to drink their milk raw. And Robert F. Kennedy Jr., Donald Trump’s choice to lead the Department of Health and Human Services, now stands at the vanguard of this movement. Kennedy has said he drinks raw milk and has criticized what he describes as the Food and Drug Administration’s “aggressive suppression” of raw-milk production, among other things. Enthusiasts anticipate that, as H.H.S. secretary, he would make raw milk easier to acquire — although how remains unclear. Federal regulations prohibit the sale of raw milk across state lines, but where it’s legal, raw milk is regulated by state governments, not federal agencies.
In embracing raw milk, Kennedy is following an established trend as much as leading it. The roots of the movement stretch back decades. The small, independent health-food stores my parents frequented in New Mexico in the 1980s, for example, sold raw milk. (We never partook.) But to hear Mark McAfee tell it, the pandemic supercharged demand.
McAfee heads one of the largest producers of raw milk in the country, Raw Farm in California. McAfee, who has said Kennedy is a customer, has applied to serve in an advisory role at H.H.S. — at the urging of Kennedy’s transition team, he says. During the pandemic, McAfee told me, people felt abandoned by medical professionals and began researching ways to care for their own immune systems. Many turned to raw milk, which he calls “the first food of life.” Maybe they thought it could protect them from the coronavirus, he says, an unproven idea that may stem from the observation that human breast milk provides nursing infants with some protection against infection.
Anecdotes of seemingly miraculous cures from raw milk also help fuel the phenomenon — inflammatory diseases that go into remission, allergies and digestive problems that disappear. McAfee eagerly shared such stories. Nonetheless, his customers defy easy categorization. When he began selling raw milk 25 years ago, hippie “nut-and-berry moms” and natural foodies, as he puts it, formed McAfee’s core clientele. But as his sales have grown — about 30-fold since then, he estimates — his customers have diversified.
Today’s raw-milk movement is made up of people and ideas from across the political spectrum: back-to-the-land types seeking unadulterated whole foods; health fanatics seeking the latest superfood; don’t-tell-me-what-to-eat libertarians who distrust authority and who, in McAfee’s description, intend to do the opposite of whatever the F.D.A. says. A variety of labels have been applied to the movement: “food sovereignty,” “slow food,” “real food,” “food freedom.” For the more conspiratorially minded, raw milk represents food free of government meddling. For those merely chasing the latest fad, raw milk may be a status symbol — a single gallon can cost nearly $20.
Science
Far From the Fires, the Deadly Risks of Smoke Are Intensifying

It kills more people each year than car crashes, war or drugs do. This invisible killer is the air pollution from sources like cars and trucks or factory smokestacks.
But as wildfires intensify and grow more frequent in a warming world, the smoke from these fires is emerging as a new and deadly pollution source, health experts say. By some estimates, wildfire smoke — which contains a mixture of hazardous air pollutants like particulate matter, nitrogen dioxide, ozone and lead — already causes as many as 675,000 premature deaths a year worldwide, as well as a range of respiratory, heart and other diseases.
Research shows that wildfire smoke is starting to erode the world’s progress in cleaning up pollution from tailpipes and smokestacks, as climate change supercharges fires.
“It’s heartbreaking, it really is,” said Dr. Afif El-Hasan, a pediatrician who specializes in asthma care at Kaiser Permanente in Southern California and a board director of the American Lung Association. Wildfires “are putting our homes in danger, but they’re also putting our health in danger,” Dr. El-Hasan said, “and it’s only going to get worse.”
Those health concerns were coming to the fore this week as wildfires ravaged the Los Angeles area. Residents began to return to their neighborhoods, many strewed with smoldering ash and rubble, to survey the damage. Air pollution levels remained high in many parts of the city, including in northwest coastal Los Angeles, where the air quality index climbed to “dangerous” levels.
Los Angeles, in particular, has seen air pollution at levels that could be raising daily mortality by between 5 to 15 percent, said Carlos F. Gold, an expert in the health effects of air pollution at the University of California, San Diego.
That means current death counts, “while tragic, are likely large underestimates,” he said. People with underlying health issues, as well as older people and children, are particularly vulnerable.
The rapid spread of this week’s fires into dense neighborhoods, where they burned homes, furniture, cars, electronics and materials like paint and plastic, made the smoke more dangerous, said Dr. Lisa Patel, a pediatrician in the San Francisco Bay Area and the executive director of the Medical Society Consortium on Climate and Health.
A recent study found that even for homes that are spared destruction, smoke and ash blown inside could adhere to rugs, sofas and drywall, creating health hazards that can linger for months. “We’re breathing in this toxic brew of volatile organic compounds and polycyclic aromatic hydrocarbons and hexavalent chromium,” Dr. Patel said. “All of it is noxious.”
Intensifying and more frequent fires, meanwhile, are upending experts’ understanding of smoke’s health effects. “Wildfire season is no longer a season,” said Colleen Reid, who researches the effects of air pollution from wildfires on heath at the University of Colorado Boulder. “We have fires all year round that affect the same population repeatedly.”
“The health impacts are not the same as if you were exposed once, and then not again for 10 years,” she said. “The effects of that is something that we still don’t really know.”
A United Nations report from 2022 concluded that the risk of devastating wildfires around the world would surge in coming decades. Heating and drying caused by climate change, along with development in places vulnerable to fire, was expected to intensify a “global wildfire crisis,” the report said. Both the frequency and intensity of extreme wildfires have more than doubled in the past two decades. In the United States, the average acreage burned a year has surged since the 1990s.
Now, pollution from wildfires is reversing what had been a decades-long improvement in air quality brought about by cleaner cars and power generation. Since at least 2016, in nearly three-quarters of states in the U.S. mainland, wildfire smoke has eroded about 25 percent of progress in reducing concentrations of a type of particulate matter called PM 2.5, a Nature study in 2023 found.
In California, wildfire smoke’s effect on air quality is offsetting public health gains brought about by a decline in air pollution from automobiles and factories, state health officials have found. (By releasing carbon dioxide and other planet-warming gases into the atmosphere, wildfires are themselves a big contributor to climate change: The wildfires that ravaged Canada’s boreal forests in 2023 produced more greenhouse gases than the burning of fossil fuels in all but three countries.)
”It’s not a pretty picture,” said Dr. Gold of U.C. San Diego, who took part in the Nature study. If planet-warming gas emissions continue at current levels, “we’ve got some work that suggests that mortality from wildfire smoke in the U.S. could go up by 50 percent,” he said.
One silver lining is that the Santa Ana winds that so ferociously fueled the flames in recent days have been blowing some of the smoke toward the ocean. That stands in contrast to the smoke from the 2023 Canadian wildfires that drifted to New York and other American states hundreds of miles away, causing spikes in emergency room visits for asthma.
At one point that year, more than a third of Americans, from the East Coast to the Midwest, were under air quality alerts from Canadian wildfire smoke. “We’re seeing new and worsening threats in places that are not used to them,” Dr. Patel, the pediatrician, said.
The new normal is bringing about changes to health care, Dr. Patel said. More health systems are sending out air quality alerts to vulnerable patients. In the small community hospital where she works, “every child that comes in with wheezing or asthma, I talk to them about how air pollution is getting worse because of wildfires and climate change,” she said.
“I teach them how to look up air quality, and say they should ask for an air purifier,” Dr. Patel added. She also cautions that children should not participate in cleanup after a wildfire.
Scientists are still trying to understand the full range of wildfire smoke’s health effects. One big question is how much of what researchers know about vehicle exhaust and other forms of air pollution apply to wildfire smoke, said Mark R. Miller, a researcher at the Center for Cardiovascular Science at the University of Edinburgh who led a recent global survey of climate change, air pollution and wildfires.
For example, exhaust particles “are so small that when we breathe them in, they go deep down into our lungs and are actually small enough that they can pass from our lungs into our blood,” he said. “And once they’re in our blood, they can be carried around our body and start to build up.”
That means air pollution affects our entire body, he said. “It has effects on people who have diabetes, has effects on the liver and the kidney, it has effects on the brain, on pregnancy,” he said. What’s still not clear is whether pollution from wildfires has all of those same effects. “But it’s likely,” he said.
Experts have a range of advice for people living in areas with smoke. Keep an eye on air quality alerts, and follow evacuation orders. Stay indoors as much as possible, and use air purifiers. When venturing outside, wear N95 masks. Don’t do strenuous exercise in bad air. Keep children, older people and other vulnerable groups away from the worst smoke.
Ultimately, tackling climate change and cutting back on all kinds of air pollution is the way to reduce the overall burden on health, said Dr. El-Hasan of the American Lung Association. “Can you imagine how much worse things would be if we hadn’t started cleaning up emissions from our cars?” he said. “I’m trying to think, glass half full, but it does break my heart and it does worry me.”
-

 Politics1 week ago
Politics1 week agoWho Are the Recipients of the Presidential Medal of Freedom?
-

 Health1 week ago
Health1 week agoOzempic ‘microdosing’ is the new weight-loss trend: Should you try it?
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology4 days ago
Technology4 days agoMeta is highlighting a splintering global approach to online speech
-

 Science2 days ago
Science2 days agoMetro will offer free rides in L.A. through Sunday due to fires
-

 News1 week ago
News1 week agoSeeking to heal the country, Jimmy Carter pardoned men who evaded the Vietnam War draft
-

 Movie Reviews7 days ago
Movie Reviews7 days ago‘How to Make Millions Before Grandma Dies’ Review: Thai Oscar Entry Is a Disarmingly Sentimental Tear-Jerker
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology6 days ago
Technology6 days agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 News1 week ago
News1 week agoTrump Has Reeled in More Than $200 Million Since Election Day















