Science
Canny as a crocodile but dumber than a baboon — new research ponders T. rex's brain power

In December 2022, Vanderbilt University neuroscientist Suzana Herculano-Houzel published a paper that caused an uproar in the dinosaur world.
After analyzing previous research on fossilized dinosaur brain cavities and the neuron counts of birds and other related living animals, Herculano-Houzel extrapolated that the fearsome Tyrannosaurus rex may have had more than 3 billion neurons — more than a baboon.
As a result, she argued, the predators could have been smart enough to make and use tools and to form social cultures akin to those seen in present-day primates.
The original “Jurassic Park” film spooked audiences by imagining velociraptors smart enough to open doors. Herculano-Houzel’s paper described T. rex as essentially wily enough to sharpen their own shivs. The bold claims made headlines, and almost immediately attracted scrutiny and skepticism from paleontologists.
In a paper published Monday in “The Anatomical Record,” an international team of paleontologists, neuroscientists and behavioral scientists argue that Herculano-Houzel’s assumptions about brain cavity size and corresponding neuron counts were off-base.
True T. rex intelligence, the scientists say, was probably much closer to that of modern-day crocodiles than primates — a perfectly respectable amount of smarts for a therapod to have.
“What needs to be emphasized is that reptiles are certainly not as dim-witted as is commonly believed,” said Kai Caspar, a biologist at Heinrich Heine University Düsseldorf and co-author of the paper. “So whereas there is no reason to assume that T. rex had primate-like habits, it was certainly a behaviorally sophisticated animal.”
Brain tissue doesn’t fossilize, and so researchers examine the shape and size of the brain cavity in fossilized dinosaur skulls to deduce what their brains may have been like.
In their analysis, the authors took issue with Herculano-Houzel’s assumption that dinosaur brains filled their skull cavities in a proportion similar to bird brains. Herculano-Houzel’s analysis posited that T. rex brains occupied most of their brain cavity, analogous to that of the modern-day ostrich.
But dinosaur brain cases more closely resemble those of modern-day reptiles like crocodiles, Caspar said. For animals like crocodiles, brain matter occupies only 30% to 50% of the brain cavity. Though brain size isn’t a perfect predictor of neuron numbers, a much smaller organ would have far fewer than the 3 billion neurons Herculano-Houzel projected.
“T. rex does come out as the biggest-brained big dinosaur we studied, and the biggest one not closely related to modern birds, but we couldn’t find the 2 to 3 billion neurons she found, even under our most generous estimates,” said co-author Thomas R. Holtz, Jr., a vertebrate paleontologist at University of Maryland, College Park.
What’s more, the research team argued, neuron counts aren’t an ideal indicator of an animal’s intelligence.
Giraffes have roughly the same number of neurons that crows and baboons have, Holtz pointed out, but they don’t use tools or display complex social behavior in the way those species do.
“Obviously in broad strokes you need more neurons to create more thoughts and memories and to solve problems,” Holtz said, but the sheer number of neurons an animal has can’t tell us how the animal will use them.
“Neuronal counts really are comparable to the storage capacity and active memory on your laptop, but cognition and behavior is more like the operating system,” he said. “Not all animal brains are running the same software.”
Based on CT scan reconstructions, the T. rex brain was probably “ a long tube that has very little in terms of the cortical expansion that you see in a primate or a modern bird,” said paleontologist Luis Chiappe, director of the Dinosaur Institute at the Natural History Museum of Los Angeles County.
“The argument that a T. Rex would have been as intelligent as a primate — no. That makes no sense to me,” said Chiappe, who was not involved in the study.
Like many paleontologists, Chiappe and his colleagues at the Dinosaur Institute were skeptical of Herculano-Houzel’s original conclusions. The new paper is more consistent with previous understandings of dinosaur anatomy and intelligence, he said.
“I am delighted to see that my simple study using solid data published by paleontologists opened the way for new studies,” Herculano-Houzel said in an email. “Readers should analyze the evidence and draw their own conclusions. That’s what science is about!”
When thinking about the inner life of T. rex, the most important takeaway is that reptilian intelligence is in fact more sophisticated than our species often assumes, scientists said.
“These animals engage in play, are capable of being trained, and even show excitement when they see their owners,” Holtz said. “What we found doesn’t mean that T. rex was a mindless automaton; but neither was it going to organize a Triceratops rodeo or pass down stories of the duckbill that was THAT BIG but got away.”

Science
As national wastewater testing expands, Texas researchers identify bird flu in nine cities

As researchers increasingly rely on wastewater testing to monitor the spread of bird flu, some are questioning the reliability of the tests being used. Above, the Hyperion Water Reclamation Plant in Playa Del Rey.
(Jason Armond / Los Angeles Times)
As health officials turn increasingly toward wastewater testing as a means of tracking the spread of H5N1 bird flu among U.S. dairy herds, some researchers are raising questions about the effectiveness of the sewage assays.
Although the U.S. Centers for Disease Control and Prevention says current testing is standardized and will detect bird flu, some researchers voiced skepticism.
“Right now we are using these sort of broad tests” to test for influenza A viruses in wastewater, said epidemiologist Denis Nash, referring to a category of viruses that includes normal human flu and the bird flu that is circulating in dairy cattle, wild birds, and domestic poultry.
“It’s possible there are some locations around the country where the primers being used in these tests … might not work for H5N1,” said Nash, distinguished professor of epidemiology and executive director of City University of New York’s Institute for Implementation Science in Population Health.
The reason for this is that the tests most commonly used — polymerase chain reaction, or PCR, tests — are designed to detect genetic material from a specific organism, such as a flu virus.
But in order for them to identify the virus, they must be “primed” to know what they are looking for. Depending on what part of the virus researchers are looking for, they may not identify the bird flu subtype.
There are two common human influenza A viruses: H1N1 and H3N2. The “H” stands for hemagglutinin, which is an identifiable protein in the virus. The “N” stands for neuraminidase.
The bird flu, on the other hand, is also an influenza A virus. But it has the subtype H5N1.
That means that while the human and avian flu virus share the N1 signal, they don’t share an H.
If a test is designed to look for only the H1 and H3 as indicators of influenza A virus, they’re going to miss the bird flu.
Marc Johnson, a professor of molecular microbiology and immunology at the University of Missouri, said he doesn’t think that’s too likely. He said the generic panels that most labs use will capture H1, H3 and H5.
He said while his lab specifically looks for H1 and H3, “I think we may be the only ones doing that.”
It’s been just in the last few years that health officials have started using wastewater as a sentinel for community health.
Alexandria Boehm, professor of civil and environmental engineering at Stanford University and principal investigator and program director for WastewaterSCAN, said wastewater surveillance really got going during the pandemic. It’s become a routine way to look for hundreds if not thousands of viruses and other pathogens in municipal wastewater.
“Three years or four years ago, no one was doing it,” said Boehm, who collaborates with a network of researchers at labs at Stanford, Emory University and Alphabet Inc.’s life sciences research organization. “It sort of evolved in response to the pandemic and has continued to evolve.”
Since late March, when the bird flu was first reported in Texas dairy cattle, researchers and public health officials have been combing through wastewater samples. Most are using the influenza A tests they had already built into their systems — most of which were designed to detect human flu viruses, not bird flu.
On Tuesday, the CDC released its own dashboard showing wastewater sites where it has detected influenza A in the last two weeks.
Displaying a network of more than 650 sites across the nation, there were only three sites — in Florida, Illinois and Kansas — where levels of influenza A were considered high enough to warrant further agency investigation. There were more than 400 where data were insufficient to allow a determination.
Jonathan Yoder, deputy director of the CDC’s Division of Infectious Disease Readiness and Innovation, said those sites were deemed to have insufficient data because testing hasn’t been in place long enough, or there may not have been enough positive influenza A samples to include.
Asked if some of the tests being used could miss bird flu because of the way they were designed, he said: “We don’t have any evidence of that. It does seem like we’re at at a broad enough level that we don’t have any evidence that we would not pick up H5.”
He also said the tests were standardized across the network.
“I’m pretty sure that it’s the same assay being used at all the sites,” he said. “They’re all based on … what the CDC has published as a clinical assay for for influenza A, so it’s based on clinical tests.”
But there are discrepancies between the CDC’s findings and others’.
Earlier this week, a team of scientists from Baylor College of Medicine, the University of Texas Health Science Center at Houston, the Texas Epidemic Health Institute and the El Paso Water Utility, published a report showing high levels of bird flu from wastewater in nine Texas cities. Their data show that H5N1 is the dominant form of influenza A swirling in these Texas towns’ wastewater.
But unlike other research teams, including the CDC, they used an “agnostic” approach known as hybrid-capture sequencing.
“So it’s not just targeting one virus or one of several viruses,” as one does with PCR testing, said Eric Boerwinkle, dean of the UTHealth Houston School of Public Health and a member of the Texas team. “We’re actually in a very complex mixture, which is wastewater, pulling down viruses and sequencing them.”
“What’s critical here is it’s very specific to H5N1,” he said, noting they’d been doing this kind of testing for approximately two years, and hadn’t ever seen H5N1 before the middle of March.
Blake Hanson, an assistant professor at the University of Texas Health Science Center at Houston School of Public Health and a member of the Texas wastewater team, agreed, saying that PCR-based methods are “exquisite” and “highly accurate.”
“But we have the ability to look at the representation of the entire genome, not just a marker component of it. And so that has allowed us to look at H5N1, differentiate it from some of our seasonal fluids like H1N1 and H3N2,” he said. “It’s what gave us high confidence that it is entirely H5N1, whereas the other papers are using a part of the H5 gene as a marker for H5.”
Boerwinkle and Hanson underscored that while they could identify H5N1 in the wastewater, they cannot tell where it came from.
“Texas is really a confluence of a couple of different flyways for migratory birds, and Texas is also an agricultural state, despite having quite large cities,” Boerwinkle said. “It’s probably correct that if you had to put your dime and gamble what was happening, it’s probably coming from not just one source but from multiple sources. We have no reason to think that one source is more likely any one of those things.”
But they are pretty confident it’s not coming from people.
“Because we are looking at the entirety of the genome, when we look at the single human H5N1 case, the genomic sequence … has a hallmark amino acid change … compared to all of the cattle from that same time point,” Hanson said. “We do not see that hallmark amino acid present in any of our sequencing data. And we’ve looked very carefully for that, which gives us some confidence that we’re not seeing human-human transmission.”
The Texas’ team approach was really exciting, said Devabhaktuni Srikrishna, the CEO and founder of PatientKnowHow.com, noting it exhibited “proof of principle” for employing this kind of metagenomic testing protocol for wastewater and air.
He said government agencies, private companies and academics have been searching for a reliable way to test for thousands of microscopic organisms — such as pathogens — quickly, reliably and at low cost.
“They showed it can be done,” he said.
Science
Deadly overdoses fell in U.S. for first time in five years, new estimates show

Deaths from drug overdoses fell last year in the United States as fewer people lost their lives to fentanyl and other opioids, marking the first time the death toll had dropped in five years, according to newly released estimates from the Centers for Disease Control and Prevention.
Federal officials said the numbers show a 3% decline in the estimated overdose fatalities between 2022 and 2023. That downturn equates to nearly 3,500 fewer deaths across the U.S. than the year before.
The new figures are tentative and could still be updated. Even a slight decline could be a balm for a country where drug overdoses have taken a devastating toll: In one survey, more than 40% of adults said they knew someone who lost their life to a drug overdose, according to a Rand study published this year.
“I’m thrilled that there wasn’t an increase, but we’re still talking about 107,000 people dying, which is completely unacceptable,” said Beau Kilmer, co-director of the Rand Drug Policy Research Center. Kilmer said better data on drug use are needed to untangle exactly what is driving the changes.
Community groups and health officials grappling with the devastating toll of fentanyl have pushed to equip more people with naloxone, a medicine that can stop opioid overdoses and is commonly sold as a nasal spray under the brand name Narcan. Los Angeles County officials, for instance, credited an effort to hand out Narcan on the streets when they announced last week that overdose deaths had stopped surging among homeless people. To try to reduce the deadly risks, people who use drugs have also turned to test strips to detect fentanyl and avoided using drugs by themselves, among other strategies.
Health researchers have also noted that broader changes in the population could be affecting the numbers: Many heroin users who switched to fentanyl have died, and if fewer people are newly turning to fentanyl use, that could mean fewer people are now at risk, said Dr. Daniel Ciccarone, a UCSF addiction medicine professor.
“Based on utterly anecdotal, street-level observations, I’ll say there aren’t a lot of newbies,” Ciccarone said. “We’re looking for them, but we don’t see them. We don’t see the 22-year-old who says, ‘Hey, I want to use fentanyl.’ This is an aging cohort.”
Even as U.S. deaths linked to fentanyl and other opioids dropped between 2022 and 2023, the country saw an uptick in deaths tied to stimulants such as methamphetamine and cocaine, according to the new estimates. Drug researchers said that in recent years, many deaths involving meth have also involved opioids.
And not all parts of the country saw an overall drop in fatal overdoses. “In the East Coast and in the Midwest, we are seeing declines, but on the West Coast — particularly in the upper Northwest — we’re still seeing increases,” said Farida Ahmad, a health scientist at the National Center for Health Statistics.
The federal figures show that in California, the estimated number of overdose deaths continued to rise in 2023 compared with 2022, increasing by 4.1%. In Oregon and Washington, increases were significantly steeper — roughly 30% and 27% respectively.
Drug use can differ from region to region, shaping ensuing overdoses and deaths: Fentanyl hit the eastern U.S. before spreading west, and methamphetamine use generally has been more common on the West Coast.
Ciccarone lamented that the West Coast should have been better prepared for fentanyl after seeing it hit other parts of the country years earlier, calling it a “failure of public policy.”
“We saw this coming. So why didn’t we prepare for it better?”
Ciccarone credited states in the Midwest and East Coast that had seen notable decreases in overdose deaths, saying that although the exact reasons are unclear, there has been a panoply of efforts that could play a role, including ramping up naloxone distribution and easing access to buprenorphine to treat opioid addiction.
“These are places that were hard hit by fentanyl,” Ciccarone said. “So they’re doing something right.”
The federal estimates released Wednesday do not detail how many deaths linked to methamphetamine also involved other drugs, a phenomenon that has gained growing attention as American mix drugs both knowingly and unknowingly.
Researchers drawing on both federal and local data have found substantial overlap in methamphetamine and opioid use: In L.A. County, for instance, a recent report indicated that in 2022, nearly half of overdose deaths among homeless people involved both methamphetamine and fentanyl.
People who use fentanyl may turn to stimulants for energy to get themselves through daily activities, said Chelsea Shover, an assistant professor at UCLA’s David Geffen School of Medicine. For those facing the dangers of living outside, “you know what helps you stay up at night and stay vigilant? Meth.”
Shover said in recent years, national data have consistently shown the majority of methamphetamine deaths also involve opioids. Those findings were echoed in local research by Shover and other researchers, which found that between 2012 and mid-2021, the bulk of meth-related deaths in L.A. County also involved other drugs or medical conditions, rather than being driven solely by the stimulant.
To help prevent such deaths, “we need to keep doing what we’re doing for opioid-related deaths — because a lot of meth-involved deaths are also opioid-involved,” Shover said.
Scholars have also urged more attention to methamphetamine itself: As it stands, there are no medications approved by the Food and Drug Administration to treat addiction to meth, although some existing medicines have shown promising results, as has offering incentives such as gift cards for people to stay off stimulants.
“The massive investment in reducing overdose deaths has been almost exclusively targeted to opioids,” said Steven Shoptaw, director of the UCLA Center for Behavioral and Addiction Medicine. “There’s been no systematic investment to reduce methamphetamine deaths” — a lapse that Shoptaw said had hindered effective interventions from being widely adopted.
Americans have been eager for any signs of hope amid the overdose crisis, but experts have cautioned against declaring victory too soon in reaction to year-to-year changes in overdose deaths.
For instance, University of Pittsburgh researchers found that the last time fatal overdoses dropped nationally in 2018, the downturn coincided with stricter regulations in China on carfentanil, a highly potent synthetic opioid. The following year, deaths from drug overdoses rose again.
Dr. Donald Burke said that the estimated number of overdose deaths in 2023 was still above the level that researchers had forecast, based on the historic trajectory of such fatalities. The death numbers had jumped higher than expected during the COVID-19 pandemic, Burke said — and may just be returning to the same levels that would have happened in its absence.
“You can make a case that it’s come down, but it’s come down because the COVID impact is less now,” said Burke, dean emeritus of the University of Pittsburgh School of Public Health.
“Without knowing what are the drivers, it’s really hard to tell whether a reduction is a return to the expected trajectory or some other change,” said Dr. Hawre Jalal, an associate professor at the University of Ottawa who has partnered with Burke on such research.
Ciccarone was reluctant to even characterize the newly released estimates as a decrease in overdose deaths, instead referring to “a flattening of the curve.”
“Can we sing hosannas over that? No,” Ciccarone said. “We’re still fighting. We still have a lot of work to do to bend this overdose curve down.”
Science
Despite its 'nothingburger' reputation, COVID-19 remains deadlier than the flu

Since the earliest days of the pandemic, health officials have gauged the threat of COVID-19 by comparing it to the flu.
At first, it wasn’t even close. People hospitalized in 2020 with the then-novel respiratory disease were five times more likely to die of their illness than were patients who had been hospitalized with influenza during the preceding flu seasons.
Immunity from vaccines and past coronavirus infections has helped tame COVID-19 to the point that when researchers compared the mortality rates of hospitalized COVID-19 and seasonal influenza patients during the height of the 2022-23 flu season, they found that the pandemic disease was only 61% more likely to result in death.
Now the same researchers have analyzed data for the the fall and winter of 2023 and 2024. Dr. Ziyad Al-Aly, director of the Clinical Epidemiology Center at the VA St. Louis Health Care System, and his colleagues expected to find that the two respiratory diseases had finally equalized.
“There’s a narrative out there that the pandemic is over, that it’s a nothingburger,” Al-Aly said. “We came into this thinking we would do this rematch and find it would be like the flu from now on.”
The VA team examined electronic health records of patients treated in Veterans Affairs hospitals in all 50 states between Oct. 1 and March 27. They zeroed in on patients who were admitted because they had fevers, shortness of breath or other symptoms due to either COVID-19 or influenza. (People who were admitted for another reason, such as a heart attack, and were then found to have a coronavirus infection weren’t included in the analysis.)
The COVID-19 patients were a little older, on average, than the flu patients (73.9 versus 70.2 years old), and they were less likely to be current or former smokers. They were also more likely to have received at least three doses of COVID-19 vaccine and less likely to have shunned the shots altogether.
Yet after Al-Aly and his colleagues accounted for these differences and a host of other factors, they found that 5.7% of the COVID-19 patients died of their disease, compared with 4.2% of the influenza patients.
In other words, the risk of death from COVID-19 was still 35% greater than it was for the flu. The findings were published Wednesday in the Journal of the American Medical Assn.
“There is undeniably an impression out there that [COVID-19] is no longer a major threat to human health,” Al-Aly said. “I think it’s largely driven by opinion and an emotional itch to move beyond the pandemic, to put it all behind us. We want to believe that it’s like the flu, and we did — until we saw the data.”
Dr. Peter Chin-Hong, an infectious diseases specialist at UC San Francisco, said the study results are right in line with what he sees in his hospital.
“COVID continues to make some people in our community very ill and die — even in 2024,” he said. “Although most will not get seriously ill from COVID, for some people it is like 2020 all over again.”
That’s particularly true for people who are older, who haven’t received their most recent recommended COVID-19 booster, and who haven’t taken full advantage of antivirals such as Paxlovid. Chin-Hong noted that only 5% of the COVID-19 patients in the study had been treated with antivirals before they were hospitalized.
Even if the mortality rates for the COVID-19 and flu patients had been equal, COVID-19 would still be the bigger health threat because it is sending more people to the hospital, Al-Aly said.
Between Oct. 1 and the end of March, 75.5 out of every 100,000 Americans had been hospitalized with influenza, according to the Centers for Disease Control and Prevention. During that same period, the hospitalization rate for COVID-19 was 122.9 per 100,000 Americans, the CDC says.
“COVID still carries a higher risk of hospitalization,” Al-Aly said. “And among those hospitalized, more will die as a result.”
Yet Al-Aly noted with frustration that while 48% of adults in the U.S. received a flu shot this year, only 21% of adults are up to date with their COVID-19 vaccinations, according to the CDC.
Chin-Hong added that more than 95% of adults hospitalized with COVID-19 this past fall and winter had not received the latest booster shot, according to the CDC.
Considering all the tools available to prevent hospitalizations and deaths — and especially the fact that they are readily available to patients in the VA system — the 35% relative risk of death from COVID-19 compared with the flu was “surprisingly high,” Chin-Hong said.
And it’s not like the flu is a trivial health threat, especially for senior citizens and people who are immunocompromised. It routinely kills tens of thousands of Americans each year, CDC data show.
“Influenza is a consequential infection,” Al-Aly said. “Even when COVID becomes equal to the flu, it’s still sobering and significant.”
The researchers also compared the mortality rates of VA COVID-19 patients before and after Dec. 24, when the Omicron subvariant known as JN.1 became the dominant strain in the United States. The difference was not statistically significant.
In just the last two weeks, JN.1 appears to have been overtaken by one of its descendants, a subvariant known as KP.2. It’s part of a family of subvariants that’s taken on the nickname “FLiRT,” a moniker that references some of the mutations that have cropped up on the viruses’ spike proteins.
So far, there’s no indication that KP.2 is any more dangerous than JN.1, Al-Aly said.
“Are the hospitals filling up? No,” he said. “Are ER rooms all over the country flooded with respiratory illness? No.” Nor are there worrying changes in the amount of coronavirus detected in wastewater.
“When you look at all these data streams, we’re not seeing ominous signs that KP.2 is something the general public should worry about,” Al-Aly said.
It’s also too early to tell whether KP.2 — or whatever comes after it — will finally erase the mortality gap between COVID-19 and the flu, he added.
“Maybe when we do a rematch in 2025, that will be the case,” he said.
-

 News1 week ago
News1 week agoMan, 75, confesses to killing wife in hospital because he couldn’t afford her care, court documents say
-

 World1 week ago
World1 week agoPentagon chief confirms US pause on weapons shipment to Israel
-

 Politics1 week ago
Politics1 week agoRFK Jr said a worm ate part of his brain and died in his head
-

 World1 week ago
World1 week agoConvicted MEP's expense claims must be published: EU court
-

 Politics1 week ago
Politics1 week agoBiden takes role as bystander on border and campus protests, surrenders the bully pulpit
-

 Politics1 week ago
Politics1 week agoHere's what GOP rebels want from Johnson amid threats to oust him from speakership
-

 World1 week ago
World1 week agoPro-Palestine protests: How some universities reached deals with students
-
 Politics1 week ago
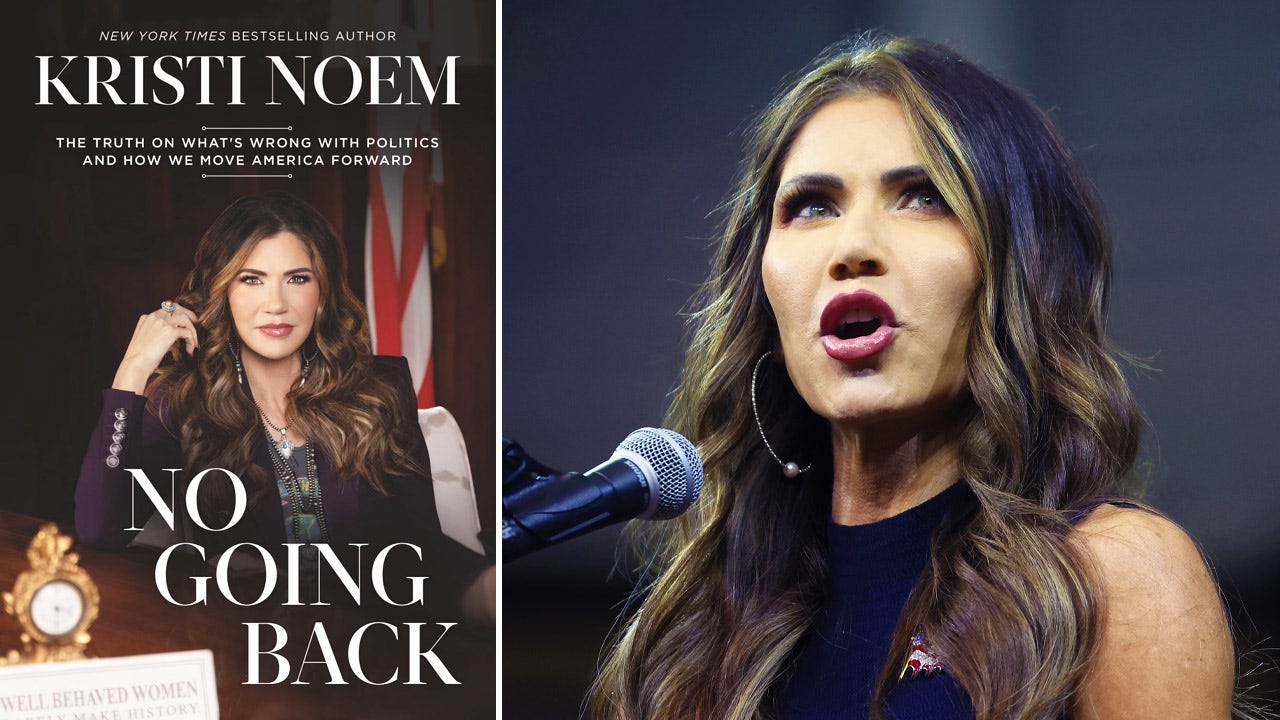
Politics1 week ago'You need to stop': Gov. Noem lashes out during heated interview over book anecdote about killing dog















