Health
Chicago nurse is finally free of COVID-19-related PTSD and depression after electrical brain tapping therapy

A Chicago nurse has been liberated from her own mind, thanks to a brain-tapping technology called deep TMS.
Gulden, who requested to omit her surname for privacy reasons, worked as a nurse for more than 40 years before COVID-19 rocked the hospital system and took a toll on her mental health.
The mother of four worked at Advocate South Suburban Hospital in Hazel Crest, Illinois, as an ICU and ER nurse.
ARTIFICIAL INTELLIGENCE NOT ALWAYS HELPFUL FOR REDUCING DOCTOR BURNOUT, STUDIES SUGGEST
In an interview with Fox News Digital, Gulden described the “massive chaos” that the 2020 coronavirus pandemic brought to the hospital.
“No matter what we did, it was like a failure,” she said. “We were not prepared [for] the onslaught of patients.”
Housekeeper Tonia Harvey changes a bed in the Roseland Community Hospital intensive care unit after a COVID-19 patient passed away, April 17, 2020. (E. Jason Wambsgans/Chicago Tribune/Tribune News Service via Getty Images)
“The predictable outcome of coming in through the ER and leaving in a body bag was just devastating.”
Despite her many years of medical work, New York City-born Gulden admitted that she “could not cope with it.”
By Sept. 2020, she was a “different person,” she said.
“I was on autopilot. I lived at work and when I came home, I was not functioning … My organization and concentration skills were gone.”
NURSES CALL FOR CHANGE AS MANY REVEAL THEY’RE ‘EXTREMELY LIKELY’ TO LEAVE PROFESSION: ‘EMOTIONAL, STRESSFUL’
“It was very, very unlike me, because I’m a single mom. I’ve raised four kids all by myself … but I started to notice that I could not let go of what had transpired during the day.”
Gulden told her primary care provider about her symptoms, including “horrible nightmares” that prevented her from sleeping and constant “weeping” that came “from her soul.”

Gulden, pictured here, said that working in a hospital during the coronavirus pandemic turned her into a “different person.” (Melanie Eilers)
In the span of two years, the doctor prescribed Gulden eight different medications for sleep, PTSD and major depressive disorder, along with cognitive behavior therapy — but nothing worked.
Even after the pandemic began to slow down, the nurse described how she hit a “spiral” when she realized COVID-19 created a “chain reaction.”
AMERICANS NEED MORE SLEEP, LESS STRESS, EXPERTS SAY, AS GALLUP POLL REVEALS TROUBLING FINDINGS
“[There] was a 51-year-old who had bilateral tumors and needed a mastectomy,” she shared. “She’d gone through all her chemo and radiation, and she was ready for her mastectomy, but she had to wait like 11 months.”
Added Gulden, “By the time she came back, her tumors had grown back, and that’s when I was like, This is never going to be over.”
Gulden mentioned that screenings for major health complications were down at least 84% during the pandemic, feeding into a “ripple” of patients who received care too late.

Tamara Jones gives antibiotics to James Davis as he recovers from COVID-19 in the intensive care unit at Roseland Community Hospital on Dec. 16, 2020, in Chicago, Illinois. (Scott Olson/Getty Images)
The nurse said through tears that she decided to leave the hospital and retire, since she “just couldn’t function there.”
After leaving, she fell into a “hibernation state” of sleeping 16 to 18 hours a day.
“The only reason I got up was to go to the bathroom,” she said. “And I’m embarrassed to say I would go weeks without showering.”
KETAMINE THERAPY SHOWN EFFECTIVE IN TREATING SEVERE DEPRESSION IN VETERANS, STUDY FINDS
“I lost 54 pounds — I got to the point where I couldn’t eat, because everything in the refrigerator reminded me of what was on patients’ trays.”
Gulden’s “incredibly vivid, horrible nightmares” continued along with other symptoms, including the inability to stay awake. She called it a “complete shutdown.”

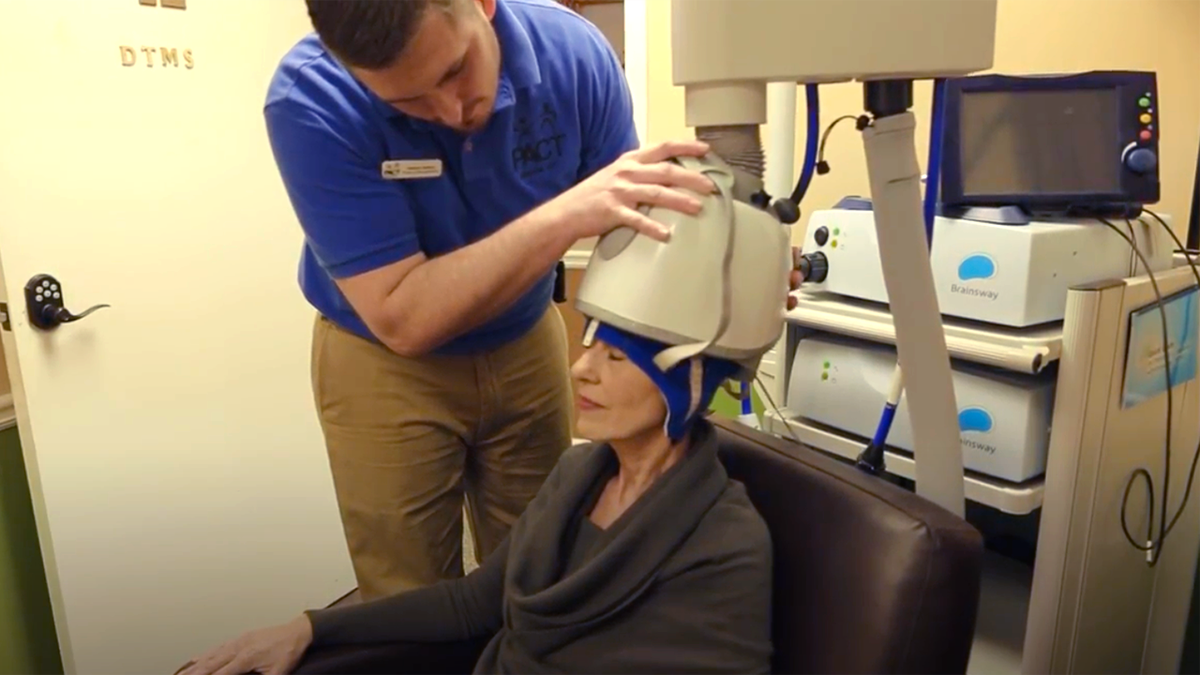
Gulden received deep TMS treatment at Relief Mental Health in Orland Park, Illinois. (Melanie Eilers)
After Gulden spent three years in “hibernation,” a friend introduced her to a new type of mental health treatment called deep TMS (transcranial magnetic stimulation) — a magnetized tapping of the brain used to treat various disorders and diseases.
Gulden agreed to visit Dr. Teresa Poprawski, the chief medical officer of Relief Mental Health in Orland Park, Illinois, who helped “put the threads together” on what was triggering her PTSD and other symptoms.
What is deep TMS?
Dr. Aaron Tendler, a psychiatrist and chief medical officer of BrainsWay, a brain disorder treatment company, discussed how the therapy works in an interview with Fox News Digital.
Tendler is based in West Palm Beach, Florida and was not involved in Gulden’s care. He said the brain is primarily an “electrochemical organ” that sends messages to different parts of the body.
‘PANDEMIC SKIP,’ A COVID MENTAL HEALTH PHENOMENON, COULD DELAY MAJOR MILESTONES, EXPERTS SAY
Most symptoms, including depression and anxiety, are controlled by changes in the brain, Tendler said, which can be treated electrically.
Deep TMS is a more “targeted” approach than electroshock therapy, he told Fox News Digital.

Gulden described the sensation of deep TMS as “tapping on specific parts of the brain.” (iStock; BrainsWay)
“Transcranial magnetic stimulation uses the principle of electromagnetic induction, where magnetic pulses induce an electrical current inside of neurons,” he said.
“Essentially, we are changing the electrical activity in a group of neurons in an area of the brain.”
COVID-19 PANDEMIC HAS CAUSED ‘COLLECTIVE TRAUMA’ AMONG US ADULTS, NEW POLL SAYS
These magnetic pulses only stimulate a specific area of the brain for “a brief period of time,” he said, with treatments lasting anywhere from six to 20 minutes. Patients undergo treatments for a series of days, depending on what’s necessary.
Tendler described the therapy as a “learning experience” that changes “the state of the brain” through repetitive treatment.

Deep TMS interrupts activity in the brain that is creating unwanted patterns, an expert said. (BrainsWay)
Gulden received deep TMS treatments for five days a week, for six to eight weeks. She described the sensation as “tapping on specific parts of the brain.”
After three weeks, she reported a noticeable difference in her cognitive state.
“I realized, ‘Oh my gosh, it’s been three years since I’ve heard the birds,’” she said. “I see life again. I see my flowers. Before, I couldn’t even look at the flowers because they just reminded me of funerals.”
PASTOR BASED IN DALLAS SHARES DEPRESSION JOURNEY, URGES OTHERS TO SEEK HELP: ‘DON’T HESITATE’
Gulden described her quality of life as “just so much better” since receiving treatment.
She still attends cognitive behavioral therapy sessions to hone her coping skills, she said.
“And if I need deep TMS again, I will be back there in a heartbeat,” she added.

Deep TMS is covered by “every insurer” across the country, according to one expert. (BrainsWay)
‘Very useful tool’
Gulden’s goal is to teach others to not feel ashamed about seeking help for their mental health struggles.
“I want people to know that there are interventions,” she said.
“The meds did not work for me. Had I not had this treatment today, I don’t know where I’d be.”
Although deep TMS technology was developed in the 1980s, the first treatment application for depression was FDA-cleared in 2009. (BrainsWay)
Most patients experience a 40% to 50% improvement after four weeks of treatment, according to Tendler.
After completing a typical course of 36 treatments, patients have shown 75% to 80% improvement, he said.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Deep TMS is “not a cure,” Tendler said — but many patients are able to regain normal function for months or years at a time.
The electrical therapy doesn’t have the potential side effects that antidepressants and other treatments can cause, Tendler said, noting that the brain manipulation is “temporary.”

“Had I not had this treatment today, I don’t know where I’d be,” Gulden said. (Melanie Eilers)
“I know this might sound like a disadvantage, but it is also an advantage,” he said. “We don’t do anything to the person’s brain that’s permanent. We’re changing the state of the brain temporarily.”
He added, “Generally, we get you out of the state that you were in … and then nature takes its course.”
Deep TMS can also be paired with other medications, such as antidepressants, Tendler added.
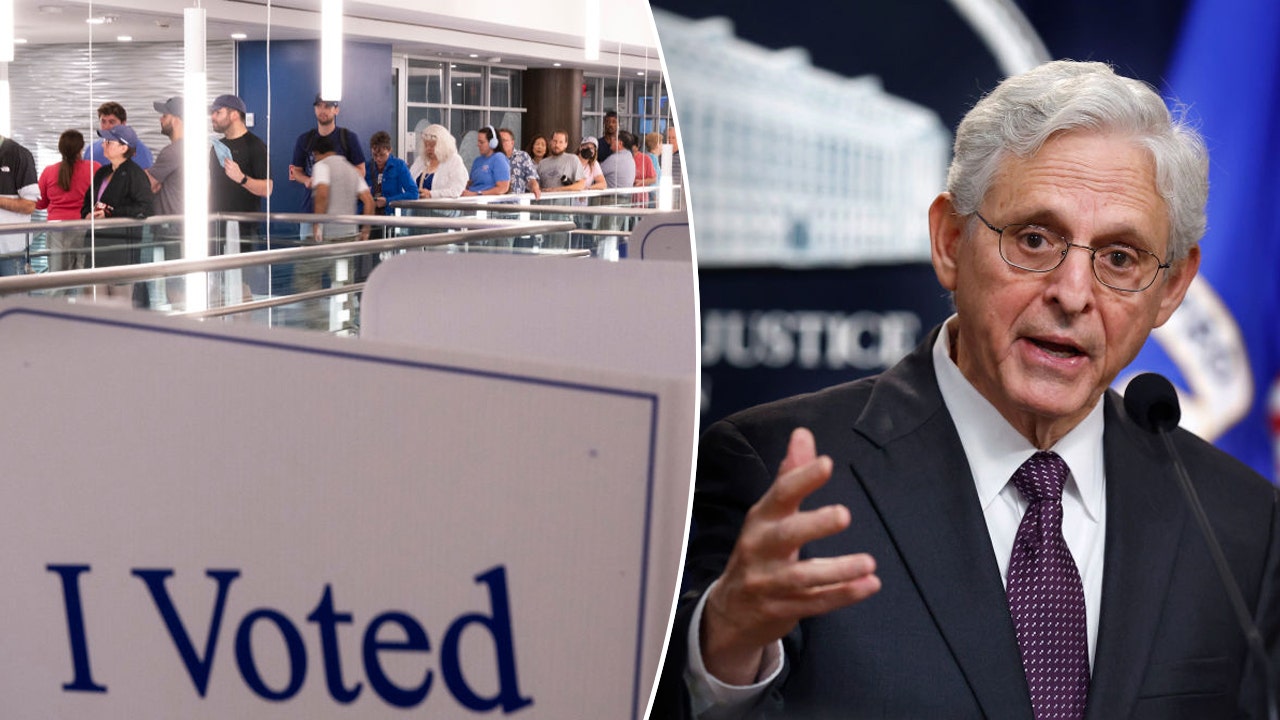
Fox News medical contributor Dr. Marc Siegel cautioned that deep TMS could potentially cause some cognitive and behavioral changes, but called it a “very useful tool” overall. (Dr. Marc Siegel)
Fox News medical contributor Dr. Marc Siegel cautioned that deep TMS could potentially cause some cognitive and behavioral changes, but called it a “very useful tool” overall.
He told Fox News Digital that deep TMS is also “very useful for movement disorders like Parkinson’s, with a high rate of success.”
“We’re changing the state of the brain temporarily.”
Siegel cautioned that deep TMS could potentially cause some cognitive and behavioral changes, but called it a “very useful tool” overall.
“[Deep TMS is] still being investigated for various purposes to interrupt aberrant nerve conduction,” he said.
For other medical professionals suffering from mental health issues, Gulden stressed the importance of having a “healthy health care team,” especially following the pandemic.
“I don’t care how tough you think you are,” she said. “You need to know what the signs are, and you need to know what treatments are available.”
For more Health articles, visit foxnews.com.com/health.

Health
Just Walking Can Help You Lose Weight: Try These Simple Fat-Burning Tips!

Sign Up
Create a free account to access exclusive content, play games, solve puzzles, test your pop-culture knowledge and receive special offers.
Already have an account? Login
Use left and right arrow keys to navigate between menu items.
Use escape to exit the menu.
Health
Pig infected with bird flu for first time in US, health officials confirm

A pig in Oregon has tested positive for H5N1 bird flu, according to a Wednesday announcement from the U.S. Department of Agriculture (USDA).
The infected pig was from a backyard farming operation that had a “mix of poultry and livestock,” the press release stated.
The USDA National Veterinary Services Laboratories confirmed that this was the “first detection of H5N1 in swine” in the U.S.
TUBERCULOSIS HAS OVERTAKEN COVID AS WORLD’S DEADLIEST INFECTIOUS DISEASE
“The livestock and poultry on this farm shared water sources, housing and equipment; in other states, this combination has enabled transmission between species,” the release noted.
A pig in Oregon (not pictured) has tested positive for H5N1 bird flu, according to a Wednesday announcement from the U.S. Department of Agriculture. (iStock)
The infected pig did not display symptoms of illness, but was tested — along with four other swine — out of “an abundance of caution” after other animals on the farm tested positive.
“There is no concern about the safety of the nation’s pork supply as a result of this finding.”
Out of the other five pigs tested, two were negative and two still have pending results.
“This farm is a non-commercial operation, and the animals were not intended for the commercial food supply,” the USDA stated.
LASSA FEVER DEATH REPORTED IN MIDWESTERN STATE, CONTACT TRACING BEGINS
“There is no concern about the safety of the nation’s pork supply as a result of this finding.”
The farm has been placed under quarantine to prevent further spread of bird flu, and the other animals are being monitored, per the USDA.
Doctors weigh in
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Health and Fox News Senior Medical Analyst, noted that cattle are “definitely now a reservoir” for H5N1.
“A solo pig isn’t concerning except for two things — how many more have it that we don’t know about, and that pigs are a mixing vessel for flu,” he told Fox News Digital.

The infected pig (not pictured) was from a backyard farming operation that had a “mix of poultry and livestock,” the press release stated. (iStock)
“There can be several different kinds of flu in swine at any given time, and they can exchange genetic material, creating new strains,” the doctor cautioned.
The 2009 H1N1 pandemic, though “mild by pandemic standards,” involved a swine flu, Siegel noted.
Added the doctor, “Continued spread in the pig population would concern me.”
E. COLI OUTBREAK LINKED TO MCDONALD’S BURGERS: HOW TO SPOT THE SYMPTOMS
Dr. Benjamin Anderson, PhD, assistant professor in the Department of Environmental and Global Health at the University of Florida, noted that while this appears to be an isolated event, there is still “some cause for concern.”
The doctor echoed Siegel’s concern that swine are a known “mixing vessel” for influenza A viruses, “as they are able to be infected by avian and human influenza virus strains.”

“There can be several different kinds of flu in swine at any given time, and they can exchange genetic material, creating new strains,” a doctor warned. (iStock)
“If H5N1, an avian influenza virus, were to regularly transmit among pigs, the greatest concern is that the genetic material from other influenza virus strains circulating in pigs may recombine with it to make a new progeny virus that is more transmissible to humans,” Anderson told Fox News Digital.
The fact that all five of the pigs at the farm were not clinically ill is also concerning when it comes to surveillance, according to the doctor.
“It’s abundantly clear we have a serious H5N1 problem in the U.S. that isn’t going away anytime soon.”
“Most of our testing for H5N1 in farm settings to date has only occurred due to clinical outbreaks,” he said.
“If the virus is causing subclinical (mild illness) or asymptomatic (no illness) infections in other livestock, then we may not catch it without regular ongoing testing.”
Factors that mitigate risk
Samuel Scarpino, director of AI and life sciences and professor of health sciences at Northeastern University in Boston, said there are two factors that could potentially mitigate the risk associated with this pig becoming infected with bird flu.
“First, the H5N1 virus that infected the pig in Oregon likely came from an infected bird, as opposed to a spillover from an infected dairy farm,” he told Fox News Digital.

There are two main lineages of H5N1 currently circulating in the US, one in birds and one in dairy cows, an expert noted. (iStock)
“There are two main lineages of H5N1 currently circulating in the US, one in birds and one in dairy cows. We suspect that the H5N1 lineage circulating in dairy cows may be more infectious in humans than the lineage of H5N1 circulating in birds.”
Second, the farm was not large, Scarpino noted, which means there are fewer opportunities for transmission between pigs and for evolution of the virus.
“In addition, there are fewer humans working on the farm who may have come in contact with infected animals,” he added.

Because the farm was not large, there are fewer opportunities for transmission between pigs and for evolution of the virus, said an infectious diseases expert. (AP Photo/Vadim Ghirda, File)
Despite these factors, the expert went on, anytime there are pigs infected with a highly pathogenic avian influenza, measures should be taken to ensure that farm workers are protected and that they have not transmitted the virus to others.
“Even though this virus did not originate from an infected dairy farm, it’s abundantly clear we have a serious H5N1 problem in the U.S. that isn’t going away anytime soon,” Scarpino cautioned.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“We are also entering the normal seasonal flu period, which will make it harder to detect rare H5N1 infections.”
For more Health articles, visit www.foxnews.com/health
Scarpino calls for the Centers for Disease Control and Prevention (CDC), along with state and local public health agencies, to increase resources for influenza surveillance to include both clinical and wastewater testing.
Health
Tuberculosis has overtaken COVID as world's deadliest infectious disease

Tuberculosis (TB) is once again the infectious disease responsible for the most deaths worldwide, according to a Tuesday announcement from the World Health Organization (WHO).
The contagious disease was responsible for 1.25 million global deaths in 2023, WHO reported, including 161,000 people with HIV.
COVID-19 had overtaken TB as the world’s leading infectious killer for the previous three years.
LASSA FEVER DEATH REPORTED IN MIDWESTERN STATE, CONTACT TRACING BEGINS
What to know about tuberculosis
TB is a preventable and curable disease caused by bacteria that typically impacts the lungs, according to WHO.
This 2006 electron microscope image provided by the Centers for Disease Control and Prevention shows Mycobacterium tuberculosis bacteria, which causes the disease tuberculosis. (Janice Carr/CDC/AP)
It is an airborne contagion that can be spread through coughing, sneezing or saliva.
While around 25% of people have likely been infected with the bacteria, only 5% to 10% will experience symptoms and develop the disease, the same source stated.
Only people with symptoms can spread the disease.
Who is at risk?
“If you breathe, you can catch TB — so all people are at risk,” Masae Kawamura, M.D., a former TB control director in San Francisco and a tuberculosis clinician, told Fox News Digital.
Kawamura calls TB a “social disease of crowding and mobility.”
E. COLI OUTBREAK LINKED TO MCDONALD’S BURGERS: HOW TO SPOT THE SYMPTOMS
“Since TB is airborne, congregate settings like hospitals, nursing homes, prisons, jails, classrooms and homeless shelters are places TB is more easily spread, especially if multiple risks are involved,” she said.
Those at the highest risk of developing TB disease after exposure include people who have diabetes, have weakened immunity, are malnourished, use tobacco and/or drink excess amounts of alcohol.
Babies and children are also at higher risk.
“If a person has latent TB infection, TB disease activation varies from 5% to 15% over a lifetime, but can be higher if a person has multiple risks, such being an elderly person and/or being malnourished, having diabetes and/or having other diseases that weaken the immune system,” said Kawamura.
Symptoms, diagnosis and treatment
Those who get sick with TB may experience mild symptoms, including coughing, chest pain, fatigue, weight loss, weakness, fever and night sweats, according to WHO.
Symptoms will vary depending on which organs are affected.
“If you breathe, you can catch TB — so all people are at risk.”
In addition to the lungs, the disease can also affect the kidneys, spine, skin and brain.
“TB can affect any organ of the body, but it causes disease in the lung in over 80% of cases,” said Kawamura.
“This is dangerous because it causes cough, the mechanism of airborne spread.”

TB is an airborne contagion that can be spread through coughing, sneezing or saliva. (iStock)
In more severe cases, patients may cough up blood, noted Kawamura, who serves on the board of directors of Vital Strategies, a global public health organization.
“Often there are minimal symptoms for a long time and people mistake their occasional cough with allergies, smoking or a cold they can’t shake off,” she added.
TB can be identified with rapid diagnostic tests, WHO noted.
The disease is treated with antibiotics that are taken every day for four to six months, the same source stated. Some of the most common include isoniazid, rifampicin, pyrazinamide and ethambutol.

“TB can affect any organ of the body, but it causes disease in the lung in over 80% of cases,” an expert said. “This is dangerous because it causes cough, the mechanism of airborne spread.” (iStock)
Failing to take the complete course of medications can cause the bacteria to become drug-resistant.
Cases of drug-resistant TB need to be treated with different medications.
When TB becomes deadly
If TB goes untreated, it is fatal in about half of its victims, according to Kawamura.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“About 25% recover on their own and another 25% persist as chronic active TB cases,” she said.
In the U.S., most active TB cases are detected at an earlier stage, the expert noted, but the death rate is still “shockingly high” at 10%, and much higher if the patient is over 65 years old.
Prevention of the disease
There is a childhood vaccine called BCG (Bacille-Calmette-Guerin) that is given in most of the world to infants, Kawamura noted.
“It reduces death, meningitis and organ dissemination by 75% in children under 5 — however, it does not prevent TB infection and is ineffective in adults,” the doctor told Fox News Digital.

The best means of prevention is testing those at risk and treating latent tuberculosis infection (LTBI), a doctor advised. (iStock)
“Overall, BCG is considered ineffective, hence, TB’s title as the greatest infectious disease killer of all time.”
BCG was never used in the U.S. because of the country’s lower rates of TB, its ineffectiveness and its interference with TB tests, she added.
For more Health articles, visit www.foxnews.com/health
The best means of prevention is testing those at risk and treating latent tuberculosis infection (LTBI), according to the doctor.
-

 Movie Reviews1 week ago
Movie Reviews1 week agoAlien Country (2024) – Movie Review
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25431700/STK201_SAM_ALTMAN_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25431700/STK201_SAM_ALTMAN_CVIRGINIA_A.jpg) Technology7 days ago
Technology7 days agoOpenAI plans to release its next big AI model by December
-

 Health6 days ago
Health6 days agoNew cervical cancer treatment approach could reduce risk of death by 40%, trial results show
-

 Culture7 days ago
Culture7 days agoTop 45 MLB free agents for 2024-25 with contract predictions, team fits: Will Soto get $600M+?
-

 Sports6 days ago
Sports6 days agoFreddie Freeman's walk-off grand slam gives Dodgers Game 1 World Series win vs. Yankees
-
News5 days ago
Sikh separatist, targeted once for assassination, says India still trying to kill him
-

 Culture5 days ago
Culture5 days agoFreddie Freeman wallops his way into World Series history with walk-off slam that’ll float forever
-

 Technology4 days ago
Technology4 days agoWhen a Facebook friend request turns into a hacker’s trap