Science
A California panel is holding up studies on psychedelics. Some researchers want it gone

At the Pacific Neuroscience Institute in Santa Monica, scientists are eager to explore whether a psychedelic chemical found in a toad could help people whose depression has not eased with typical treatments. Patients regularly call or send emails about joining clinical trials to test that and other compounds, but the research center is turning them away.
“We have to tell them we don’t have any studies enrolling right now,” said Dr. Keith Heinzerling, director of the institute’s TRIP Center, which focuses on treatment and research on psychedelics. “We’ve been put on hold by the state.”
Across the state, dozens of such studies are in limbo thanks to a little-known government panel that monitors research on federally restricted drugs and addiction treatment.
The holdup, tied to a state law requiring government meetings to be held in public, has dragged on since the fall and galvanized some scientists to push for the panel to be dissolved.
Lawmakers in Sacramento established the Research Advisory Panel of California more than half a century ago to vet studies involving cannabis, hallucinogens and treatments for “abuse of controlled substances,” according to the state’s health and safety code.
The panel, which includes representatives of state agencies and universities, has the power to reject studies if they are poorly conceived, would produce little of scientific value, or would expose Californians who sign on as research subjects to excessive risk. It also monitors ongoing research and can revoke its approval if studies veer from what it approved.
Getting the panel’s blessing is a crucial hurdle for researchers working in the state to find better ways to treat drug addiction, a crisis leading to more than 100,000 overdose deaths across the country each year. The panel also has oversight over research in the burgeoning field of psychedelics, which is developing potential treatments for depression, substance use disorder and other conditions.
The panel typically meets every other month, but gatherings scheduled for October and December were canceled with little explanation. Scientists waiting for the go-ahead to launch their studies say they’ve received no information about when meetings will resume.
Among those frustrated by the standstill is David, a 50-year-old grappling with post-traumatic stress disorder. The Los Angeles resident, who asked not to be identified by his full name to protect his medical privacy, reached out to the Pacific Neuroscience Institute to ask about upcoming clinical trials.
“I’ve been in search of a treatment that will alleviate symptoms of PTSD for a long time,” David said. Some existing treatments “have worked pretty well, but there are still times where there’s challenges and episodes that can be pretty destabilizing,” including prolonged bouts of insomnia.
Researchers use a quiet room to test psilocybin therapy at the Pacific Neuroscience Institute in Santa Monica.
(Genaro Molina / Los Angeles Times)
The potential of a psychedelic compound like psilocybin is appealing, but since he’s in recovery for alcohol use, David wants to try it only if it’s administered by medical professionals in a therapeutic environment. The Santa Monica center told him their next possible trial was being held up indefinitely.
“It just seems like the gears of bureaucracy conspire against meaningful solutions,” he said.
At UC San Francisco, Dr. Josh Woolley said two of his planned studies on psilocybin are on indefinite hold. One of them is for young adults with anorexia, a disorder that can significantly ramp up the risk of death if left untreated. Now “we don’t know when it will be approved,” said Woolley, director of the Translational Psychedelic Research Program at UCSF.
The holdup has also interrupted plans for Dr. Charles Grob, a psychiatrist doing research with the Lundquist Institute at Harbor-UCLA Medical Center to examine whether psilocybin could help patients suffering from existential anxiety and demoralization near the end of life.
“Just when things are ready to take off with more research, the field is frozen,” Grob said.
Just when things are ready to take off with more research, the field is frozen.
— Dr. Charles Grob, a psychiatrist with the Lundquist Institute at Harbor-UCLA Medical Center
Several current or former members of the panel declined to comment or did not respond to messages. Dr. Tanveer Khan, the panel’s executive officer, referred questions to the California attorney general’s office.
In a statement, the office said the panel was created to ensure that research involving addiction or certain controlled substances is tracked by the state and proceeds safely in line with “best medical practices and California law.” It attributed the interruption in its meetings to concerns about how a state law requiring public meetings might apply to the panel, but declined to clarify whether those concerns were prompted by recent changes to the Bagley-Keene Open Meetings Act or a new interpretation of existing rules.
Before it stopped meeting altogether, the Research Advisory Panel routinely convened behind closed doors. Scientists argued that meeting in public would be a nonstarter with funders who wanted to protect their intellectual property.
“Realistically, the pharmaceutical companies are not going to allow their stuff to be reviewed in public, unless there’s a very well-thought-out process that protects their interests,” Heinzerling said.
The backlog of studies awaiting review and approval has ballooned since the panel last met in August. By December, 33 new proposals were on ice, as were 13 amendments to existing research projects, according to the attorney general’s office.
The attorney general’s office said it was working with lawmakers and the governor’s office on a legislative solution to resolve the problem but declined to give specifics.
The impasse, first reported in the newsletter Psychedelic Alpha, has deepened longtime frustrations among scientists who argue that even when the panel is meeting normally, it is an outdated and unnecessary entity that slows down vital research.
Dozens of researchers in a newly formed consortium are now calling for the panel to be eliminated. They argue that studies involving controlled substances and addiction treatment are vetted by other oversight boards and that the California panel often rehashes issues that were already decided by other regulators.
Dr. Keith Heinzerling holds a ceramic bowl containing one psilocybin pill that will be used by a study volunteer to try to treat her alcoholism.
(Genaro Molina / Los Angeles Times)
Psychologist Steven Shoptaw, director of the Center for Behavioral and Addiction Medicine at UCLA, said there was a time when such experiments were conducted on people in jails and other settings who could not freely consent. But the rigorous scrutiny from institutional review boards, the Food and Drug Administration, the National Institutes of Health and others now makes the California panel obsolete, he said.
“I’ve never understood why this was not dismantled decades ago,” said Shoptaw, who has studied possible treatments for people who use methamphetamine.
Stanford University clinical psychologist Keith Humphreys said he was asked to join the panel years ago by then-Gov. Jerry Brown, but he declined “because I could see no purpose to it.”
“I just thought, ‘We have an FDA. We have an NIH. Why is the state doing this?’” Humphreys said.
We have an FDA. We have an NIH. Why is the state doing this?
— Stanford clinical psychologist Keith Humphreys
Even without hiccups, undergoing the state review can delay a study for upward of five months, researchers complained. That means wasting $100,000 or more on “unnecessary staff expenditures” during that time, they argued in a letter sent Thursday to Gov. Gavin Newsom and other decision makers.
Such delays can also shut Californians out of multi-state trials of emerging treatments, scientists argue. The lag time now looms larger as medication studies are expected to be run more quickly — within as little as a year instead of five, they said.
“If you’re competing against other states where they don’t have this delay, the industry is going other places,” said Woolley of UC San Francisco.
Dr. Phillip Coffin, director of the Center on Substance Use and Health at the San Francisco Department of Public Health, wanted to join a federally funded study on whether ketamine could help people struggling with methamphetamine addiction. But he said his site and others in California were excluded because of the panel’s delays.
Losing out on the ketamine study and other research opportunities means that “I won’t be able to hire or I will have to let go of staff,” Coffin said.
Compass Pathways, a London biotech firm developing psilocybin treatments, decided not to establish a new “centre of excellence” in San Diego. In an email sent in 2019 to a San Diego researcher, company co-founder George Goldsmith cited the “incredibly slow” state panel as a reason. (A Compass representative reached this week said the company’s clinical trials for depression treatments underway in California had not encountered any delays.)
Many researchers are frustrated that the panel has been reviewing trials for addiction treatment even if they involve ordinary medications. For instance, the panel vetted a study Coffin undertook on mirtazapine — an FDA-approved antidepressant — as a treatment for people who use meth.
In 2022, the panel reviewed 52 new applications plus two submitted the previous year, according to its most recent available annual report. Among those 54 applications, three were either not approved or withdrawn. The reasons weren’t given in the report.
By the end of that year, the panel was monitoring 132 ongoing research projects, including studies on whether cannabis use affects antiretroviral therapy and how psilocybin helps people suffering from phantom limb pain.
Michiel van Elk, who studies altered states of consciousness at Leiden University in the Netherlands, said he wasn’t familiar with the California panel, but could understand the need for a specialized review board because assessing research procedures for psychedelics poses some unique challenges.
“It is really difficult to evaluate the risks of the drug itself, because it always interacts with the mind-set of the person and also with the setting in which it’s administered,” Van Elk said. In general, “our current system is not set up for dealing with those type of challenges.”
Not all researchers who interact with the panel are joining the calls to eliminate it. Grob said going through the panel is “extra work, but it’s been positive,” praising its members as astute and helpful.
“California has this extra layer of regulatory oversight, but the problem is not the committee itself,” he said. “It’s that the committee is unable to do its job.”

Science
Diablo Canyon clears last California permit hurdle to keep running

Central Coast Water authorities approved waste discharge permits for Diablo Canyon nuclear plant Thursday, making it nearly certain it will remain running through 2030, and potentially through 2045.
The Pacific Gas & Electric-owned plant was originally supposed to shut down in 2025, but lawmakers extended that deadline by five years in 2022, fearing power shortages if a plant that provides about 9 percent the state’s electricity were to shut off.
In December, Diablo Canyon received a key permit from the California Coastal Commission through an agreement that involved PG&E giving up about 12,000 acres of nearby land for conservation in exchange for the loss of marine life caused by the plant’s operations.
Today’s 6-0 vote by the Central Coast Regional Water Board approved PG&E’s plans to limit discharges of pollutants into the water and continue to run its “once-through cooling system.” The cooling technology flushes ocean water through the plant to absorb heat and discharges it, killing what the Coastal Commission estimated to be two billion fish each year.
The board also granted the plant a certification under the Clean Water Act, the last state regulatory hurdle the facility needed to clear before the federal Nuclear Regulatory Commission (NRC) is allowed to renew its permit through 2045.
The new regional water board permit made several changes since the last one was issued in 1990. One was a first-time limit on the chemical tributyltin-10, a toxic, internationally-banned compound added to paint to prevent organisms from growing on ship hulls.
Additional changes stemmed from a 2025 Supreme Court ruling that said if pollutant permits like this one impose specific water quality requirements, they must also specify how to meet them.
The plant’s biggest water quality impact is the heated water it discharges into the ocean, and that part of the permit remains unchanged. Radioactive waste from the plant is regulated not by the state but by the NRC.
California state law only allows the plant to remain open to 2030, but some lawmakers and regulators have already expressed interest in another extension given growing electricity demand and the plant’s role in providing carbon-free power to the grid.
Some board members raised concerns about granting a certification that would allow the NRC to reauthorize the plant’s permits through 2045.
“There’s every reason to think the California entities responsible for making the decision about continuing operation, namely the California [Independent System Operator] and the Energy Commission, all of them are sort of leaning toward continuing to operate this facility,” said boardmember Dominic Roques. “I’d like us to be consistent with state law at least, and imply that we are consistent with ending operation at five years.”
Other board members noted that regulators could revisit the permits in five years or sooner if state and federal laws changes, and the board ultimately approved the permit.
Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
Science
When slowing down can save a life: Training L.A. law enforcement to understand autism
Kate Movius moved among a roomful of Los Angeles County sheriff’s deputies, passing out a pop trivia quiz and paper prism glasses.
She told them to put on the vision-distorting glasses, and to write with their nondominant hand. As they filled out the tests, Movius moved about the City of Industry classroom pounding abruptly on tables. Then came the cowbell. An aide flashed the overhead lights on and off at random. The goal was to help the deputies understand the feeling of sensory overwhelm, which many autistic people experience when incoming stimulation exceeds their capacity to process.
“So what can you do to assist somebody, or de-escalate somebody, or get information from someone who suffers from a sensory disorder?” Movius asked the rattled crowd afterward. “We can minimize sensory input. … That might be the difference between them being able to stay calm and them taking off.”
Movius, founder of the consultancy Autism Interaction Solutions, is one of a growing number of people around the U.S. working to teach law enforcement agencies to recognize autistic behaviors and ensure that encounters between neurodevelopmentally disabled people and law enforcement end safely.
She and City of Industry Mayor Cory Moss later passed out bags filled with tools donated by the city to aid interactions: a pair of noise-damping headphones to decrease auditory input, a whiteboard, a set of communication cards with words and images to point to, fidget toys to calm and distract.
“The thing about autistic behavior when it comes to law enforcement is a lot of it may look suspicious, and a lot of it may feel very disrespectful,” said Movius, who is also the parent of an autistic 25-year-old man. Responding officers, she said, “are not coming in thinking, ‘Could this be a developmentally disabled person?’ I would love for them to have that in the back of their minds.”
A sheriff’s deputy reads a pamphlet on autism during the training program.
(Genaro Molina / Los Angeles Times)
Autism spectrum disorder is a developmental condition that manifests differently in nearly every person who has it. Symptoms cluster around difficulties in communication, social interaction and sensory processing.
An autistic person stopped by police might hold the officer’s gaze intensely or not look at them at all. They may repeat a phrase from a movie, repeat the officer’s question or temporarily lose their ability to speak. They might flee.
All are common involuntary responses for an autistic person in a stressful situation, which a sudden encounter with law enforcement almost invariably is. To someone unfamiliar with the condition, all could be mistaken for intoxication, defiance or guilt.
Autism rates in the U.S. have increased nearly fivefold since the Centers for Disease Control began tracking diagnoses in 2000, a rise experts attribute to broadening diagnostic criteria and better efforts to identify children who have the condition.
The CDC now estimates that 1 in 31 U.S. 8-year-olds is autistic. In California, the rate is closer to 1 in 22 children.
As diverse as the autistic population is, people across the spectrum are more likely to be stopped by law enforcement than neurotypical peers.
About 15% of all people in the U.S. ages 18 to 24 have been stopped by police at some point in their lives, according to federal data. While the government doesn’t track encounters for disabled people specifically, a separate study found that 20% of autistic people ages 21 to 25 have been stopped, often after a report or officer observation of a person behaving unusually.
Some of these encounters have ended in tragedy.
In 2021, Los Angeles County sheriff’s deputies shot and permanently paralyzed a deaf autistic man after family members called 911 for help getting him to a hospital.
Isaias Cervantes, 25, had become distressed about a shopping trip and started pushing his mother, his family’s attorney said at the time. He resisted as two deputies attempted to handcuff him and one of the deputies shot him, according to a county report.
In 2024, Ryan Gainer’s family called 911 for support when the 15-year-old became agitated. Responding San Bernardino County sheriff‘s deputies shot and killed him outside his Apple Valley home.
Last year, police in Pocatello, Idaho, shot Victor Perez, 17, through a chain-link fence after the nonspeaking teenager did not heed their shouted commands. He died from his injuries in April.

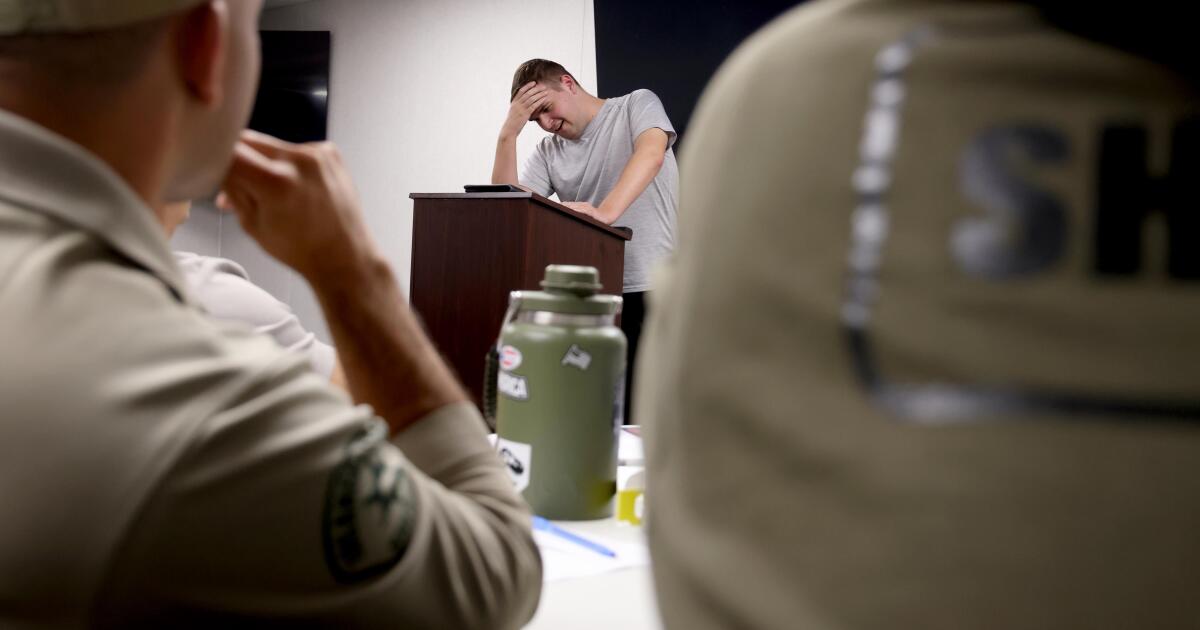
Sheriff’s deputies take a trivia quiz using their non-writing hands, while wearing vision-distorting glasses, as Kate Movius, standing left, and Industry Mayor Cory Moss, right, ring cowbells. The idea was to help them understand the sensory overwhelm some autistic people experience.
(Genaro Molina / Los Angeles Times)
As early as 2001, the FBI published a bulletin on police officers’ need to adjust their approach when interacting with autistic people.
“Officers should not interpret an autistic individual’s failure to respond to orders or questions as a lack of cooperation or as a reason for increased force,” the bulletin stated. “They also need to recognize that individuals with autism often confess to crimes that they did not commit or may respond to the last choice in a sequence presented in a question.”
But a review of multiple studies last year by Chapman University researchers found that while up to 60% of officers have been on a call involving an autistic person, only 5% to 40% had received any training on autism.
In response, universities, nonprofits and private consultants across the U.S. have developed curricula for law enforcement on how to recognize autistic behaviors and adapt accordingly.
The primary goal, Movius told deputies at November’s training session, is to slow interactions down to the greatest extent possible. Many autistic people require additional time to process auditory input and verbal responses, particularly in unfamiliar circumstances.
If at all possible, Movius said, wait 20 seconds for a response after asking a question. It may feel unnaturally long, she acknowledged. But every additional question or instruction fired in that time — what’s your name? Did you hear me? Look at me. What’s your name? — just decreases the likelihood that a person struggling to process will be able to respond at all.
Moss’ son, Brayden, then 17, was one of several teenagers and young adults with autism who spoke or wrote statements to be read to the deputies. The diversity of their speech patterns and physical mannerisms showed the breadth of the spectrum. Some were fluently verbal, while others communicated through signs and notes.
“This population is so diverse. It is so complicated. But if there’s anything that we can show [deputies] in here that will make them stop and think, ‘Hey, what if this is autism?’ … it is saving lives,” Moss said.

Mayor Cory Moss, left, and Kate Movius hug at the end of the training program last November. Movius started Autism Interaction Solutions after her son was born with profound autism.
(Genaro Molina / Los Angeles Times)
Some disability advocates cautioned that it takes more than isolated training sessions to ensure encounters end safely.
Judy Mark, co-founder and president of the nonprofit Disability Voices United, says she trained thousands of officers on safe autism interactions but stopped after Cervantes’ shooting. She now urges families concerned about an autistic child’s safety to call an ambulance rather than law enforcement.
“I have significant concern about these training sessions,” Mark said. “People get comfort from it, and the Sheriff’s Department can check the box.”
While not a panacea, supporters argue that a brief course is better than no preparation at all. Some years ago, Movius received a letter from a man whose profoundly autistic son slipped away as the family loaded their car at the beach. He opened the unlocked door of a police vehicle, climbed into the back and began to flail in distress.
Though surprised, the officer seated at the wheel de-escalated the situation and helped the young man find his family, the father wrote to Movius. He had just been to her training.
-

 World1 day ago
World1 day agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts2 days ago
Massachusetts2 days agoMother and daughter injured in Taunton house explosion
-

 Montana1 week ago
Montana1 week ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Oklahoma1 week ago
Oklahoma1 week agoWildfires rage in Oklahoma as thousands urged to evacuate a small city
-

 Louisiana4 days ago
Louisiana4 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Technology6 days ago
Technology6 days agoYouTube TV billing scam emails are hitting inboxes
-

 Denver, CO2 days ago
Denver, CO2 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Technology6 days ago
Technology6 days agoStellantis is in a crisis of its own making


















