Health
Surprising sleep trends revealed in new survey, including the rise of ‘Scandinavian sleeping’

More than 20% of American adults say they “rarely or never” wake up feeling well-rested, according to a new survey from U.S. News & World Report.
Nearly half (43%) of survey respondents said they have experienced insomnia in 2023, and 17% said they’ve suffered from sleep apnea.
The survey, which polled 1,200 adults about their sleep habits and quality, revealed some of the biggest sources of sleep struggles.
LACK OF SLEEP IS COMPROMISING THE MENTAL HEALTH OF 78% OF ADULTS, SURVEY FINDS
Here’s the state of slumber.
What’s keeping people up at night
One in three adult respondents said they do not sleep in the same bed as their partners due to differing sleep preferences, a trend known as “sleep divorce.” (iStock)
The survey identified the biggest concerns that are hindering Americans’ sleep:
- The increase in cost of living
- The COVID-19 pandemic
- Gun violence
- Climate change
- The 2024 presidential election
These results were virtually identical to last year, except for No. 5, which was the Russia-Ukraine war.
(The survey was conducted before the onset of the Israel-Hamas war.)
WWII-ERA MILITARY SLEEP METHOD COULD HELP INSOMNIACS NOD OFF QUICKLY, SOME CLAIM: ‘PEACE AND CALM’
“In addition to these general worries, there are also specific concerns that may keep Americans up at night depending on their individual circumstances, such as relationship problems or work stress,” Dr. Shelby Harris, the New York-based director of sleep health at Sleepopolis, who was not involved in the survey, told Fox News Digital.
Americans’ worst sleep habits

A previous poll by the National Sleep Foundation found that 89% of adults and 75% of children have at least one electronic device in their bedrooms. (iStock)
Survey respondents shared these top five habits that are detrimental to their sleep:
- Going to bed at inconsistent times
- Accessing screens in bed
- Eating too much before bed
- Falling asleep with the television on
- Staying up all night
A previous poll by the National Sleep Foundation found that 89% of adults and 75% of children have at least one electronic device in their bedrooms.
“By allowing each partner to regulate their own temperature and choose bedding that meets their personal preferences and needs, the method can significantly reduce sleep disruptions and improve comfort.”
“Other common sleep habits that can negatively affect sleep quality include consuming caffeine or alcohol close to bed, napping for too long or too late in the day, not getting enough sunlight in the morning/afternoon, sleeping in a hot or uncomfortable environment and not having a relaxing bedtime routine,” said Harris of Sleepopolis.
Impact of partners on sleep
One in three adult respondents said they do not sleep in the same bed as their partners due to differing sleep preferences, a trend known as “sleep divorce.”

With the Scandinavian sleep method, “both you and your partner can each have your own individual, preferred sleep space in the same bed,” a sleep expert told Fox News Digital. “No more tugging at the sheets or dealing with a blanket hog.” (iStock)
Dr. Brandy Smith, an Alabama-based psychologist with the virtual health care company Thriveworks, who was not involved in the survey, previously told Fox News Digital that the most common reasons for sleep divorce include snoring, frequent movements that keep one partner awake or wake them too often throughout the sleep cycle, mismatched sleep/wake cycles — and schedule differences.
‘SLEEP DIVORCE’: WHY ARE SOME COUPLES SPENDING THEIR NIGHTS IN SEPARATE BEDS?
Another sleep trend revealed in the survey is “Scandinavian sleeping.”
This is when couples share the same bed but use individual comforters or duvets instead of sharing bedding.
“While most surveyed U.S. adults (59%) prefer sharing a comforter with their partner at night, the remainder (41%) would rather sleep with their own blanket at night, which is commonly referred to as the Scandinavian sleeping method,” Haniya Rae, a New York-based sleep feature editor at U.S. News & World Report, told Fox News Digital.

Nearly half (43%) of survey respondents said they have experienced insomnia in 2023. (iStock)
“The Danes, Icelanders, etc. prefer sleeping with their own duvet with no top sheet to fight over,” she noted.
“This means both you and your partner can each have your own individual, preferred sleep space in the same bed. No more tugging at the sheets or dealing with a blanket hog.”
6 SIGNS YOUR MATTRESS MIGHT BE DISRUPTING YOUR SLEEP, ACCORDING TO EXPERTS
Harris agreed that the Scandinavian sleep method can have several potential benefits for sleep quality and overall well-being.

In the survey, a high-quality mattress was rated as the most critical for quality sleep, followed by memory foam pillows, high-thread-count sheets and a down comforter. (iStock)
“By allowing each partner to regulate their own temperature and choose bedding that meets their personal preferences and needs, the method can significantly reduce sleep disruptions and improve comfort,” she told Fox News Digital.
“Getting better sleep can also help to reduce stress levels and lead to a healthier relationship.”
Essentials for a good night’s sleep
In the survey, adults were asked to rate which items are most critical for quality sleep. In order from most to least important, they noted the following:
- High-quality mattress
- Memory foam pillows
- High thread-count sheets
- Down comforter
- Weighted blanket
Nearly 40% of respondents also said they use white noise to help them fall asleep.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The National Sleep Foundation recommends that adults between 18 and 64 years of age get seven to nine hours of sleep each night.
For more Health articles, visit www.foxnews.com/health.

Health
C.D.C. Cuts Threaten to Set Back the Nation’s Health, Critics Say

The extensive layoffs of federal health workers that began on Tuesday will greatly curtail the scope and influence of the Centers for Disease Control and Prevention, the world’s premier public health agency, an outcome long sought by conservatives critical of its handling of the Covid-19 pandemic.
The reorganization of the Department of Health and Human Services shrinks the C.D.C. by 2,400 employees, or roughly 18 percent of its work force, and strips away some of its core functions.
Some Democrats in Congress described the reorganization throughout H.H.S. as flatly illegal.
“You cannot decimate and restructure H.H.S. without Congress,” said Senator Patty Murray, Democrat of Washington, and a member of the Senate health committee.
“This is not only unlawful but seriously harmful — they are putting Americans’ health and well-being on the line,” she added.
Ms. Murray noted that the Trump administration had not detailed which units are being cut at the C.D.C. and other health agencies. Robert F. Kennedy Jr., the health secretary, said last week the layoffs would affect primarily administrative functions.
But according to information gathered by The New York Times from dozens of workers, the reductions were more broadly targeted. Scientists focused on environmental health and asthma, injuries, lead poisoning, smoking and climate change were dismissed.
Researchers studying blood disorders, violence prevention and access to vaccines were let go. The agency’s center on H.I.V. and sexually transmitted diseases was among the hardest hit, losing about 27 percent of its staff.
The National Institute for Occupational Safety and Health, which makes recommendations on how to keep workers safe, was all but dissolved.
What remains is a hobbled C.D.C., with a smaller global footprint, devoting fewer resources to environmental health, occupational health and disease prevention, public health experts said.
Instead, the agency will be trained more narrowly on domestic disease outbreaks. Communications will be centralized at H.H.S. in Washington.
The department intends “to ensure a more coordinated and effective response to public health challenges, ultimately benefiting the American taxpayer,” said Emily Hilliard, deputy press secretary at the department.
“C.D.C. scientists have conducted numerous interviews on a variety of topics and will continue to do so,” she added.
Critics predicted the move would prevent scientists from speaking frankly about public health.
“American taxpayers provide the resources for C.D.C.’s specialists and have the right to hear directly from them without interference by politicians,” said Dr. Thomas R. Frieden, who led the agency from 2009 to 2017.
The sweeping reductions arrive as the nation confronts an outbreak of measles in Texas and elsewhere, a spreading bird flu epidemic on poultry and dairy farms, and a raft of new questions about public health measures like water fluoridation and school vaccine requirements.
“What we seem to be seeing is a dismantling rather than a restructuring” of the public health system, said Dr. Richard Besser, chief executive of the Robert Wood Johnson Foundation and a former acting director of the C.D.C.
On Capitol Hill, the Senate health committee, which recommended confirmation of Mr. Kennedy as secretary, scheduled a hearing on the reorganization of H.H.S., citing the possible impacts on public health.
Mr. Kennedy has described the reorganization as an effort to clean up waste and bureaucracy while promising that federal health agencies would do more to improve the health of Americans.
“We’re going to eliminate an entire alphabet soup of departments and agencies while preserving their core functions by merging them into a new organization called the Administration for a Healthy America,” the secretary said in a videotaped message announcing the layoffs.
The department did not respond to requests for more detailed information.
Society’s most vulnerable — the poor, Black, Latino and Native American people, rural Americans with less access to health care, the disabled and those at highest risk for illness — are likely to be hit hardest, experts said.
“These communities rely on public health to a larger extent than wealthy communities do,” Dr. Besser said.
For decades, public health and medical research drew support across the political spectrum.
But the C.D.C. has been in the political cross hairs since the first Trump administration, when the White House muzzled the agency’s communications, meddled with its publications and blamed its scientists for bungling the pandemic response.
In recent years, lawmakers have harshly criticized the agency’s advice on masks, lockdowns, social distancing, school closures and various other attempts to contain the pandemic, calling them economically and socially disastrous.
Project 2025, the conservative blueprint for reshaping the federal government, described the C.D.C. as “perhaps the most incompetent and arrogant” federal agency, and called on Congress to curb its powers.
Through staffing cuts, the administration reduced critical divisions of the National Center for Injury Prevention and Control, and employees studying how to prevent gun violence, child abuse and elder abuse were fired.
Injuries are the leading cause of death among Americans under 45. About 47,000 Americans are killed by firearms each year, more than half of them suicides.
But gun violence is a politically fraught topic. Pressure from the National Rifle Association and conservative politicians led to a ban on using federal funds to study gun violence for almost 25 years. Funding was restored in 2019.
The injury center studied ways to improve gun safety and promoted the use of gun locks, particularly in homes where children live.
“People think of gun violence as a question for law enforcement, but the public health approach has made a big difference,” said Dr. Mark Rosenberg, a former center director.
Most of the C.D.C.’s Division of Reproductive Health, which studies maternal health, was also shuttered. Whether some or all of its portfolio will be assumed by the new organization created by Mr. Kennedy was not clear.
Pregnant women and newborns die in the United States at a far higher rate than in other industrialized nations.
In recent years, the C.D.C. focused on stark racial health disparities that put Black American women at nearly three times the risk of dying of pregnancy complications than white women.
But the Trump administration has been defunding studies of health disparities in racial, ethnic and gender minorities, saying they do not align with the president’s executive orders ending diversity, equity and inclusion initiatives.
Mr. Kennedy said last week that the National Institute for Occupational Safety and Health, which makes recommendations for preventing work-related injuries and illnesses, would be absorbed into the health department.
But on Tuesday, most of its divisions were eliminated, among them offices dedicated to protecting workers in various industries, including mine inspectors.
Even one of the agency’s most essential functions, infectious disease research, was affected.
The Trump administration had been weighing moving the H.I.V. prevention division to a different agency within the health department.
But on Tuesday, teams leading H.I.V. surveillance and research within that division were laid off. It was unclear whether some of those functions would be recreated elsewhere. (A team in the global health center working on preventing mother-to-child transmission of H.I.V. was also cut.)
Until now, the C.D.C. provided funds to states and territories for responding to and preventing H.I.V. outbreaks. Roughly one in four new diagnoses of H.I.V. is made with agency funds.
Some H.I.V. experts warned that the move could lead to a rise in H.I.V. infections among Americans.
“H.I.V. prevention is a lot more than just giving out condoms,” said Dr. John Brooks, who served as chief medical officer for the division of H.I.V. prevention until last year. “It saves lives, averts illness and produces enormous cost savings.”
Broadly, the reorganization aligns with Mr. Kennedy’s preferred emphasis on research into chronic diseases; federal research has been far too focused on infectious diseases, he has said.
But the line between them is not always clear, said Dr. Anne Schuchat, former principal deputy director of the C.D.C. Research that seems disconnected from outbreak response may also be a key for fighting pathogens.
“For Zika, we needed experts in birth defects, entomology and vector control, virologists and environmental health experts,” she said. “Emerging threats don’t respect borders of C.D.C. organizational units.”
The reorganization risks choking the talent pipeline for public health, said Ursula Bauer, former director of the agency’s National Center for Chronic Disease Prevention and Health Promotion.
“Once you decimate an agency like C.D.C., which is full of high-caliber highly trained individuals, building back is going to be incredibly difficult,” she said.
“It will take two to three times as long to undo the damage as it took to inflict it.”
The cuts also will take a toll on the agency’s ability to gather and analyze data, which are keys to identifying trends and developing interventions, Dr. Phil Huang, director of Dallas County Health and Human Services, said at a news briefing.
“You take away those systems, and it takes away the ability to see the impact of all these cuts,” he added.
Health
Death probe of ex-Yankee's son triggers carbon monoxide warnings from experts

Experts are speaking out about the potential dangers attached to carbon monoxide, as authorities continue to probe the death of teen Miller Gardner, son of former New York Yankees player Brett Gardner.
While the cause of Miller Gardner’s death remains unconfirmed, Costa Rican Judicial Investigative Agency (OIJ) General Director Randall Zúñiga told reporters at a press conference on Monday that high levels of carbon monoxide contamination were found in the Gardner family’s hotel room, and that it might have caused the teen’s death.
“Which then leads us towards a line of investigation in which it seems that this person could have died from inhaling these very dangerous gases,” Zúñiga said.
Zúñiga said investigators who work on a specialized dangerous atmospheres team detected “high emissions of pollution of…carbon monoxide” in the room at Costa Rica’s Arenas Del Mar Beachfront & Rainforest Resort, which is where the Gardners were staying.
Officials at the hotel are denying the carbon monoxide claims.
DEATH OF EX-YANKEE’S SON IN COSTA RICA HAS EXPERTS SOUNDING ALARM ON HEALTHY TRAVEL
“The levels in the hotel room were non-existent and non-lethal. There was an error in this initial reporting. As mentioned, we await for conclusive results to confirm the cause of this unfortunate death,” a hotel spokesperson told Fox News Digital.
The spokesperson also said the room has been “closed off out of an abundance of precaution.”
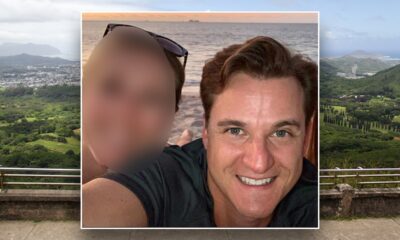
Miller Gardner, 14, is photographed with his father, Brett Gardner, a former New York Yankee. Miller Gardner died last month in Costa Rica. His death is currently being investigated. (Courtesy of New York Yankees)
Dr. Nicole Saphier, a Fox News medical contributor, said no parent should ever have to endure the tragedy of losing a child.
In regard to carbon monoxide, she said the gas is “a silent, deadly threat.”
“We often focus on smoke alarms, but carbon monoxide is colorless, odorless and can overcome a person before they even realize what’s happening,” Saphier told Fox News Digital.
Saphier said every household should have multiple functioning carbon monoxide detectors, especially near sleeping areas.
For more Health articles, visit www.foxnews.com/health
“When we travel — whether staying at a hotel, Airbnb, or even in an RV — it’s worth considering bringing a portable carbon monoxide monitor for added protection,” she suggested.

The death of Miller Gardner, son of former New York Yankee Brett Gardner, has experts speaking out about carbon monoxide after the teen died while on vacation in Costa Rica. (AP Photo/Seth Wenig)
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Health and a Fox News senior medical analyst, said, “symptoms can come on rapidly within minutes or hours and can include headache, nausea, fatigue, dizziness and vomiting.”
If you experience symptoms that you think could be from carbon monoxide poisoning, the Environmental Protection Agency recommends opening doors and windows, turning off combustion appliances and leaving the building.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Siegel said prompt treatment with oxygen can sometimes reverse carbon monoxide poisoning.
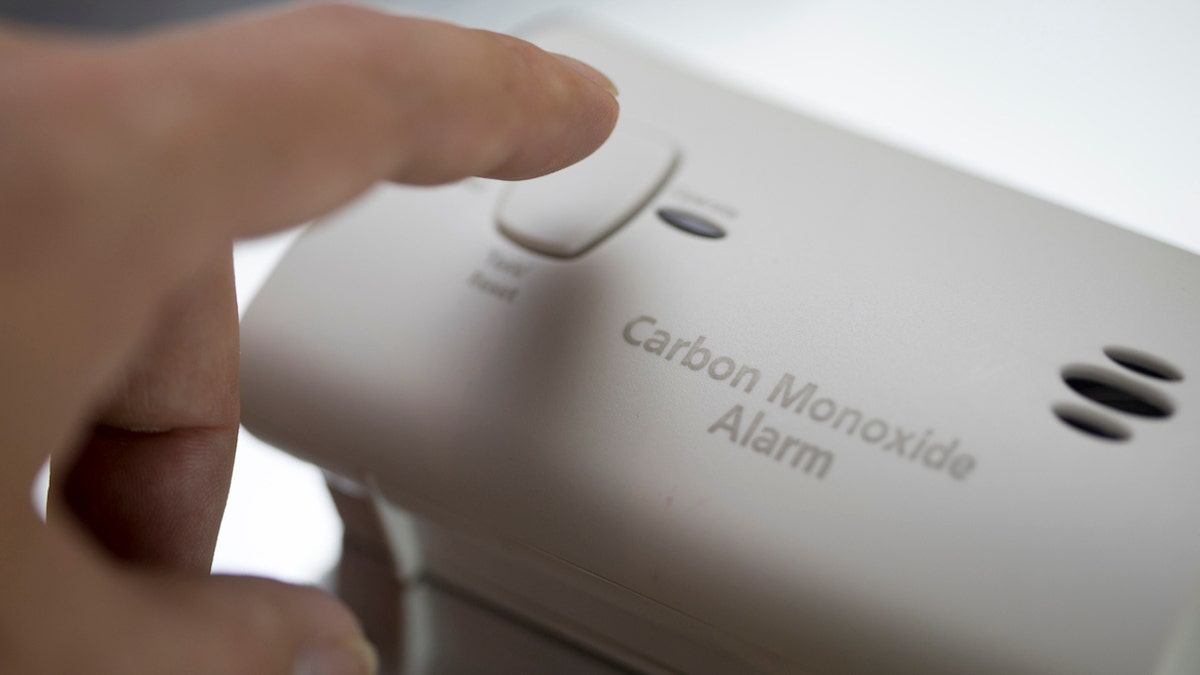
Between 2009 and 2019, deaths from non-fire-related carbon monoxide poisoning have been on the rise, according to a new report released by the CPSC. (iStock)
“It is absolutely shocking to me that it took this long to be disclosed as a likely cause of death, when they could have done a test for carbon monoxide in [Miller Gardener’s] blood within hours during his autopsy weeks ago,” Siegel told Fox News Digital.
Between 2009 and 2019, deaths from non-fire-related carbon monoxide poisoning were on the rise, according to a report released by the U.S. Consumer Product Safety Commission (CPSC) in March 2023.
Fox News Digital reached out to OIJ in Costa Rica for additional comment.
Health
Federal Health Workers Make Up Less Than 1% of Agency Spending

A few days ago, Robert F. Kennedy Jr., the health secretary, embarked on a media tour to defend his decision to lay off thousands of his department’s workers.
He announced a plan last week to cut 10,000 jobs, in addition to the estimated 10,000 jobs cut through retirements and buyouts in the early weeks of the Trump administration.
Mr. Kennedy had called the Health and Human Services Department “the biggest agency in government, twice the size of the Pentagon, $1.9 trillion dollars,” during an interview with NewsNation. He went on to suggest that the department was doing little to improve the health of Americans, “with all the money that was being thrown at it, with all the personnel that were being brought in.”
H.H.S. does spend more than the Department of Defense, which has a discretionary budget of about $850 billion. But according to several budget experts, the overwhelming majority of the H.H.S. department’s $1.8 trillion budget is not spent on its staff.
Spending on personnel at the federal health agencies accounts for a small fraction of its budget — less than 1 percent, according to three budget experts. That includes the staff of the Food and Drug Administration, the Centers for Disease Control and Prevention, the National Institutes of Health and others.
The overwhelming majority of the money is spent through Medicare, for the health care of people older than 65, or through Medicaid, for people with low incomes. Those funds filter out to hospitals, clinics, nursing homes, dialysis centers, pharmaceutical companies, medical device makers and Medicare Advantage private insurance plans.
Melinda Buntin, professor of health policy and economics at Johns Hopkins University, said the $17.6 billion in costs for H.H.S. employees made up less than 1 percent of the department’s budget, and has risen in line with overall spending.
“I think that most people would be surprised by what a small share of Health and Human Services spending is for personnel, both their wages and compensation and benefits,” she said, noting that it made sense in the context of the agency’s spending on care.
Bobby Kogan, senior director of federal budget policy at the Center for American Progress, a left-leaning think tank, said Mr. Kennedy’s framing was “incredibly misleading.”
“It would leave someone with a super wrong understanding of what is going on really,” Mr. Kogan said. “The only story of what’s going on in H.H.S. is that we have a huge increase in the elderly population.”
An H.H.S. spokesman said the work force reductions are meant to cut $1.8 billion a year in federal spending, and that the amount is significant.
The Administration for Children and Families, another agency within H.H.S., also spends billions of dollars on services to the public. It operates Head Start programs, foster care, Temporary Assistance for Needy Families, formerly known as welfare, and care homes for unaccompanied minors from other countries.
Chris Towner, policy director for the Committee for a Responsible Federal Budget, made his own calculation, also concluding that H.H.S. staff costs appeared to be shy of 1 percent of the department’s spending. The figure could be slightly higher, he said, given the number of health agency workers with advanced degrees.
So far, the Trump administration has talked about fraud in the federal government repeatedly — though not the type that’s long been a target in Congress. Lawmakers have repeatedly raised the idea of reeling in Medicare Advantage insurance plans, which were estimated to overcharge Medicare by tens of billions of dollars a year.
-

 News1 week ago
News1 week agoTrump Is Trying to Gain More Power Over Elections. Is His Effort Legal?
-

 News1 week ago
News1 week agoWashington Bends to RFK Jr.’s ‘MAHA’ Agenda on Measles, Baby Formula and French Fries
-

 News1 week ago
News1 week agoCompanies Pull Back From Pride Events as Trump Targets D.E.I.
-

 World1 week ago
World1 week agoAt least six people killed in Israeli attacks on southern Syria
-

 Technology1 week ago
Technology1 week agoTrump officials planned a military strike over Signal – with a magazine editor on the line
-

 Technology1 week ago
Technology1 week agoThe FBI launched a task force to investigate Tesla attacks
-

 World1 week ago
World1 week agoNo, Norway and Sweden haven't banned digital transactions
-

 Culture1 week ago
Culture1 week agoAnalysing Jamal Musiala’s bizarre corner goal for Germany against Italy