North Carolina
Boviet Solar Invests $294 Million in North Carolina: First Manufacturing Facility in North America Signals Growth in U.S. Solar Industry

Boviet Solar Technology Co. Ltd., a leading Vietnamese solar energy technology company specializing in monocrystalline PV cells, announces its decision to establish its inaugural production facility in North America, specifically in Greenville, Pitt County, North Carolina. The facility, representing a $294 million investment, is set to create approximately 908 skilled local jobs and bolster the region’s economy.

The company’s move signifies its commitment to the U.S. solar market and aims to meet the growing demand for renewable energy solutions. Boviet Solar’s expansion into North Carolina follows its successful track record of PV cell and module production in Vietnam.

The manufacturing facility will initially focus on producing Boviet Solar’s TOPCon N-Type cell-based Monofacial and Bifacial PV modules for various applications, including residential, commercial, industrial, and utility-scale projects. Phase one of the project will utilize existing infrastructure, while phase two involves constructing a state-of-the-art factory on 34 acres to manufacture PV cells.

Scheduled for completion in Q1 2025, the facility is expected to output 2 GW of solar panels and 2 GW of PV cells annually, significantly contributing to the local clean energy sector.
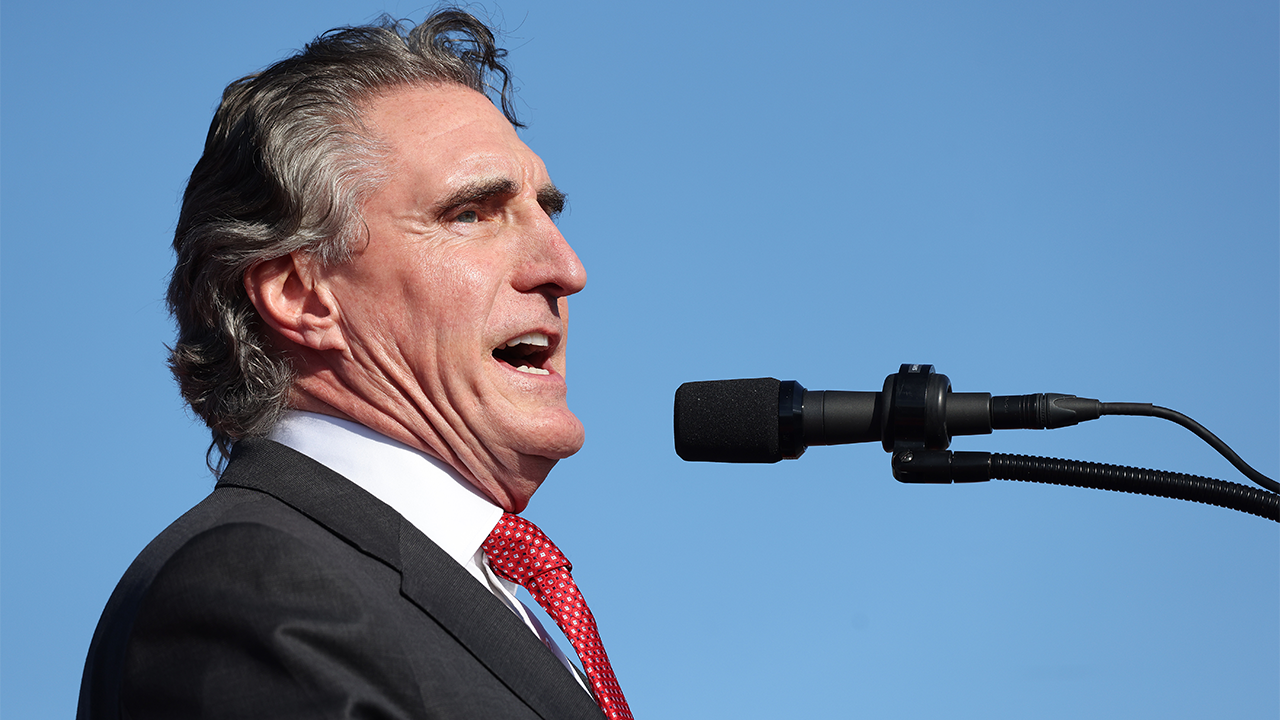
North Carolina Governor Roy Cooper expressed his enthusiasm for welcoming Boviet Solar to the state, highlighting North Carolina’s reputation as a hub for clean energy and its supportive business environment.
Representative Don Davis of North Carolina’s 1st District emphasized the positive impact of Boviet Solar’s investment in the region, noting its contribution to innovation and sustainability efforts.
Greenville Mayor P.J. Connelly echoed the sentiment, underscoring the collaborative efforts that led to attracting Boviet Solar to the community and the significant economic benefits it brings.
Boviet Solar’s decision to establish a manufacturing facility in North Carolina underscores its dedication to providing high-quality, locally-made PV modules and its commitment to sustainability and innovation in the U.S. solar industry.
Related

North Carolina
North Carolina grapples with growing nursing shortage

North Carolina faces an estimated nursing shortage of 12,500 workers by 2033.
One projection by the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill says long-term effects of the pandemic could cause that to jump to 18,600.
Braxton Nowell, UNC Health RN, has experienced the strain of a nursing shortage firsthand.
“One wonderful thing about medicine is people are living longer, healthier lives. However, we also have to have the nurses to take care of them,” he said.
The North Carolina native started working for UNC Health in January of 2020 as a nursing assistant.
“My grandmother is really my main reason for nursing,” Nowell explained. “I saw when she was in the hospital – she’s been hospitalized multiple times throughout my life – I saw the care she was given and how nurses advocated for her. I knew that’s what I wanted to do for people as well.”
He had only been on the job a mere three months before the healthcare system experienced an unprecedented shift in patient care due to a global pandemic.
“This unit was the COVID unit,” Nowell explained while showing WRAL News around the medicine progressive care unit at the Chapel Hill hospital.
Despite widespread burnout with healthcare as COVID cases climbed, Nowell continued his training. He graduated from UNC with a bachelor’s degree in nursing in 2022.
As UNC marks the recent graduation of 113 BSN students and another 70 graduate students from its school of nursing in Chapel Hill, Nowell hopes more students will follow suit to work in the Tar Heel State.
But, he says a lack of program space is a big issue.
“There’s not enough slots for people that want to be nurses. I think at UNC, they have 120 spots and I know they get more than 200 applications,” Nowell explained. “They always can’t give people who I know want to be nurses a slot.”
Kylie Goodman is in the midst of her first year in the accelerated bachelor of science nursing program through UNC.
“Originally I thought I wanted to be a dietitian but growing up I was always really passionate about healthcare,” said Goodman. “I’m very interested in the overall body as a whole and helping people who are sick more in that aspect.”
He and other nursing students take classes in Roper Hall with the School of Medicine while the university’s School of Nursing is demolished. A new building is expected to open in 2026. Officials say it will help the university reach its goal to increase nursing program capacity by 50%.
The UNC Health system currently has about 1,400 openings.
Goodman and dozens of others in the ABSN program are looking to one day fill some of those roles.
“I really do enjoy (pediatrics) but I also like adult,” Goodman shared. “I think trauma sounds interesting.”
When asked why she still wished to pursue a career in medicine in the wake of a global pandemic, Goodman said she just wanted to help people.
“Just to be able to come home from work today and say I know I made a difference in someone’s life,” she said. “Patients are in a stressful environment and they’re vulnerable. I want to be that person to help them in those situations.”
She added, being a student during such a difficult time makes her better equipped to handle a stressful career like nursing.
“I think the ability to adapt is really going to help me in this career and the ability to just take things as they come and adjust to them,” Goodman said.
US News and World Reports ranks Duke’s undergraduate nursing program the best in the country. UNC is ranked No. 4.
Terry McDonnell, senior vice president and chief nurse executive for Duke University Health System, said Duke’s current nurse vacancy rate “is less than 1%.” McDonnell said this is due to the use of “team-based models” used to provide care.
McDonnell added, “Duke nursing care benefits from partnership with the Watts School of Nursing and close collaboration with Duke University School of Nursing, Durham Tech and Wake Tech, as well as by undergoing efforts to reduce administrative burdens on nurses.”
North Carolina
Chris Suttle on SB3 and whether NC could become the 39th state to legalize medical marijuana • NC Newsline

Medical marijuana is now legal and accessible for the vast majority of Americans, but one state that remains a stubborn holdout is North Carolina. A state Senate bill known as the Compassionate Care Act would change that by allowing patients suffering from a list of illnesses to gain access. The bill is sponsored by a conservative Republican and enjoyed bipartisan support when it won Senate approval last year, but right now, House Republicans refuse to take it up.
So, is there a chance the measure will pass during the ongoing short session and what are proponents of the bill doing and saying to try and break the logjam?
NC Newsline caught up with one of the bill’s most outspoken champions, cannabis advocate and consultant, Chris Suttle.
Suttle shares details on a May 24th trip for legislators to North Carolina’s first marijuana dispensary run by the Eastern Band of Cherokee Indians. He believes the guardrails they have put in place may alleviate some concerns that conservative lawmakers have about moving forward with Senate Bill 3.
North Carolina
After the only hospital in town closed, a North Carolina city directs its ire at politicians

By Amanda Seitz and Allen G. Breed | Associated Press
WILLIAMSTON, N.C. — Weeds have punctured through the vacant parking lot of Martin General Hospital’s emergency room. A makeshift blue tarp covering the hospital’s sign is worn down from flapping in the wind. The hospital doors are locked, many in this county of 22,000 fear permanently.
Some residents worry the hospital’s sudden closure last August could cost them their life.
“I know we all have to die, but it seems like since the hospital closed, there’s a lot more people dying,” Linda Gibson, a lifelong resident of Williamston, North Carolina, said on a recent afternoon while preparing snacks for children in a nearby elementary school kitchen.
More than 100 hospitals have downsized services or closed altogether over the past decade in rural communities like Williamston, where people openly wonder if they’d survive the 25-minute ambulance ride to the nearest hospital if they were in a serious car crash.
When Quorum Health shut down Martin County’s 43-bed hospital, citing “financial challenges related to declining population and utilization trends,” residents here didn’t just lose a sense of security. They lost trust, too, in the leaders they elected to make their town a better place to live.
People like 73-year-old Bobby Woolard say they don’t believe any politicians – from the local county commissioners to the presidential candidates who will pass through this swing state with big campaign promises in the coming months – care enough to help them fix the problem.
“If you’re critically ill, there’s no help for you here,” Woolard said on a sunny April afternoon while trimming his neighbor’s hedges. “Nobody seems to care. You got a building sitting there empty and nobody seems to care.”
Trouble for Biden’s health care campaign?
The sentiment in this sharply polarized and segregated eastern North Carolina county could hint at trouble for President Joe Biden, who has made health care a key part of his reelection campaign against Republican rival Donald Trump.
His TV campaign ads hone in on Trump’s promises to diminish the Affordable Care Act. On social media, Biden regularly reminds followers of the law he signed that caps the cost of insulin. And in North Carolina, the campaign is narrowly focused on promoting Democrats’ successful efforts to expand Medicaid, which will extend nearly free government health insurance to thousands of people and reduce the indigent population for hospitals.
Biden and Trump are fiercely competing for the state, which also features the most prominent governor’s race of the year. Martin County, where Williamston is located, voted for Trump in 2020.
“Health care is on the ballot this year, and voters will remember that when they reject Donald Trump in November,” said Dory MacMillan, the Biden campaign’s North Carolina communications director.
But Biden’s achievements might not be enough for crucial voters living in towns like this one in North Carolina, where people have a hard time just getting emergency care when they need it.
Nationally, emergency room wait times have ballooned, with the average emergency room visit taking nearly three hours last year, according to the Centers for Medicare and Medicaid Services. Health care systems are also grappling with a health care worker shortage that worsened after burned-out employees emerged from the pandemic.
Those problems are particularly pronounced in rural communities, where more than 68 hospitals have closed in the last decade. The closures slowed down during the COVID-19 pandemic, when the federal government doled out billions of dollars in extra funds to hospitals. But with that money spent, hospital closures might tick up again, said George Pink, the deputy director of the University of North Carolina’s Sheps Center’s Rural Health Research Program.
Often, it’s emergency room care that residents miss the most, Pink said.
“If you’re having a heart attack, if you’re having a stroke, if you’re giving birth, all those are the kinds of life events where you need access to emergency care quickly and properly,” Pink said. “Those communities that have lost their rural hospitals, they don’t have that.”
A system ‘at risk’
Months before Williamston’s hospital closed, an outside consultant sent a dire warning about emergency care in the county.
The county’s volunteer first responder system was ineffective and long response times that stretched past 15 minutes in some areas were putting “lives at risk,” the consultant told the county’s commissioners last April.
The system was “in desperate need for vision, direction, guidance, command and control, and additional financial support,” the consultant advised the county, according to meeting minutes.
Since Martin General Hospital shut down, things have only gotten worse.
Longer drives to hospitals outside of the county mean ambulances and their crews are tied up for hours sometimes on a run, said Capt. Kenny Warren of the Williamston Fire and Rescue.
“A call that used to take us 20 to 30 minutes is now taking an hour to two hours, depending on where we’ve got to transport to,” Warren said. He added that the agency is staffed with emergency medical technicians, but not paramedics who are trained to provide more advanced care to patients in emergencies.
Warren, however, said he doesn’t think anyone has died as a result.
“Most of the outcomes probably would have been the same anyway,” he said.
In December, first responders arrived on a Williamston street within three minutes of receiving 911 calls that several shots had been fired and a young man might be dead.
They tried unsuccessfully to get a medical helicopter to transport the 21-year-old gunshot victim. The closest option was a six-bed hospital, a 21-minute ambulance ride away. All told, it would take 34 minutes from the time of the 911 call to get him there, according to police dispatch logs. He was transferred from that hospital to a higher-level trauma center where he died a few days later.
The scene of the shooting was just four minutes away from Martin General Hospital’s site.
‘Do you really care?’
More than a dozen Williamston residents interviewed for this story blamed the Martin County Board of Commissioners for failing to prevent the troubled hospital from closing.
Last month, Williamston resident Verna Perry told commissioners that her sister made a 25-minute drive to the closest hospital only to find out she would not be able to get the treatment she needed there.
“Do you really care, commissioners?” Perry asked. “If you cared, you would do something to get us a hospital here.”
Kaitlyn Paxton was seeking treatment for her asthma at Martin General Hospital’s emergency room the day it shut down. She watched staff wheel out patients on stretchers to transfer them to other hospitals.
Since then, she’s had a hard time finding primary care doctors and specialists to replace the ones who left once the hospital closed.
“As far as everyday doctors and appointments, from my personal experience it has been a nightmare trying to find someone,” she said.
She’s used the federally qualified health center, called Agape Health, which is one of a few facilities in the county still offering primary care. More than a thousand of these health centers operate across the U.S. They receive federal government funds and take patients on a sliding pay scale, regardless of their insurance status or ability to pay.
Agape Health added Saturday hours because of an influx of new patients after Martin General closed, said clinic CEO Dr. Michael McDuffie. Last month, Agape reopened one of the orthopedic clinics that shut down along with the hospital.
McDuffie wants to reopen Martin General next, even if just as a stand-alone emergency room.
“It could mean life or death,” McDuffie said. “They need an emergency department here so that it could at least stabilize them.”
The county, which still owns the hospital and land, is consulting with state officials and federal Health and Human Services agency representatives to determine whether the facility can reopen as a Rural Emergency Hospital, said interim County Manager Ben Eisner. Gov. Roy Cooper helped to usher in a new state law that allows North Carolina’s rural hospitals to make the transition.
The Rural Emergency Hospital program was developed by Congress, signed into law by Trump and finetuned by the Biden administration. The designation allows rural hospitals to unlock millions of federal dollars and beef up Medicare payments if they stay open to provide 24/7 emergency care.
“The simple question we’re trying to answer is how do we go from closed to open in a way that makes sense for the citizens of Martin County,” Eisner said.
If successful, Martin County would be the first hospital in the country to reopen its doors after closing with the new federal designation.
“It’s a top priority for us, we live it every day as a community,” Paxton said of getting the hospital reopened. It’ll be top of mind for her when she votes in the presidential election this fall.
Even still, she said: “I do not think it is a top priority for any of them at all – president, senators – any of them.”
-

 News1 week ago
News1 week agoSkeletal remains found almost 40 years ago identified as woman who disappeared in 1968
-

 Movie Reviews1 week ago
Movie Reviews1 week ago“Kingdom of the Planet of the Apes”: Disney's New Kingdom is Far From Magical (Movie Review)
-

 World1 week ago
World1 week agoIndia Lok Sabha election 2024 Phase 4: Who votes and what’s at stake?
-

 World1 week ago
World1 week agoUkraine’s military chief admits ‘difficult situation’ in Kharkiv region
-

 Politics1 week ago
Politics1 week agoTales from the trail: The blue states Trump eyes to turn red in November
-

 World1 week ago
World1 week agoBorrell: Spain, Ireland and others could recognise Palestine on 21 May
-

 World1 week ago
World1 week agoCatalans vote in crucial regional election for the separatist movement
-
 Politics1 week ago
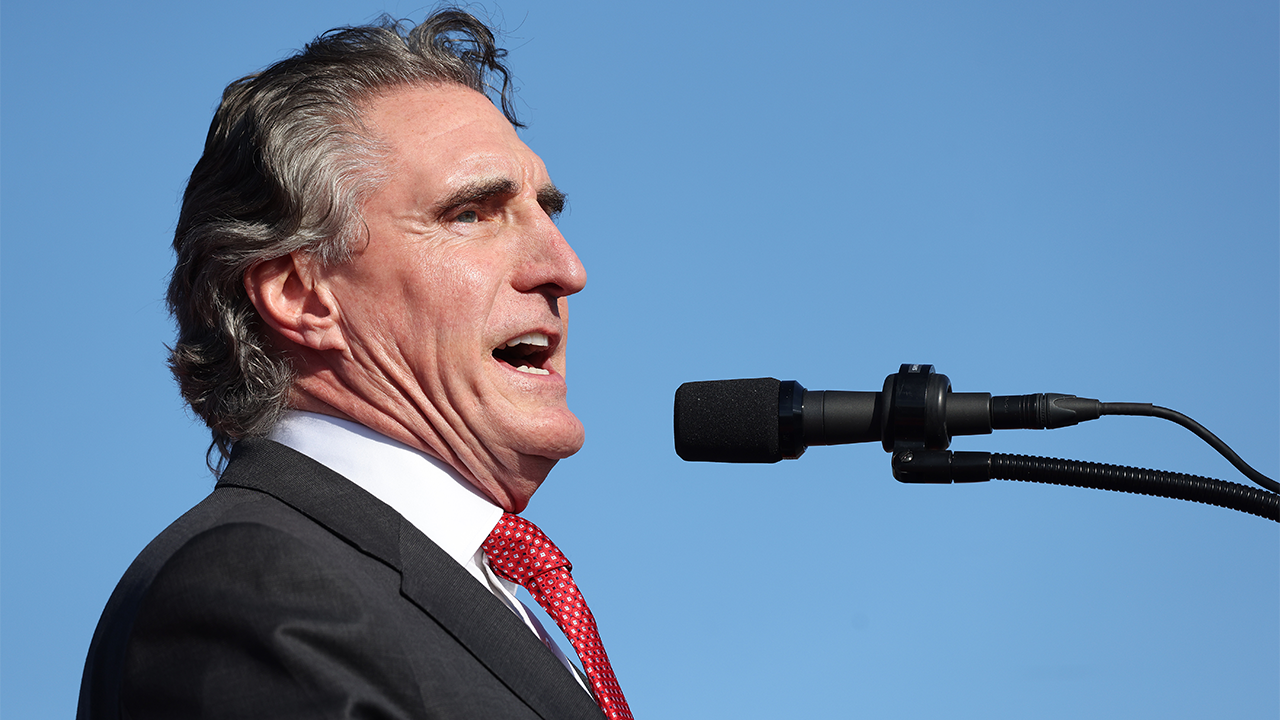
Politics1 week agoNorth Dakota gov, former presidential candidate Doug Burgum front and center at Trump New Jersey rally