Science
Why Measles Outbreaks May Be the New Normal

As the Trump administration moves to dismantle international public health safeguards, pull funding from local health departments and legitimize health misinformation, some experts now fear that the country is setting the stage for a long-term measles resurgence.
If federal health officials do not change course, large multistate outbreaks like the one that has torn through West Texas, jumping to neighboring states and killing two people, may become the norm.
“We have really opened the door for this virus to come back,” said Dr. Thomas R. Frieden, a former director of the Centers for Disease Control and Prevention.
In order for an outbreak to occur in the United States, the virus must first be imported into the country, and it must reach a large, unvaccinated population.
Recent events have made both conditions seem increasingly likely, said Dr. William Moss, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health.
Efforts to control the spread of measles internationally have been disrupted by the Trump administration’s recent decision to withdraw from the World Health Organization, which runs a network of more than 700 laboratories that track measles cases in 164 countries.
The program — which helps to ensure prompt public health responses to emerging outbreaks — relies on the United States to fund its entire $8 million annual budget.
The funds for Gavi were not included on a list the State Department sent to Congress last week of programs it intends to continue to support. But the organization has yet to receive a formal grant termination letter, and its leadership is lobbying the administration to preserve the funding.
Both the W.H.O. withdrawal and the possible loss of Gavi’s funding are likely to cause a surge in measles cases overseas, increasing the likelihood that a U.S. traveler will bring the virus back into the country, said Dr. Walter Orenstein, a professor emeritus at Emory University and the former director of the National Immunization Program at the C.D.C.
“People don’t understand that supporting global immunization not only is good for their countries, but for our country,” he said.
This week’s layoffs at the C.D.C. included staff members who communicate with the public during infectious disease outbreaks and help craft campaigns to encourage vaccination.
Now communications will be centralized at the Department of Health and Human Services, under the control of health secretary Robert F. Kennedy Jr., a vaccine skeptic. The department did not respond to requests for comment.
Dr. Frieden, the former C.D.C. director, described the cuts as “a recipe for disaster.”
The national immunization rate for measles, which fell during the Covid-19 pandemic, has not rebounded to the 95 percent required to stem the spread of the virus in a community. That raises the odds that an imported case will land in a vulnerable population and ignite.
Roughly 93 percent of children in kindergarten had the M.M.R. shot in the 2023-24 school year. But vaccination rates are unevenly distributed; some communities have rates around 80 percent, offset by others where the figure is closer to 99 percent.
Now that H.H.S. has moved to cut billions of dollars to local health departments, they may struggle to quash outbreaks early on, allowing the virus to hop to other unvaccinated communities. (A judge temporarily blocked the funding cuts after a coalition of states sued the Trump administration.)
During infectious disease emergencies, it is local health departments that investigate the source of the pathogen and track down anyone who might have been exposed so they can be quarantined.
The contact-tracing process is time consuming and resource intensive, especially for a virus as contagious as measles.
“A fire is burning and we are at the same time shutting down all the fire departments,” said Jennifer Nuzzo, director of the Pandemic Center at the Brown University School of Public Health.
The current outbreak that began in West Texas shows no signs of slowing. There have been more than 480 cases in the area and 56 hospitalizations since late January. The outbreak has also spread to bordering states, sickening 54 people in New Mexico and 10 in Oklahoma.
Genetic sequencing has suggested that the outbreak is also linked to 24 measles cases discovered in southwest Kansas.
Measles was officially eliminated in the United State in 2000. But the speed at which the Texas outbreak has grown and the fact that it has already jumped to other, under-vaccinated communities makes it very likely that the United States will lose that status, Dr. Nuzzo said.
Measles is no longer considered eliminated if a chain of infections continues for more than twelve months. Public health officials in West Texas have predicted the outbreak will continue for a year.
A large measles outbreak that spread through parts of New York State for nearly 12 months nearly cost the country its elimination status in 2019. The outbreak was contained in large part because of aggressive vaccine mandates, which helped substantially increase childhood immunization rates in the community.
“We just missed it by a hair,” Dr. Nuzzo said. “Where we are now is worse than that.”
Mr. Kennedy has offered muted support for vaccination and has emphasized untested treatments for measles, such as cod liver oil. According to doctors in Texas, his endorsement of alternative treatments has contributed to patients delaying critical care and ingesting toxic levels of vitamin A.
Mr. Kennedy recently tapped a prominent figure in the anti-vaccine movement to work on a study examining the long-debunked theory that vaccines are linked to autism.
If the country does lose elimination status, Dr. Moss said, its unlikely that infection rates will resemble those of the pre-vaccine era, when measles infected nearly every child by age 15.
But it would be likely to mean more frequent and larger outbreaks that make life riskier for society’s most vulnerable: babies too young to be vaccinated, and immunocompromised people.
“There are direct consequences — the health tolls, the long-term health impacts,” Dr. Nuzzo said. “Measles outbreaks are like just incredibly costly and disruptive.”
“It’s also just an embarrassment. It puts the United States on par with some of the most resource-constrained settings in the world, and out of step with most high-income countries.”

Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
Science
When slowing down can save a life: Training L.A. law enforcement to understand autism
Kate Movius moved among a roomful of Los Angeles County sheriff’s deputies, passing out a pop trivia quiz and paper prism glasses.
She told them to put on the vision-distorting glasses, and to write with their nondominant hand. As they filled out the tests, Movius moved about the City of Industry classroom pounding abruptly on tables. Then came the cowbell. An aide flashed the overhead lights on and off at random. The goal was to help the deputies understand the feeling of sensory overwhelm, which many autistic people experience when incoming stimulation exceeds their capacity to process.
“So what can you do to assist somebody, or de-escalate somebody, or get information from someone who suffers from a sensory disorder?” Movius asked the rattled crowd afterward. “We can minimize sensory input. … That might be the difference between them being able to stay calm and them taking off.”
Movius, founder of the consultancy Autism Interaction Solutions, is one of a growing number of people around the U.S. working to teach law enforcement agencies to recognize autistic behaviors and ensure that encounters between neurodevelopmentally disabled people and law enforcement end safely.
She and City of Industry Mayor Cory Moss later passed out bags filled with tools donated by the city to aid interactions: a pair of noise-damping headphones to decrease auditory input, a whiteboard, a set of communication cards with words and images to point to, fidget toys to calm and distract.
“The thing about autistic behavior when it comes to law enforcement is a lot of it may look suspicious, and a lot of it may feel very disrespectful,” said Movius, who is also the parent of an autistic 25-year-old man. Responding officers, she said, “are not coming in thinking, ‘Could this be a developmentally disabled person?’ I would love for them to have that in the back of their minds.”
A sheriff’s deputy reads a pamphlet on autism during the training program.
(Genaro Molina / Los Angeles Times)
Autism spectrum disorder is a developmental condition that manifests differently in nearly every person who has it. Symptoms cluster around difficulties in communication, social interaction and sensory processing.
An autistic person stopped by police might hold the officer’s gaze intensely or not look at them at all. They may repeat a phrase from a movie, repeat the officer’s question or temporarily lose their ability to speak. They might flee.
All are common involuntary responses for an autistic person in a stressful situation, which a sudden encounter with law enforcement almost invariably is. To someone unfamiliar with the condition, all could be mistaken for intoxication, defiance or guilt.
Autism rates in the U.S. have increased nearly fivefold since the Centers for Disease Control began tracking diagnoses in 2000, a rise experts attribute to broadening diagnostic criteria and better efforts to identify children who have the condition.
The CDC now estimates that 1 in 31 U.S. 8-year-olds is autistic. In California, the rate is closer to 1 in 22 children.
As diverse as the autistic population is, people across the spectrum are more likely to be stopped by law enforcement than neurotypical peers.
About 15% of all people in the U.S. ages 18 to 24 have been stopped by police at some point in their lives, according to federal data. While the government doesn’t track encounters for disabled people specifically, a separate study found that 20% of autistic people ages 21 to 25 have been stopped, often after a report or officer observation of a person behaving unusually.
Some of these encounters have ended in tragedy.
In 2021, Los Angeles County sheriff’s deputies shot and permanently paralyzed a deaf autistic man after family members called 911 for help getting him to a hospital.
Isaias Cervantes, 25, had become distressed about a shopping trip and started pushing his mother, his family’s attorney said at the time. He resisted as two deputies attempted to handcuff him and one of the deputies shot him, according to a county report.
In 2024, Ryan Gainer’s family called 911 for support when the 15-year-old became agitated. Responding San Bernardino County sheriff‘s deputies shot and killed him outside his Apple Valley home.
Last year, police in Pocatello, Idaho, shot Victor Perez, 17, through a chain-link fence after the nonspeaking teenager did not heed their shouted commands. He died from his injuries in April.

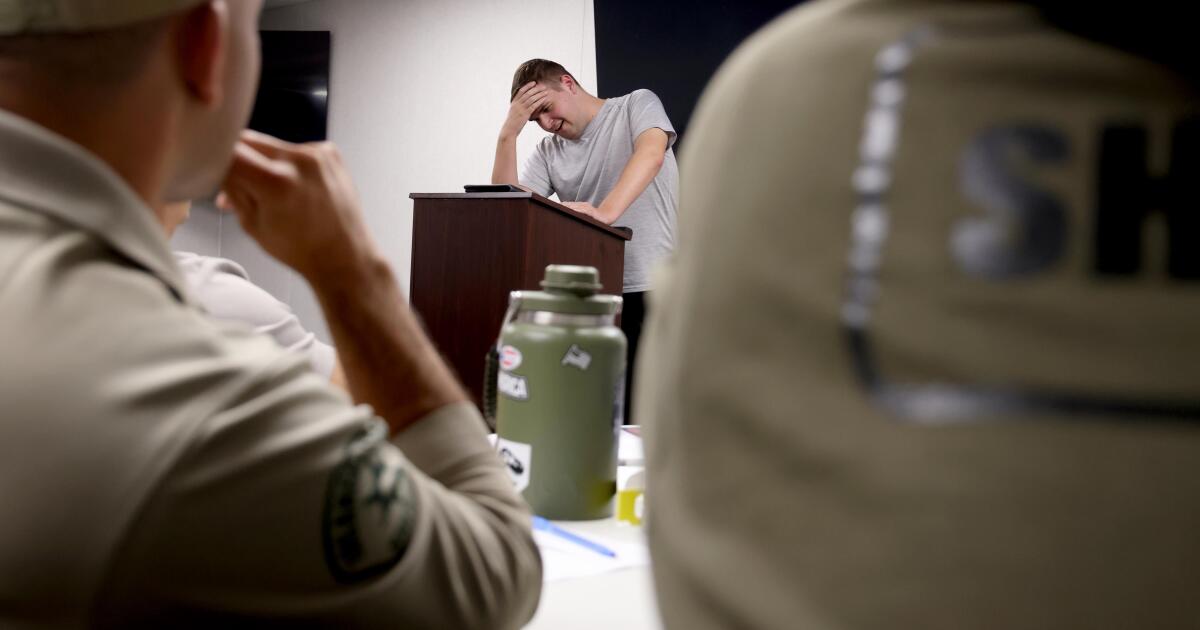
Sheriff’s deputies take a trivia quiz using their non-writing hands, while wearing vision-distorting glasses, as Kate Movius, standing left, and Industry Mayor Cory Moss, right, ring cowbells. The idea was to help them understand the sensory overwhelm some autistic people experience.
(Genaro Molina / Los Angeles Times)
As early as 2001, the FBI published a bulletin on police officers’ need to adjust their approach when interacting with autistic people.
“Officers should not interpret an autistic individual’s failure to respond to orders or questions as a lack of cooperation or as a reason for increased force,” the bulletin stated. “They also need to recognize that individuals with autism often confess to crimes that they did not commit or may respond to the last choice in a sequence presented in a question.”
But a review of multiple studies last year by Chapman University researchers found that while up to 60% of officers have been on a call involving an autistic person, only 5% to 40% had received any training on autism.
In response, universities, nonprofits and private consultants across the U.S. have developed curricula for law enforcement on how to recognize autistic behaviors and adapt accordingly.
The primary goal, Movius told deputies at November’s training session, is to slow interactions down to the greatest extent possible. Many autistic people require additional time to process auditory input and verbal responses, particularly in unfamiliar circumstances.
If at all possible, Movius said, wait 20 seconds for a response after asking a question. It may feel unnaturally long, she acknowledged. But every additional question or instruction fired in that time — what’s your name? Did you hear me? Look at me. What’s your name? — just decreases the likelihood that a person struggling to process will be able to respond at all.
Moss’ son, Brayden, then 17, was one of several teenagers and young adults with autism who spoke or wrote statements to be read to the deputies. The diversity of their speech patterns and physical mannerisms showed the breadth of the spectrum. Some were fluently verbal, while others communicated through signs and notes.
“This population is so diverse. It is so complicated. But if there’s anything that we can show [deputies] in here that will make them stop and think, ‘Hey, what if this is autism?’ … it is saving lives,” Moss said.

Mayor Cory Moss, left, and Kate Movius hug at the end of the training program last November. Movius started Autism Interaction Solutions after her son was born with profound autism.
(Genaro Molina / Los Angeles Times)
Some disability advocates cautioned that it takes more than isolated training sessions to ensure encounters end safely.
Judy Mark, co-founder and president of the nonprofit Disability Voices United, says she trained thousands of officers on safe autism interactions but stopped after Cervantes’ shooting. She now urges families concerned about an autistic child’s safety to call an ambulance rather than law enforcement.
“I have significant concern about these training sessions,” Mark said. “People get comfort from it, and the Sheriff’s Department can check the box.”
While not a panacea, supporters argue that a brief course is better than no preparation at all. Some years ago, Movius received a letter from a man whose profoundly autistic son slipped away as the family loaded their car at the beach. He opened the unlocked door of a police vehicle, climbed into the back and began to flail in distress.
Though surprised, the officer seated at the wheel de-escalated the situation and helped the young man find his family, the father wrote to Movius. He had just been to her training.
Science
Bodies of all 9 skiers killed in devastating avalanche recovered by authorities

California search-and-rescue teams have recovered the bodies of all nine missing skiers killed Tuesday in a devastating avalanche in a remote region of Sierra Nevada north of Lake Tahoe.
When a catastrophic avalanche rumbled over a stretch of the High Sierra, dozens of law enforcement officers scoured the mountainside for a group of 15 skiers, including four mountain guides.
Within hours, crews rescued six survivors and discovered eight deceased skiers near the Frog Lake Backcountry Huts. Another skier was still missing, but was presumed dead.
After five days of navigating deep snowpack and treacherous weather conditions, authorities announced they had found the body of the ninth victim.
During a press conference on Saturday afternoon, Nevada County identified the victims as six skiers and three professional mountain guides:
- Andrew Alissandratos, 34, of Verdi, Nev., a Blackbird Mountain Guide
- Carrie Atkin, 46, of Soda Springs, Calif.
- Nicole Choo, 42, of South Lake Tahoe, Calif., Blackbird Mountain Guide
- Lizabeth Clabaugh, 52, of Boise, Idaho
- Michael Henry, 30, from Soda Springs, Calif., a Blackbird Mountain Guide
- Danielle Keatley, 44, of Soda Springs and Larkspur, Calif.
- Kate Morse, 45, of Soda Springs and Tiburon, Calif.
- Caroline Sekar, 45, of Soda Springs and San Francisco, Calif.
- Katherine Vitt, 43, of Greenbrae, Calif.
Authorities lamented the fast-moving disaster as the deadliest avalanche in modern California history.
“There are no words that truly capture the significance of this loss and our hearts mourn alongside the families of those affected by this catastrophic event,” Nevada County Sheriff Shannan Moon said in a statement on Saturday. “The weight of this event is felt across many families, friends, and colleagues, and we stand together with them during this difficult time.” Moon said.
The avalanche occurred amid a powerful atmospheric river storm that unleashed several feet of snow onto the Sierra Nevada mountains. First responders maneuvered through the blizzard on snowcats and skis to rescue the survivors.
But the unstable snowpack, high winds and whiteout conditions made search-and-recovery efforts too perilous, prompting first responders to leave behind the bodies of deceased skiers and suspend operations on Wednesday and Thursday.
Authorities carved paths through the deep snow to eventually continue the search, and California Highway Patrol officers found the ninth victim.
The Nevada County Sheriff‘s Office was also assisted by California National Guard, California State Parks, Placer County Sheriff’s Office, Washoe County Sheriff’s Office, California Governor’s Office of Emergency Services, Truckee Police Department and the United States Forest Service.
-

 World10 hours ago
World10 hours agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts19 hours ago
Massachusetts19 hours agoMother and daughter injured in Taunton house explosion
-

 Montana6 days ago
Montana6 days ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Oklahoma1 week ago
Oklahoma1 week agoWildfires rage in Oklahoma as thousands urged to evacuate a small city
-

 Louisiana3 days ago
Louisiana3 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Technology5 days ago
Technology5 days agoYouTube TV billing scam emails are hitting inboxes
-

 Culture1 week ago
Culture1 week agoTest Your Knowledge of the Authors and Events That Helped Shape the United States
-

 Technology5 days ago
Technology5 days agoStellantis is in a crisis of its own making























