Science
Avocados, salmon, strawberry yogurt: Which of these meets FDA's new definition of a “healthy” food?

In an effort to improve American diets, the U.S. Food and Drug Administration Thursday released a new definition of what it means for a food to qualify as “healthy.”
Products like fruit-flavored yogurt, fortified white bread and sweetened energy bars will no longer be allowed to label themselves as healthy if they exceed certain limits on saturated fat, sodium and added sugars.
At the same time, foods like salmon, almonds and even water will qualify as healthy for the first time.
The new definition reflects the advice offered in the Dietary Guidelines for Americans, which are produced by the Department of Agriculture and the Department of Health and Human Services. The hope is that consumers who consider health claims on packaged foods while filling their grocery carts will be steered toward a more nutritious eating pattern, the FDA said.
There’s no question that Americans can use some help with their diets. For example, less than half of U.S. adults eat a piece of fruit on any given day, and only 12% consume the recommended 1.5 to 2 cups of fruit per day, according to national surveys conducted by the Centers for Disease Control and Prevention. Americans are even further off the mark with vegetables, with only 10% meeting the target of 2 to 3 cups per day.
On the other hand, 90% of us eat too much sodium, 75% eat too much saturated fat and 63% eat too many added sugars, the FDA said.
The new definition of healthy foods aims to turn that around by excluding foods with excess sodium, saturated fat and added sugars even if they also contain valuable nutrients like protein and whole grains.
The specific limits vary depending on food groups. The limits will also depend on whether a product is an individual food (like cheese), a “mixed product” (like trail mix) or a complete meal (like a frozen dinner).
For instance, in order for a dairy product such as yogurt to qualify as healthy, a single 2/3-cup serving can’t have more than 5% of the recommended daily amount of added sugars, 10% of the recommended daily amount of sodium or 10% of the recommended daily amount of saturated fat.
Those limits translate to 2.5 grams of added sugars, 230 milligrams of sodium and 2 grams of saturated fat. A single serving of Chobani strawberry Greek yogurt would miss the mark because it contains 9 grams of added sugars. So would Chobani’s “less sugar” variety, which has 5 grams of added sugars.
Sugar, salt and fat are only part of the new criteria. To meet the new definition of healthy, foods must contain a minimum amount of protein, whole grains, fruit, vegetables or fat-free or low-fat dairy, the FDA said.
Whole foods like eggs, beans, seafood and nuts will automatically qualify as healthy if they are sold with no added ingredients (except for water). That makes foods like avocados, olive oil and higher-fat fish like salmon eligible to be labeled as healthy for the first time. Fruits, vegetables and fish can make the cut if they are fresh, frozen or canned, making them accessible to people on a range of budgets, the agency said.
However, products like fortified breads, cereals, fruit snacks, granola bars and fruit punch will lose the label unless they are reformulated to meet the new definition.
Nancy Brown, chief executive of the American Heart Assn., said the new definition was long overdue and hopes it will improve Americans’ diets by motivating food manufacturers to create healthier products. However, she added that it would be more meaningful to require products to carry a nutrition label on the front of their packages, which she believes would make it easier for consumers to identify and select healthier options.
The previous definition of healthy foods, which was issued in 1994, focused more on total fat and cholesterol. Since then, nutrition scientists have recognized that not all fats should be treated the same, and that unsaturated fats found in nuts, seeds, fish and certain vegetable oils can lower disease risk.
The old definition also required foods to provide at least 10% of the recommended daily amount of vitamin A, vitamin C, calcium, iron, protein or fiber. The FDA said it is shifting its focus from specific nutrients to larger food groups in order to help consumers build a healthy dietary pattern.
Poor diet is a risk factor for many of the leading causes of death in the U.S., including heart disease, stroke, diabetes and some types of cancer.
Food manufacturers will have three years to conform to the new definition, the FDA said, though those that meet the new criteria don’t have to wait that long to start using the “healthy” label.

Science
Newsom’s fight with Trump and RFK Jr. on public health
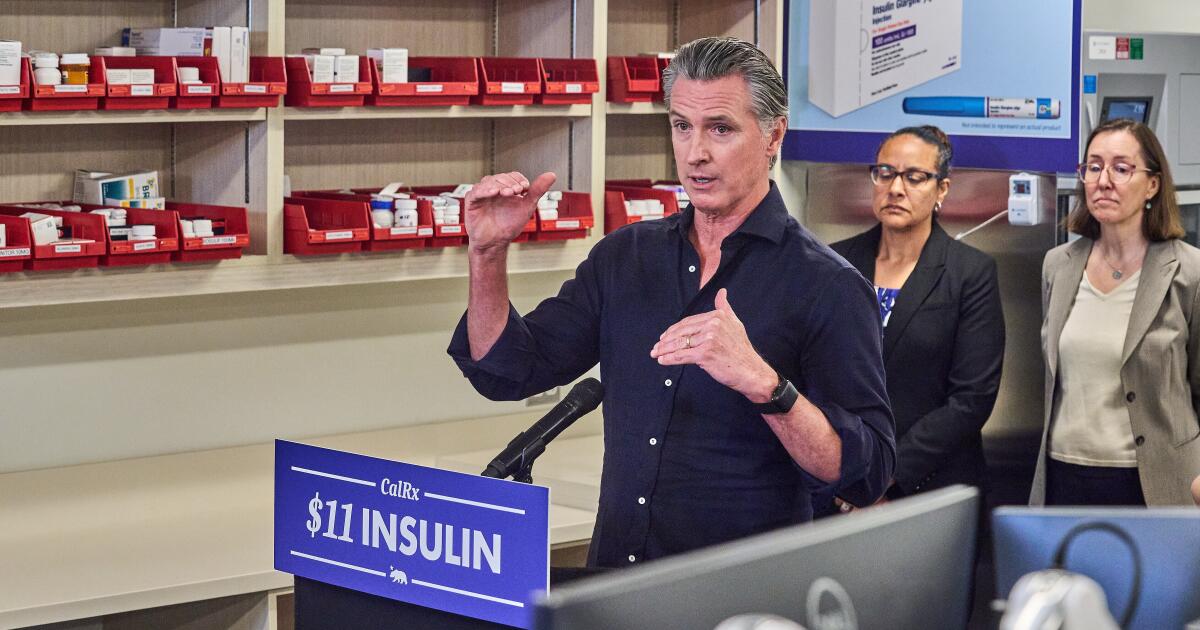
SACRAMENTO — California Gov. Gavin Newsom has positioned himself as a national public health leader by staking out science-backed policies in contrast with the Trump administration.
After Health and Human Services Secretary Robert F. Kennedy Jr. fired Centers for Disease Control and Prevention Director Susan Monarez for refusing what her lawyers called “the dangerous politicization of science,” Newsom hired her to help modernize California’s public health system. He also gave a job to Debra Houry, the agency’s former chief science and medical officer, who had resigned in protest hours after Monarez’s firing.
Newsom also teamed up with fellow Democratic governors Tina Kotek of Oregon, Bob Ferguson of Washington and Josh Green of Hawaii to form the West Coast Health Alliance, a regional public health agency, whose guidance the governors said would “uphold scientific integrity in public health as Trump destroys” the CDC’s credibility. Newsom argued establishing the independent alliance was vital as Kennedy leads the Trump administration’s rollback of national vaccine recommendations.
More recently, California became the first state to join a global outbreak response network coordinated by the World Health Organization, followed by Illinois and New York. Colorado and Wisconsin signaled they plan to join. They did so after President Trump officially withdrew the United States from the agency on the grounds that it had “strayed from its core mission and has acted contrary to the U.S. interests in protecting the U.S. public on multiple occasions.” Newsom said joining the WHO-led consortium would enable California to respond faster to communicable disease outbreaks and other public health threats.
Although other Democratic governors and public health leaders have openly criticized the federal government, few have been as outspoken as Newsom, who is considering a run for president in 2028 and is in his second and final term as governor. Members of the scientific community have praised his effort to build a public health bulwark against the Trump administration’s slashing of funding and scaling back of vaccine recommendations.
What Newsom is doing “is a great idea,” said Paul Offit, an outspoken critic of Kennedy and a vaccine expert who formerly served on the Food and Drug Administration’s vaccine advisory committee but was removed under Trump in 2025.
“Public health has been turned on its head,” Offit said. “We have an anti-vaccine activist and science denialist as the head of U.S. Health and Human Services. It’s dangerous.”
The White House did not respond to questions about Newsom’s stance and Health and Human Services declined requests to interview Kennedy. Instead, federal health officials criticized Democrats broadly, arguing that blue states are participating in fraud and mismanagement of federal funds in public health programs.
Health and Human Services spokesperson Emily Hilliard said the administration is going after “Democrat-run states that pushed unscientific lockdowns, toddler mask mandates, and draconian vaccine passports during the COVID era.” She said those moves have “completely eroded the American people’s trust in public health agencies.”
Public health guided by science
Since Trump returned to office, Newsom has criticized the president and his administration for engineering policies that he sees as an affront to public health and safety, labeling federal leaders as “extremists” trying to “weaponize the CDC and spread misinformation.” He has excoriated federal officials for erroneously linking vaccines to autism, warning that the administration is endangering the lives of infants and young children in scaling back childhood vaccine recommendations. And he argued that the White House is unleashing “chaos” on America’s public health system in backing out of the WHO.
The governor declined an interview request, but Newsom spokesperson Marissa Saldivar said it’s a priority of the governor “to protect public health and provide communities with guidance rooted in science and evidence, not politics and conspiracies.”
The Trump administration’s moves have triggered financial uncertainty that local officials said has reduced morale within public health departments and left states unprepared for disease outbreaks and prevention efforts. The White House last year proposed cutting Health and Human Services spending by $33 billion, including $3.6 billion from the CDC. Congress largely rejected those cuts last month, although funding for programs focusing on social drivers of health, such as access to food, housing and education, were axed.
The Trump administration announced that it would claw back more than $600 million in public health funds from California, Colorado, Illinois and Minnesota, arguing that the Democratic-led states were funding “woke” initiatives that didn’t reflect White House priorities. Within days, the states sued and a judge temporarily blocked the cut.
“They keep suddenly canceling grants and then it gets overturned in court,” said Kat DeBurgh, executive director of the Health Officers Assn. of California. “A lot of the damage is already done because counties already stopped doing the work.”
Federal funding has accounted for more than half of state and local health department budgets nationwide, with money going toward fighting HIV and other sexually transmitted infections, preventing chronic diseases, and boosting public health preparedness and communicable disease response, according to a 2025 analysis by KFF, a health information nonprofit that includes KFF Health News.
Federal funds account for $2.4 billion of California’s $5.3-billion public health budget, making it difficult for Newsom and state lawmakers to backfill potential cuts. That money helps fund state operations and is vital for local health departments.
Funding cuts hurt all
Los Angeles County public health director Barbara Ferrer said if the federal government is allowed to cut that $600 million, the county of nearly 10 million residents would lose an estimated $84 million over the next two years, in addition to other grants for prevention of HIV and other sexually transmitted infections. Ferrer said the county depends on nearly $1 billion in federal funding annually to track and prevent communicable diseases and combat chronic health conditions, including diabetes and high blood pressure. Already, the county has announced the closure of seven public health clinics that provided vaccinations and disease testing, largely because of funding losses tied to federal grant cuts.
“It’s an ill-informed strategy,” Ferrer said. “Public health doesn’t care whether your political affiliation is Republican or Democrat. It doesn’t care about your immigration status or sexual orientation. Public health has to be available for everyone.”
A single case of measles requires public health workers to track down 200 potential contacts, Ferrer said.
The U.S. eliminated measles in 2000 but is close to losing that status as a result of vaccine skepticism and misinformation spread by vaccine critics. The U.S. had 2,281 confirmed cases last year, the most since 1991, with 93% in people who were unvaccinated or whose vaccination status was unknown. This year, the highly contagious disease has been reported at schools, airports and Disneyland.
Public health officials hope the West Coast Health Alliance can help counteract Trump by building trust through evidence-based public health guidance.
“What we’re seeing from the federal government is partisan politics at its worst and retaliation for policy differences, and it puts at extraordinary risk the health and well-being of the American people,” said Georges Benjamin, executive director of the American Public Health Assn., a coalition of public health professionals.
Robust vaccine schedule
Erica Pan, California’s top public health officer and director of the state Department of Public Health, said the West Coast Health Alliance is defending science by recommending a more robust vaccine schedule than the federal government. California is part of a coalition suing the Trump administration over its decision to rescind recommendations for seven childhood vaccines, including for hepatitis A, hepatitis B, influenza and COVID-19.
Pan expressed deep concern about the state of public health, particularly the uptick in measles. “We’re sliding backwards,” Pan said of immunizations.
Sarah Kemble, Hawaii’s state epidemiologist, said Hawaii joined the alliance after hearing from pro-vaccine residents who wanted assurance that they would have access to vaccines.
“We were getting a lot of questions and anxiety from people who did understand science-based recommendations but were wondering, ‘Am I still going to be able to go get my shot?’” Kemble said.
Other states led mostly by Democrats have also formed alliances, with Pennsylvania, New York, New Jersey, Massachusetts and several other East Coast states banding together to create the Northeast Public Health Collaborative.
Hilliard, of Health and Human Services, said that even as Democratic governors establish vaccine advisory coalitions, the federal Advisory Committee on Immunization Practices “remains the scientific body guiding immunization recommendations in this country, and HHS will ensure policy is based on rigorous evidence and gold standard science, not the failed politics of the pandemic.”
Influencing red states
Newsom, for his part, has approved a recurring annual infusion of nearly $300 million to support the state Department of Public Health, as well as the 61 local public health agencies across California, and last year signed a bill authorizing the state to issue its own immunization guidance. It requires health insurers in California to provide patient coverage for vaccinations the state recommends even if the federal government doesn’t.
Jeffrey Singer, a doctor and senior fellow at the libertarian Cato Institute, said decentralization can be beneficial. That’s because local media campaigns that reflect different political ideologies and community priorities may have a better chance of influencing the public.
A KFF analysis found some red states are joining blue states in decoupling their vaccine recommendations from the federal government’s. Singer said some doctors in his home state of Arizona are looking to more liberal California for vaccine recommendations.
“Science is never settled, and there are a lot of areas of this country where there are differences of opinion,” Singer said. “This can help us challenge our assumptions and learn.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling and journalism.
Science
How Rising Home Insurance Costs Are Linked to Credit Scores

Two friends bought nearly identical homes last year, in the same northern Minnesota neighborhood, for the same price.
But Tara Novak pays more than twice as much for home insurance as Petra Rodriguez. The only difference? Ms. Novak has a lower credit score.
Across the country, people with weaker credit histories are paying far more for home insurance than owners with spotless records.
Where the home insurance rate gap between “fair” and “excellent” credit is higher
Home insurance premiums have risen rapidly in recent years, fueled by climate change, building costs and inflation. The price shock has rippled into the real estate market, dragging down home prices in areas vulnerable to disasters and leading insurers to abandon homeowners in risky places.
But these dynamics obscure another problem: The home insurance market has cleaved in two along a boundary defined more by a customer’s personal history than by the risk of a disaster hitting their home.
Americans with weaker credit histories, usually from missed payments or high amounts of debt, now pay significantly more for insurance, regardless of where they live, two new studies have found. While those with poor credit histories often can’t purchase homes at all, people with “fair” scores, which range from around 580 to 669, are paying twice as much in some places as people with “excellent” scores of about 800 or higher. And the gap is growing.
Insurers use a metric based on credit history known as an insurance score to set rates, and the figure tracks closely with a customer’s credit score.
The penalty for having a “fair” credit history versus an “excellent” one
States with the biggest pricing gaps
That can mean owners of identical homes, like Ms. Novak and Ms. Rodriguez, pay wildly different rates to insure them. For most people, it’s now just as expensive to have a credit score of “fair” as it is to live in an area likely to experience a disaster like a hurricane or wildfire. About 29 percent of consumers have credit scores that are categorized as “fair” or “poor.”
“There’s so many reasons people have bad credit,” Ms. Novak said. “It’s not like I’ve ever not paid a bill on time. I’m a stickler on my bills, I’m a stickler on my rent, never been late. This is not fair.”
“The choice to use credit scores in pricing means that those lower-credit home owners in risky areas are effectively subsidizing more affluent high-credit homeowners who also live in risky areas,” said Nick Graetz, assistant professor of sociology at the University for Minnesota, who wrote one of the recent papers. “So in a lot of ways, you can keep your insurance price down if you’re high income, high credit — even if you live on the coast of Florida.”
A handful of states have banned insurers from using credit data because of concerns about fairness and the potential for discrimination against low-income people and people of color, but the majority allow it.
For those with both weaker credit and high disaster risk, the combination can set them up for a downward spiral: disasters tend to be followed by decreases in credit scores as people use credit cards and bank loans to recover. That can lead to higher insurance rates, pushing monthly housing costs further out of reach.
“When a disaster hits, there’s a loss of income that occurs, and then that can impact someone’s credit score because they can’t pay their debt, they can’t pay their rent, they can’t pay their mortgage,” said Lance Triggs, executive vice president at Operation HOPE, a financial literacy nonprofit. “And now they’re faced with higher insurance premiums post-disaster.”
A working paper released today by the National Bureau of Economic Research found that homeowners with the lowest credit scores paid, on average, $550 more in 2024 for home insurance than those with the highest scores.
The findings broadly track with data from Quadrant Information Services analyzed by The New York Times, which found that, on average, lower credit scores meant higher premiums across every state that allowed the practice. Dr. Graetz used the same data set for his research, which he did in collaboration with the Consumer Federation of America and the Climate and Community Institute.
When a windstorm last year hit the home of Audrey Thayer, a city council member in Bemidji, Minn., it ripped the siding off her house and stripped shingles from her roof.
Ms. Thayer’s insurance did not cover all the damage. As she fought her insurer for more money, she opened new credit cards and bank loans to repair her home. Her credit score dropped as she tried to find a new insurance plan.
Ms. Thayer, a member of the White Earth Nation, said she was not aware that her credit score could affect her home insurance rates, even though she teaches about credit ratings at a nearby tribal college. “Most of the folks here do not have good credit,” said Ms. Thayer, whose community is one of the poorest in the state. “I did not know what a credit score was until I was 35 or so.”
In Texas, the advocacy group Texas Appleseed found that some insurers charge people with poor credit up to 12 times as much as people with excellent credit for certain policies, said Ann Baddour, the director of the nonprofit’s Fair Financial Services Project.
Higher costs have serious implications for low-income homeowners who live in the path of hurricanes, said Nadia Erosa, the operations manager at Come Dream Come Build, a nonprofit community housing development organization. After the Brownsville, Texas, region saw intense flooding last spring, some residents turned to companies offering high-interest loans to fund repairs, she said, raising the risk of the disaster-credit spiral.
“Delinquencies are going up because people cannot afford their payment,” she said.
The price of risk
Before they can get a mortgage, homebuyers are usually required by lenders to purchase home insurance.
“Households with insurance have fewer financial burdens, fewer unmet needs, they recover faster, they’re more likely to rebuild,” said Carolyn Kousky, an economist and founder of Insurance for Good, a nonprofit that focuses on finding new approaches to risk management. “Yet the people who need insurance the most are the least able to afford it.”
Insurance companies consider a variety of factors when setting the premium for a property. They might examine the age of the roof, or the area’s vulnerability to hurricanes or wildfires. They factor in how much it would cost to rebuild the house if it were damaged.
Insurers have argued that credit history is also worth considering because people with low scores tend to file more claims than those with excellent scores, an assertion that is backed up by the working paper published in the National Bureau of Economic Research today. This likely happens because people with weaker credit histories tend to have less income, and when their home is damaged, they file insurance claims for smaller fixes that a wealthier homeowner might pay for out of pocket.
Paul Tetrault, senior director at the American Property Casualty Insurance Association, a trade organization, said credit scores are a valid way to price premiums.
But others argue that using credit information to price insurance doesn’t make sense.
Because a homeowner pays for insurance upfront, “it’s not like you’re really extending a loan to the customer where you would be worried about the risk of repayment,” Ms. Kousky said. She points out that insurance companies can opt not to renew a homeowner’s policy if they believe it is too risky — a tactic they have been using with increasing frequency.
The NBER analysis found that homeowners who want to pay less for insurance should pay off debt to raise their credit score rather than replace roofs and make other improvements to avoid damage when disaster strikes.
Others believe that even if credit scores are accurate predictors of future claims, they shouldn’t be used to set premiums because that can perpetuate or worsen disparities. For example, people in their mid-20s who are Black, low-income, or grow up in impoverished regions have significantly lower credit scores than their peers, a July working paper from Opportunity Insights, a not-for-profit organization at Harvard University, found.
“When the government and the financial system mandate that we buy a product, there’s a special obligation to make sure the pricing is fair,” said Doug Heller, director of insurance at the Consumer Federation. “To me that is an absolutely solid reason, just like we don’t allow pricing based on race or income or ethnicity or religion.”
A natural experiment
A handful of states, including California and Massachusetts, have banned or limited the use of credit scores in setting home insurance premiums, despite opposition from the insurance industry.
In Nevada, where a temporary pandemic-related rule prevented insurers from using credit history to increase premiums for existing customers from 2020 to 2024, companies refunded approximately $27 million to nearly 200,000 policyholders, said Drew Pearson, a spokesman for the Nevada Division of Insurance.
Perhaps the clearest example of the effects of these bans comes from Washington State, which banned the use of credit information in setting home insurance premiums starting in June 2021. The rule immediately faced legal challenges, and was in effect for just a few months until it was overturned in court.
But the episode allowed researchers to evaluate the effect of credit factors on insurance premiums. When the rule took effect, people with the lowest credit scores saw a decrease in premiums of about $175 annually while those with the highest scores saw an increase of about $100, the NBER analysis found.
“We could see the dynamics of insurance pricing for the same households over time,” said Benjamin Keys, a professor at the University of Pennsylvania’s Wharton School, who co-authored the paper.
What homeowners paid before and after a ban on credit-based pricing in Washington State
Values compared with premiums paid by homeowners with “medium” credit scores (717 to 756)
In Minnesota, where Tara Novak, Petra Rodriguez and Audrey Thayer live, a state task force looked at ways to lower insurance costs for residents. It recently considered a ban or limit on the use of credit scores to set rates, but did not move forward with a recommendation.
Ms. Rodriguez said she doesn’t think it’s fair that her friend Ms. Novak should have to pay so much more for insurance to live in an identical house.
A credit score doesn’t capture anything about a person’s habits, or what they’re like as a tenant, or even years of on-time rent payments, she said. “It’s not who you are,” she said.
Methodology
Home insurance policy rates were supplied by Quadrant Information Services, an insurance data solutions company. The rates shown are representative of publicly sourced filings and should not be interpreted as bindable quotes. Actual individual premiums may vary.
‘States with the biggest pricing gaps’Rates shown are based on a home insurance policy with $400,000 of dwelling coverage and a $100,000 liability limit on a new home, for a homeowner age 50 or younger. Rates are averaged for all the individual company filings represented in the sample, which add up to a majority of the market share in each state but do not cover all active insurers in the state. Rates are also averaged to the state level from zip code level data.
‘The credit penalty in each state’Each insurance company incorporates credit history information differently, often using proprietary methods, so the scores do not map directly to FICO credit scores.
‘What homeowners paid before and after a ban on credit-based pricing in Washington State’Data shown are based on observations of real home insurance policies and homeowner credit scores from ICE McDash analyzed by the researchers of Blonz, Hossain, Keys, Mulder and Weill (2026). The price comparisons across credit score tiers controlled for variance in disaster risk, insurance policy characteristics, geography, and other year to year fluctuations.
Science
Earth is warming faster than previously estimated, new study shows

Planetary warming has significantly accelerated over the past 10 years, with temperatures rising at a higher rate since 2015 than in any previous decade on record, a new study showed.
The Earth warmed around 0.35 degrees Celsius in the decade to 2025, compared to just under 0.2C per decade on average between 1970 and 2015, according to a paper published on Friday in the scientific journal Geophysical Research Letters. This is the first statistically significant evidence of an acceleration of global warming, the authors said.
The past three years have been the hottest on record, compared to the average before the Industrial Revolution. In 2024, warming went past 1.5C, the lower limit set by the Paris Agreement. That target refers to temperature increases over 20 years, but breaching it for one year shows efforts to slow down climate change have been insufficient, the scientists who wrote the new paper said.
The findings shed light on an ongoing debate among researchers. While there is consensus that greenhouse gas emissions have caused the planet to heat up since pre-industrial times, that warming had been steady for decades. But record-breaking temperatures in recent years have led scientists to question whether the pace of temperature gains is accelerating.
Demonstrating that was difficult due to natural fluctuations in temperatures. The researchers filtered out the “noise” to make the “underlying long-term warming signal” more clearly visible, said Grant Foster, a co-author of the study and a U.S.-based statistics expert.
Researchers isolated phenomena including the El Niño weather phase, volcanic eruptions and solar irradiance. When looking at temperature increases without their influence, the authors concluded the evidence is “strong” that the accelerated warming was not due to an unusually hot 2023 and 2024, but that since 2015 global temperatures departed from their previous, slower path of warming.
The new report adds to a growing body of work that indicates climate change is having a quicker and larger impact on the planet than scientists have understood. A separate paper published this week found that many studies on sea-level increases underestimate how much water along the coast has already risen.
“If the warming rate of the past 10 years continues, it would lead to a long-term exceedance of the 1.5C limit of the Paris Agreement before 2030,” said Stefan Rahmstorf, the lead author of the warming study and a researcher at the Potsdam Institute for Climate Impact Research. “How quickly the Earth continues to warm ultimately depends on how rapidly we reduce global CO2 emissions from fossil fuels to zero.”
Millan writes for Bloomberg.
-

 Wisconsin1 week ago
Wisconsin1 week agoSetting sail on iceboats across a frozen lake in Wisconsin
-

 Massachusetts6 days ago
Massachusetts6 days agoMassachusetts man awaits word from family in Iran after attacks
-

 Maryland1 week ago
Maryland1 week agoAM showers Sunday in Maryland
-

 Florida1 week ago
Florida1 week agoFlorida man rescued after being stuck in shoulder-deep mud for days
-

 Pennsylvania4 days ago
Pennsylvania4 days agoPa. man found guilty of raping teen girl who he took to Mexico
-

 Oregon1 week ago
Oregon1 week ago2026 OSAA Oregon Wrestling State Championship Results And Brackets – FloWrestling
-

 News1 week ago
News1 week ago2 Survivors Describe the Terror and Tragedy of the Tahoe Avalanche
-

 Sports5 days ago
Sports5 days agoKeith Olbermann under fire for calling Lou Holtz a ‘scumbag’ after legendary coach’s death
















