Science
This rural hospital closed, putting lives at risk. Is it the start of a ‘tidal wave’?

WILLOWS — As hospital staff carted away medical equipment from abandoned patient rooms, Theresa McNabb, 74, roused herself and painstakingly applied make-up for the first time in weeks, finishing with a mauve lipstick that made her eyes pop.
“I feel a little anxiety,” McNabb said. She was still taking multiple intravenous antibiotics for the massive infection that had almost killed her, was unsteady on her feet and was unsure how she was going to manage shopping and cooking food for herself once she returned to her apartment after six weeks in the hospital.
But she couldn’t stay at Glenn Medical Center. It was closing.
The hospital — which for more than seven decades has treated residents of its small farm town about 75 miles north of Sacramento, along with countless victims of car crashes on nearby Interstate 5 and a surprising number of crop-duster pilots wounded in accidents — shut its doors on Oct. 21.
McNabb was the last patient.
Registered nurse Ronald Loewen, 74, checks on one of the last few patients. Loewen, a resident of Glenn County and a former Mennonite school teacher, said the hospital closing is “a piece of our history gone.”
Nurses and other hospital workers gathered at her room to ceremonially push her wheelchair outside and into the doors of a medical transport van. Then they stood on the lawn, looking bereft.
They had all just lost their jobs. Their town had just lost one of its largest employers. And the residents — many of whom are poor— had lost their access to emergency medical care. What would happen to all of them now? Would local residents’ health grow worse? Would some of them die preventable deaths?
These are questions that elected officials and policymakers may soon be confronting in rural communities across California and the nation. Cuts to Medicaid funding and the Affordable Care Act are likely rolling down from Washington, D.C., and hitting small hospitals already teetering at the brink of financial collapse. Even before these cuts hit, a 2022 study found that half of the hospitals in California were operating in the red. Already this fall: Palo Verde Hospital in Blythe filed for bankruptcy and Southern Inyo Hospital in Lone Pine sought emergency funds.
But things could get far worse: A June analysis released by four Democrats in the U.S. Senate found that many more hospitals in California could be at risk of closure in the face of federal healthcare cuts.
“It’s like the beginning of a tidal wave,” said Peggy Wheeler, vice president of policy of the California Hospital Assn. “I’m concerned we will lose a number of rural hospitals, and then the whole system may be at risk.”
1. Medical assistant Kylee Lutz, 26, right, hugs activities coordinator Rita Robledo on closing day. Lutz, who will continue to work in the clinic that remains open, said through tears, “It’s not going to be the same without you ladies.” 2. Rose Mary Wampler, 88, sees physician assistant Chris Pilaczynski at the clinic. Wampler, who lives alone across the street from Glenn Medical Center, said, “Old people can’t drive far away. I’m all by myself, I would just dial 9-1-1.”
Glenn Medical’s financing did not collapse because of the new federal cuts. Rather, the hospital was done in by a federal decision this year to strip the hospital’s “critical access” designation, which enabled it to receive increased federal reimbursement. The hospital, the only one in Glenn County, is just 32 miles from the nearest neighboring hospital under a route mapped by federal officials — less than the 35 miles required under the law. Though that distance hasn’t changed, the federal government has now decided to enforce its rules.
Local elected officials and hospital administrators fought for months to convince the federal government to grant them an exception. Now, with the doors closed, policy experts and residents of Willows said they are terrified by the potential consequences.
“People are going to die,” predicted Glenn County Supervisor Monica Rossman. She said she feared that older people in her community without access to transportation will put off seeking care until it is too late, while people of all ages facing emergency situations won’t be able to get help in time.

Kellie Amaru, a licensed vocational nurse who has worked at Glenn Medical Center for four years, reacts after watching a co-worker leave after working their final shift at the hospital.
But even for people who don’t face a life-or-death consequence, the hospital’s closure is still a body blow, said Willows Vice Mayor Rick Thomas. He and others predicted many people will put off routine medical care, worsening their health. And then there’s the economic health of the town.
Willows, which sits just east of I-5 in the center of the Sacramento Valley, has a proud history stretching back nearly 150 years in a farm region that now grows rice, almonds and walnuts. About 6,000 people live in the town, which has an economic development webpage featuring images of a tractor, a duck and a pair of hunters standing in the tall grass.
“We’ve lost 150 jobs already from the hospital [closing],” Thomas said. “I’m very worried about what it means. A hospital is good for new business. And it’s been hard enough to attract new business to the town.”
Dismantling ‘a legacy of rural healthcare’
From the day it started taking patients on Nov. 21,1950, Glenn General Hospital (as it was then called) was celebrated not just for its role in bringing medical care to the little farm town, but also for its role in helping Willows grow and prosper.
“It was quite state-of-the-art back in 1950,” said Lauren Still, the hospital’s chief administrative officer.
When the hospital’s first baby was born a few days later — little Glenda May Nieheus clocked in at a robust 8 pounds, 11 ounces — the arrival was celebrated on the front page of the Willows Daily Journal.
But as a small hospital in a small town, the institution struggled almost immediately. Within a few years, according to a 1957 story in the local newspaper, the hospital was already grappling with the problem of nurses leaving in droves for higher-paying positions elsewhere. A story the following year revealed that hospital administrators were forcing a maintenance worker to step in as an ambulance driver on weekends — without the requisite chauffeur’s license — to save money.
In a sign of how small the town is, that driver was Still’s boyfriend’s grandfather.
1. A customer walks into Willows Hardware store. 2. Cheerleaders perform during Willows High School’s Homecoming JV football game against Durham at Willows High School. 3. The press box at Willows High School’s football field is decorated with previous Northern Section CIF Championship wins.
Still, the institution endured, its grassy campus and low-slung wings perched proudly on the east end of town. Generations of the town’s babies were born there. As they grew up, they went into the emergency room for X-rays, stitches and treatment for fevers and infections. Their parents and grandparents convalesced there and sometimes died there, cared for by nurses who were part of the community.
“They saved my brother’s life. They saved my dad’s life,” said Keith Long, 34, who works at Red 88, an Asian fusion restaurant in downtown Willows that is a popular lunch spot for hospital staff.
Glenn Medical’s finances, however, often faltered. Experts in healthcare economics say rural hospitals like Glenn Medical generally have fewer patients than suburban and urban communities, and those patients tend to be older and sicker, meaning they are more expensive to treat. What’s more, a higher share of those patients are low-income and enrolled in Medi-Cal and Medicare, which generally has lower reimbursement rates than private insurance. Smaller hospitals also cannot take advantage of economies of scale the way bigger institutions can, nor can they bring the same muscle to negotiations for higher rates with private insurance companies.
For more than two decades across California, rural hospitals have been running out of money and closing their doors.

T-Ann Pearce, who has worked at Glenn Medical Center for six years, sits in the medical surgical unit during one of her last shifts with only a few remaining patients left to care.
In 2000, Glenn Medical went bankrupt, but was saved when it was awarded the “critical access” designation by the federal government that allowed it to receive higher reimbursement rates, Still said.
But by late 2017, the hospital was in trouble again.
A private for-profit company, American Advanced Management, swooped in to rescue Glenn Medical and a nearby hospital in Colusa County, buying them and keeping them open. The Modesto-based company specializes in buying distressed rural hospitals and now operates 14 hospitals in California, Utah and Texas.
The hospital set about building back its staff and improving its reputation for patient care in the community, which had been tarnished in part by the 2013 death of a young mother and her unborn baby.
“We’ve been on an upswing,” Still said, noting that indicators of quality of care and patient satisfaction have risen dramatically in recent years.
Then came the letter from the federal Centers for Medicare & Medicaid Services. On April 23, the federal agency wrote Glenn Medical’s management company with bad news: A recent review had found that Glenn Medical was “in noncompliance” with “distance requirements.” In plain English, federal officials had looked at a map and determined that Glenn Medical was not 35 miles from the nearest hospital by so-called main roads as required by law — it was just 32. Nor was it 15 miles by secondary roads. The hospital was going to lose its critical access designation. The hit to the hospital’s budget would be about 40% of its $28 million in net revenue. It could not survive that cut.
At first, hospital officials said they weren’t too worried.
“We thought, there’s no way they’re going to close down hospitals” over a few miles of road, Still, the hospital’s chief executive, said.
Especially, Still said, because it appeared there were numerous California hospitals in the same pickle. A 2013 federal inspector general’s report found that a majority of the 1,300 critical access hospitals in the country do not meet the distance requirement. That includes dozens in California.
Still and other hospital officials flew to Washington to make their case, sure that when they explained that one of the so-called main roads that connects Glenn Medical to its nearest hospital wasn’t actually one at all, and often flooded in the winter, the problem would be solved. The route everyone actually used, she said, was 35.7 miles.
“No roads have changed. No facilities have moved,” administrators wrote to federal officials. “And yet this CMS decision now threatens to dismantle a legacy of rural health care stability.”
Without it, the administrator wrote, “lives will be lost for certain.”
But, Still said, their protestations fell on deaf ears.
In August came the final blow: Glenn Medical would lose its critical access funding by April 2026.
The news set off a panic not just in Glenn County but at hospitals around the state.
1. A bicyclist passes by Glenn Medical Center. First opened to patients on November 21, 1950, the center was called Glenn General Hospital then. 2. A member of the staff signs a farewell board on closing day at Glenn Medical Center on October 21, 2025.
At least three other hospitals got letters from the Centers for Medicare & Medicaid saying their status was under review, Wheeler said: Bear Valley Community Hospital in Big Bear Lake, George L. Mee Memorial in Monterey County and Santa Ynez Valley Cottage Hospital in Solvang. The hospitals in Monterey and Big Bear Lake provided data demonstrating they met the requirements for the critical access status.
Cottage Hospital, however, did not, despite showing that access in and out of the area where the hospital is located was sometimes blocked by wildfires or rockslides.
Cottage Hospital officials did not respond to questions about what that might mean for their facility.
Asked about these situations, officials at the Centers for Medicare & Medicaid said the law does not give the agency flexibility to consider factors such as weather, for example, in designating a critical assess hospital. They added the hospital must demonstrate there is no driving route that would make it ineligible based on driving distances included in the statute.
Jeff Griffiths, a county supervisor in Inyo County who is also the president of the California Assn. of Counties, said he has been following the grim hospital financing news around the state with mounting worry.
The hospital in his county, Southern Inyo, came close to running out of money earlier this year, he said, and with more federal cuts looming, “I don’t know how you can expect these hospitals to survive.”
“It’s terrifying for our area,” Griffiths said, noting that Inyo County, which sits on the eastern side of the Sierra, has no easy access to any medical care on the other side of the giant mountain peaks.
‘This is the final call’
In Willows, once word got out that the hospital would lose its funding, nurses began looking for new jobs.
By late summer, so many people had left that administrators realized they had no choice but to shutter the emergency room, which closed Sept. 30.

Helena Griffith, 62, one of the last patients, waves goodbye as patient transport Jolene Guerra pushes her wheelchair down the hallway on October 20, 2025.
Through it all, McNabb, the 74-year-old patient receiving intravenous antibiotics, remained in her bed, getting to know the nurses who buzzed around her.
She became aware that when they weren’t caring for her, many of them were trying to figure out what they would do with their lives once they lost their jobs.
On the hospital’s last day, nurse Amanda Shelton gifted McNabb a new sweater to wear home.
When McNabb gushed over the sweetness of the gesture, Shelton teared up. “It’s not every day that it will be the last patient I’ll ever have,” she told her.
As McNabb continued to gather her things, Shelton retreated to the hospital’s recreation room, where patients used to gather for games or conversation.
With all the patients save McNabb gone, Shelton and some other hospital staff took up a game of dominoes, the trash talk of the game peppered with bittersweet remembrances of their time working in the creaky old building.

Registered nurse Ronald Loewen, 74, looks out the window on closing day at Glenn Medical Center on October 21, 2025. Loewen, who grew up and attended school in Willows, had four children delivered at Glenn Medical, two of them survived, and took care of former classmates at this hospital, says the hospital closing is, “a piece of our history gone.”
Shelton said she is not sure what is next for her. She loved Glenn Medical, she said, because of its community feel. Many people came for long stays or were frequent patients, and the staff was able to get to know them — and to feel like they were healing them.
“You got to know people. You got to know their family, or if they didn’t have any family,” you knew that too, she said. She added that in many hospitals, being a nurse can feel like being an extension of a computer. But at Glenn Medical, she said, “you actually got to look in someone’s eyes.”
The building itself was in dire shape, she noted. Nothing was up to modern code. It didn’t have central air conditioning, and it was heated by an old-fashioned boiler. “I mean, I have never even heard of a boiler room” before coming to work there, she said.
And yet within the walls, she said, “It’s community.”
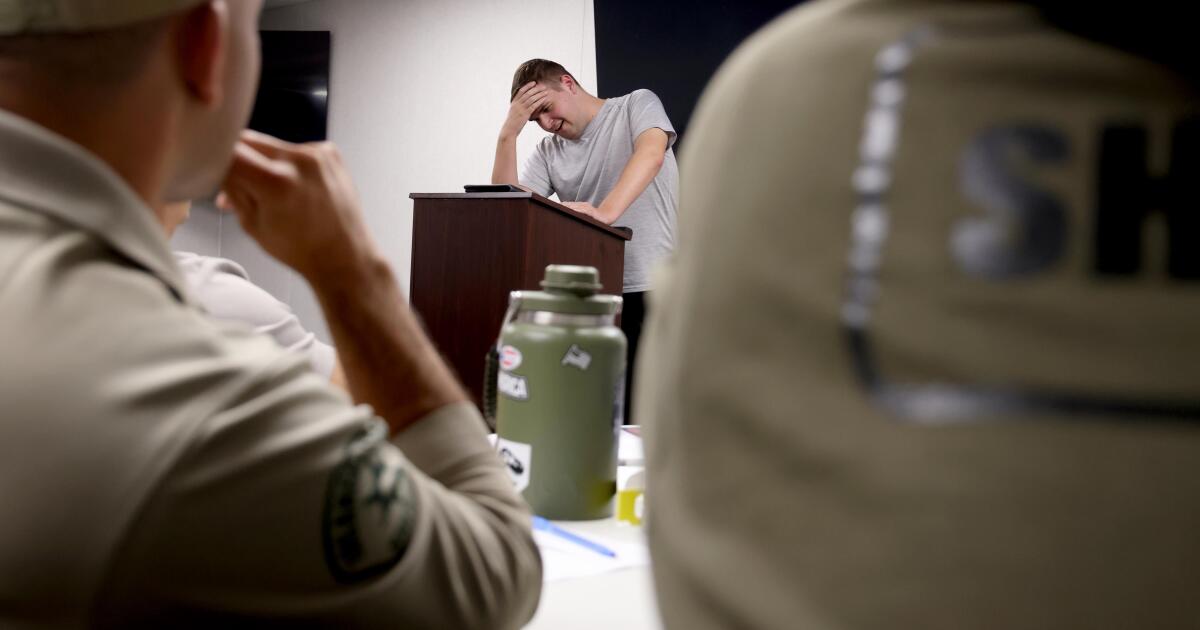
Bradley Ford, the emergency room manager, said he felt the same way and was determined to pay tribute to all the people who had made it so.
At 7 p.m. on the emergency room’s last night of service, Ford picked up his microphone and beamed his voice out to the hospital and to all the ambulances, fire trucks and others tuned to the signal.
He had practiced his speech enough times that he thought he could get through it without crying — although during his rehearsals he had never yet managed it.
“This is the final call,” Ford said. “‘After 76 years of dedicated service, the doors are closing. Service is ending. On behalf of all the physicians, nurses and staff who have walked these halls, it is with heavy hearts that we mark the end of this chapter.”
Nurses and other staff members recorded a video of Ford making his announcement, and passed it among themselves, tearing up every time they listened to it.
In an interview after the hospital had closed, Ford said he was one of the lucky ones: He had found a new job.
It was close enough to his home in Willows that he could commute — although Ford said he wasn’t sure how long he would remain in his beloved little town without access to emergency medical care there.

Rose Mary Wampler, 88, waits to have blood drawn at the lab beside a cordoning off, signaling the closure of the hospital side of Glenn Medical Center, on October 22, 2025. Wampler lives alone across the street from the hospital.
Rose Mary Wampler, 88, has lived in Willows since 1954 and now resides in a little house across the street from the hospital. Her three children were born at Glenn Medical, and Wampler herself was a patient there for two months last year when she was stricken with pneumonia and internal bleeding. She said she was fearful of the idea of driving more than 30 miles for healthcare elsewhere.
She looked out her window on a recent afternoon at the now-shuttered hospital.
“It looks like somebody just shut off the whole city, there’s nowhere to go get help,” she said.

Glenn Medical Center patient Richard Putnam, 86, closes the window in his hospital room. A month shy of it’s 75th year, the hospital closed on Oct 21, 2025.
(Christina House/Los Angeles Times)
Times photographer Christina House contributed to this report.

Science
Diablo Canyon clears last California permit hurdle to keep running

Central Coast Water authorities approved waste discharge permits for Diablo Canyon nuclear plant Thursday, making it nearly certain it will remain running through 2030, and potentially through 2045.
The Pacific Gas & Electric-owned plant was originally supposed to shut down in 2025, but lawmakers extended that deadline by five years in 2022, fearing power shortages if a plant that provides about 9 percent the state’s electricity were to shut off.
In December, Diablo Canyon received a key permit from the California Coastal Commission through an agreement that involved PG&E giving up about 12,000 acres of nearby land for conservation in exchange for the loss of marine life caused by the plant’s operations.
Today’s 6-0 vote by the Central Coast Regional Water Board approved PG&E’s plans to limit discharges of pollutants into the water and continue to run its “once-through cooling system.” The cooling technology flushes ocean water through the plant to absorb heat and discharges it, killing what the Coastal Commission estimated to be two billion fish each year.
The board also granted the plant a certification under the Clean Water Act, the last state regulatory hurdle the facility needed to clear before the federal Nuclear Regulatory Commission (NRC) is allowed to renew its permit through 2045.
The new regional water board permit made several changes since the last one was issued in 1990. One was a first-time limit on the chemical tributyltin-10, a toxic, internationally-banned compound added to paint to prevent organisms from growing on ship hulls.
Additional changes stemmed from a 2025 Supreme Court ruling that said if pollutant permits like this one impose specific water quality requirements, they must also specify how to meet them.
The plant’s biggest water quality impact is the heated water it discharges into the ocean, and that part of the permit remains unchanged. Radioactive waste from the plant is regulated not by the state but by the NRC.
California state law only allows the plant to remain open to 2030, but some lawmakers and regulators have already expressed interest in another extension given growing electricity demand and the plant’s role in providing carbon-free power to the grid.
Some board members raised concerns about granting a certification that would allow the NRC to reauthorize the plant’s permits through 2045.
“There’s every reason to think the California entities responsible for making the decision about continuing operation, namely the California [Independent System Operator] and the Energy Commission, all of them are sort of leaning toward continuing to operate this facility,” said boardmember Dominic Roques. “I’d like us to be consistent with state law at least, and imply that we are consistent with ending operation at five years.”
Other board members noted that regulators could revisit the permits in five years or sooner if state and federal laws changes, and the board ultimately approved the permit.
Science
Deadly bird flu found in California elephant seals for the first time

The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa Cruz announced Wednesday.
The virus has ravaged wild, commercial and domestic animals across the globe and was found last week in seven weaned pups. The confirmation came from the U.S. Department of Agriculture’s National Veterinary Services Laboratory in Ames, Iowa.
“This is exceptionally rapid detection of an outbreak in free-ranging marine mammals,” said Professor Christine Johnson, director of the Institute for Pandemic Insights at UC Davis’ Weill School of Veterinary Medicine. “We have most likely identified the very first cases here because of coordinated teams that have been on high alert with active surveillance for this disease for some time.”
Since last week, when researchers began noticing neurological and respoiratory signs of the disease in some animals, 30 seals have died, said Roxanne Beltran, a professor of ecology and evolutionary biology at UC Santa Cruz. Twenty-nine were weaned pups and the other was an adult male. The team has so far confirmed the virus in only seven of the dead pups.
Infected animals often have tremors convulsions, seizures and muscle weakness, Johnson said.
Beltran said teams from UC Santa Cruz, UC Davis and California State Parks monitor the animals 260 days of the year, “including every day from December 15 to March 1” when the animals typically come ashore to breed, give birth and nurse.
The concerning behavior and deaths were first noticed Feb. 19.
“This is one of the most well-studied elephant seal colonies on the planet,” she said. “We know the seals so well that it’s very obvious to us when something is abnormal. And so my team was out that morning and we observed abnormal behaviors in seals and increased mortality that we had not seen the day before in those exact same locations. So we were very confident that we caught the beginning of this outbreak.”
In late 2022, the virus decimated southern elephant seal populations in South America and several sub-Antarctic Islands. At some colonies in Argentina, 97% of pups died, while on South Georgia Island, researchers reported a 47% decline in breeding females between 2022 and 2024. Researchers believe tens of thousands of animals died.
More than 30,000 sea lions in Peru and Chile died between 2022 and 2024. In Argentina, roughly 1,300 sea lions and fur seals perished.
At the time, researchers were not sure why northern Pacific populations were not infected, but suspected previous or milder strains of the virus conferred some immunity.
The virus is better known in the U.S. for sweeping through the nation’s dairy herds, where it infected dozens of dairy workers, millions of cows and thousands of wild, feral and domestic mammals. It’s also been found in wild birds and killed millions of commercial chickens, geese and ducks.
Two Americans have died from the virus since 2024, and 71 have been infected. The vast majority were dairy or commercial poultry workers. One death was that of a Louisiana man who had underlying conditions and was believed to have been exposed via backyard poultry or wild birds.
Scientists at UC Santa Cruz and UC Davis increased their surveillance of the elephant seals in Año Nuevo in recent years. The catastrophic effect of the disease prompted worry that it would spread to California elephant seals, said Beltran, whose lab leads UC Santa Cruz’s northern elephant seal research program at Año Nuevo.
Johnson, the UC Davis researcher, said the team has been working with stranding networks across the Pacific region for several years — sampling the tissue of birds, elephant seals and other marine mammals. They have not seen the virus in other California marine mammals. Two previous outbreaks of bird flu in U.S. marine mammals occurred in Maine in 2022 and Washington in 2023, affecting gray and harbor seals.
The virus in the animals has not yet been fully sequenced, so it’s unclear how the animals were exposed.
“We think the transmission is actually from dead and dying sea birds” living among the sea lions, Johnson said. “But we’ll certainly be investigating if there’s any mammal-to-mammal transmission.”
Genetic sequencing from southern elephant seal populations in Argentina suggested that version of the virus had acquired mutations that allowed it to pass between mammals.
The H5N1 virus was first detected in geese in China in 1996. Since then it has spread across the globe, reaching North America in 2021. The only continent where it has not been detected is Oceania.
Año Nuevo State Park, just north of Santa Cruz, is home to a colony of some 5,000 elephant seals during the winter breeding season. About 1,350 seals were on the beach when the outbreak began. Other large California colonies are located at Piedras Blancas and Point Reyes National Sea Shore. Most of those animals — roughly 900 — are weaned pups.
It’s “important to keep this in context. So far, avian influenza has affected only a small proportion of the weaned at this time, and there are still thousands of apparently healthy animals in the population,” Beltran said in a press conference.
Public access to the park has been closed and guided elephant seal tours canceled.
Health and wildlife officials urge beachgoers to keep a safe distance from wildlife and keep dogs leashed because the virus is contagious.
Science
When slowing down can save a life: Training L.A. law enforcement to understand autism
Kate Movius moved among a roomful of Los Angeles County sheriff’s deputies, passing out a pop trivia quiz and paper prism glasses.
She told them to put on the vision-distorting glasses, and to write with their nondominant hand. As they filled out the tests, Movius moved about the City of Industry classroom pounding abruptly on tables. Then came the cowbell. An aide flashed the overhead lights on and off at random. The goal was to help the deputies understand the feeling of sensory overwhelm, which many autistic people experience when incoming stimulation exceeds their capacity to process.
“So what can you do to assist somebody, or de-escalate somebody, or get information from someone who suffers from a sensory disorder?” Movius asked the rattled crowd afterward. “We can minimize sensory input. … That might be the difference between them being able to stay calm and them taking off.”
Movius, founder of the consultancy Autism Interaction Solutions, is one of a growing number of people around the U.S. working to teach law enforcement agencies to recognize autistic behaviors and ensure that encounters between neurodevelopmentally disabled people and law enforcement end safely.
She and City of Industry Mayor Cory Moss later passed out bags filled with tools donated by the city to aid interactions: a pair of noise-damping headphones to decrease auditory input, a whiteboard, a set of communication cards with words and images to point to, fidget toys to calm and distract.
“The thing about autistic behavior when it comes to law enforcement is a lot of it may look suspicious, and a lot of it may feel very disrespectful,” said Movius, who is also the parent of an autistic 25-year-old man. Responding officers, she said, “are not coming in thinking, ‘Could this be a developmentally disabled person?’ I would love for them to have that in the back of their minds.”
A sheriff’s deputy reads a pamphlet on autism during the training program.
(Genaro Molina / Los Angeles Times)
Autism spectrum disorder is a developmental condition that manifests differently in nearly every person who has it. Symptoms cluster around difficulties in communication, social interaction and sensory processing.
An autistic person stopped by police might hold the officer’s gaze intensely or not look at them at all. They may repeat a phrase from a movie, repeat the officer’s question or temporarily lose their ability to speak. They might flee.
All are common involuntary responses for an autistic person in a stressful situation, which a sudden encounter with law enforcement almost invariably is. To someone unfamiliar with the condition, all could be mistaken for intoxication, defiance or guilt.
Autism rates in the U.S. have increased nearly fivefold since the Centers for Disease Control began tracking diagnoses in 2000, a rise experts attribute to broadening diagnostic criteria and better efforts to identify children who have the condition.
The CDC now estimates that 1 in 31 U.S. 8-year-olds is autistic. In California, the rate is closer to 1 in 22 children.
As diverse as the autistic population is, people across the spectrum are more likely to be stopped by law enforcement than neurotypical peers.
About 15% of all people in the U.S. ages 18 to 24 have been stopped by police at some point in their lives, according to federal data. While the government doesn’t track encounters for disabled people specifically, a separate study found that 20% of autistic people ages 21 to 25 have been stopped, often after a report or officer observation of a person behaving unusually.
Some of these encounters have ended in tragedy.
In 2021, Los Angeles County sheriff’s deputies shot and permanently paralyzed a deaf autistic man after family members called 911 for help getting him to a hospital.
Isaias Cervantes, 25, had become distressed about a shopping trip and started pushing his mother, his family’s attorney said at the time. He resisted as two deputies attempted to handcuff him and one of the deputies shot him, according to a county report.
In 2024, Ryan Gainer’s family called 911 for support when the 15-year-old became agitated. Responding San Bernardino County sheriff‘s deputies shot and killed him outside his Apple Valley home.
Last year, police in Pocatello, Idaho, shot Victor Perez, 17, through a chain-link fence after the nonspeaking teenager did not heed their shouted commands. He died from his injuries in April.

Sheriff’s deputies take a trivia quiz using their non-writing hands, while wearing vision-distorting glasses, as Kate Movius, standing left, and Industry Mayor Cory Moss, right, ring cowbells. The idea was to help them understand the sensory overwhelm some autistic people experience.
(Genaro Molina / Los Angeles Times)
As early as 2001, the FBI published a bulletin on police officers’ need to adjust their approach when interacting with autistic people.
“Officers should not interpret an autistic individual’s failure to respond to orders or questions as a lack of cooperation or as a reason for increased force,” the bulletin stated. “They also need to recognize that individuals with autism often confess to crimes that they did not commit or may respond to the last choice in a sequence presented in a question.”
But a review of multiple studies last year by Chapman University researchers found that while up to 60% of officers have been on a call involving an autistic person, only 5% to 40% had received any training on autism.
In response, universities, nonprofits and private consultants across the U.S. have developed curricula for law enforcement on how to recognize autistic behaviors and adapt accordingly.
The primary goal, Movius told deputies at November’s training session, is to slow interactions down to the greatest extent possible. Many autistic people require additional time to process auditory input and verbal responses, particularly in unfamiliar circumstances.
If at all possible, Movius said, wait 20 seconds for a response after asking a question. It may feel unnaturally long, she acknowledged. But every additional question or instruction fired in that time — what’s your name? Did you hear me? Look at me. What’s your name? — just decreases the likelihood that a person struggling to process will be able to respond at all.
Moss’ son, Brayden, then 17, was one of several teenagers and young adults with autism who spoke or wrote statements to be read to the deputies. The diversity of their speech patterns and physical mannerisms showed the breadth of the spectrum. Some were fluently verbal, while others communicated through signs and notes.
“This population is so diverse. It is so complicated. But if there’s anything that we can show [deputies] in here that will make them stop and think, ‘Hey, what if this is autism?’ … it is saving lives,” Moss said.

Mayor Cory Moss, left, and Kate Movius hug at the end of the training program last November. Movius started Autism Interaction Solutions after her son was born with profound autism.
(Genaro Molina / Los Angeles Times)
Some disability advocates cautioned that it takes more than isolated training sessions to ensure encounters end safely.
Judy Mark, co-founder and president of the nonprofit Disability Voices United, says she trained thousands of officers on safe autism interactions but stopped after Cervantes’ shooting. She now urges families concerned about an autistic child’s safety to call an ambulance rather than law enforcement.
“I have significant concern about these training sessions,” Mark said. “People get comfort from it, and the Sheriff’s Department can check the box.”
While not a panacea, supporters argue that a brief course is better than no preparation at all. Some years ago, Movius received a letter from a man whose profoundly autistic son slipped away as the family loaded their car at the beach. He opened the unlocked door of a police vehicle, climbed into the back and began to flail in distress.
Though surprised, the officer seated at the wheel de-escalated the situation and helped the young man find his family, the father wrote to Movius. He had just been to her training.
-

 World2 days ago
World2 days agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts2 days ago
Massachusetts2 days agoMother and daughter injured in Taunton house explosion
-

 Montana1 week ago
Montana1 week ago2026 MHSA Montana Wrestling State Championship Brackets And Results – FloWrestling
-

 Oklahoma1 week ago
Oklahoma1 week agoWildfires rage in Oklahoma as thousands urged to evacuate a small city
-

 Louisiana5 days ago
Louisiana5 days agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Denver, CO2 days ago
Denver, CO2 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Technology6 days ago
Technology6 days agoYouTube TV billing scam emails are hitting inboxes
-

 Technology6 days ago
Technology6 days agoStellantis is in a crisis of its own making



























