Science
NASA Spacecraft Smashed Asteroid Into New Orbit in Planetary Defense Test

Final month, NASA took goal at an asteroid, and on Tuesday, the area company introduced that its deliberate 14,000-mile-per-hour collision with an object named Dimorphos was extra profitable than it anticipated.
“We carried out humanity’s first planetary protection check,” mentioned Invoice Nelson, the administrator of NASA, throughout a brand new convention, “and we confirmed the world that NASA is severe as a defender of this planet.”
In November 2021, NASA launched the DART mission, sending a refrigerator-size spacecraft towards a small asteroid. Scientists created the DART spacecraft solely to destroy it. On Sept. 26, they despatched the spacecraft smashing right into a small asteroid, aiming to regulate its orbit in a check of a technique that would defend the planet from incoming asteroids or comets. One small shift in an area rock’s trajectory might, sometime, imply one big sigh of aid for humankind if it pushes an asteroid off a collision course with Earth.
The mission’s goal, Dimorphos, was a diminutive area rock, simply greater than 500 ft huge. It was and nonetheless is innocent, posing no threat to Earth. Earlier than DART’s impression, Dimorphos orbited a bigger asteroid referred to as Didymos each 11 hours and 55 minutes.
The spacecraft not solely related with Dimorphos on Sept. 26, it altered the area rock’s orbit, shortening its journey round a bigger asteroid by 32 minutes.
That point interval is what the DART mission aimed to alter. Scientists hoped the collision would push Dimorphos nearer to Didymos and velocity up its orbit, they usually have been crunching knowledge and taking extra observations of the double-asteroid system to know how efficient this specific protection mechanism was. In response to Mr. Nelson, scientists would have thought of DART an enormous success even when it had solely shortened Dimorphos’s orbit by 10 minutes. The fact — round thrice that shift — delighted the crew that managed the mission.
“If an Earth-threatening asteroid was found, and we might see it far sufficient away, this method might be used to deflect it,” Mr. Nelson mentioned.
It is a creating story. Please examine again for updates.

Science
Union presses California’s key bird flu testing lab for records

The union representing workers at a UC Davis lab that tests and tracks bird flu infections in livestock has sued the university, demanding that records showing staffing levels and other information about the lab’s operations be released to the public.
Workers in the lab’s small biotechnology department had raised concerns late last year about short staffing and potentially bungled testing procedures as cases of avian flu spread through millions of birds in turkey farms and chicken and egg-laying facilities, as well as through the state’s cattle herds.
The University Professional and Technical Employees-CWA Local 9119 said that it requested records in December 2024 in an attempt to understand whether the lab was able to properly service the state’s agribusiness.
But UC Davis has refused to release records, in violation of California’s public records laws, the union alleged in a lawsuit recently filed in Alameda County Superior Court.
UC Davis spokesperson Bill Kisliuk declined to comment on the lawsuit’s specific allegations.
“The university looks forward to filing our response in court. We are grateful for the outstanding work of the CAHFS lab staff, including UPTE-represented workers, during the 2024 surge in avian flu testing,” Kisliuk said in an email.
UC Davis has previously denied that workplace issues have left the lab ill-equipped to handle bird flu testing. Kisliuk had said the facility “maintained the supervision, staffing and resources necessary to provide timely and vital health and safety information to those asking us to perform tests.”
According to copies of email correspondence cited in the lawsuit, UC Davis in January denied the union’s request for records regarding short staffing or testing errors, calling the request “unduly burdensome.” It also denied its request for information about farms and other businesses that had samples tested at the lab, citing an exemption to protect from an “invasion of personal privacy.”
Workers at the lab had previously told The Times that they observed lapses in quality assurance procedures, as well as other mistakes in the testing process.
Amy Fletcher, a UC Davis employee and president of the union’s Davis chapter, said the records would provide a necessary window into how staffing levels could be hurting farms and other businesses that rely on the lab for testing. Fletcher said workers have become afraid to speak about problems at the lab, having been warned by management that the some information related to testing is confidential.
The Davis lab is the only entity in the state with the authority to confirm bird flu cases.
The union, known as UPTE, represents about 20,000 researchers and other technical workers across the University of California system’s 10 campuses.
Science
Newsom's podcast sidekick: a single-use plastic water bottle

Johnny had Ed. Conan had Andy. And Gov. Gavin Newsom? A single-use plastic water bottle.
In most of the YouTube video recordings of Newsom’s new podcast, “This is Gavin Newsom,” a single-use plastic water bottle lurks on a table nearby.
Sometimes, it is accompanied by a single-use coffee cup. Other times, it stands alone.
Typically, such product placement would raise nary an eyebrow. But in recent weeks, environmentalists, waste advocates, lawmakers and others have been battling with the governor and his administration over a landmark single-use plastic law that Newsom signed in 2022, but which he has since worked to defang — reducing the number of packaged single-use products the law was designed to target and potentially opening the door for polluting forms of recycling.
Anti-plastic advocates say it’s an abrupt and disappointing pivot from the governor, who in June 2022, decried plastic pollution and the plague of single-use plastic on the environment.
“It’s like that whole French Laundry thing all over again,” said one anti-plastic advocate, who didn’t want to be identified for fear of angering the governor. Newsom was infamously caught dining without a mask at the wine country restaurant during the COVID-19 lockdown.
Newsom’s efforts to scale back SB 54, the state’s single-use plastic recycling law, has dismayed environmentalists who have long considered Newsom one of their staunchest allies.
“Our kids deserve a future free of plastic waste and all its dangerous impacts … No more,” Newsom said in 2022, when he signed SB 54. “California won’t tolerate plastic waste that’s filling our waterways and making it harder to breathe. We’re holding polluters responsible and cutting plastics at the source.”
Asked about the presence of the plastic water bottle, Daniel Villaseñor, the governor’s deputy director of communications, had this response:
“Are you really writing a story this baseless or should we highlight this video for your editor?” Villaseñor said via email, attaching a video clip showing this reporter seated near a plastic water bottle at last year’s Los Angeles Times’ Climate Summit. (The bottles were placed near chairs for all the panelists; this particular one was never touched.)
After this story was first published, the governor’s office said the plastic water bottles seen on the podcast were placed there by staff or production teams and not at Newsom’s request, and that the governor remains committed to seeing SB 54 implemented.
More than a half-dozen environmentalists and waste advocates asked to comment for this story declined to speak on the record, citing concerns including possible retribution from the governor’s office and appearing to look like scolds as negotiations over implementing SB 54 continue.
Dianna Cohen, the co-founder and chief executive of Plastic Pollution Coalition, said that while she wouldn’t comment on the governor and his plastic sidekick, she noted that plastic pollution is an “urgent global crisis” that requires strong policies and regulations.
“Individuals — especially those in the public eye — can help shift culture by modeling these solutions. We must all work to embrace the values we want to see and co-create a healthier world,” she said in a statement.
On Thursday, Newsom dropped a new episode of “This is Gavin Newsom” with independent journalist Aaron Parnas. In the video, there wasn’t a plastic bottle in sight.
Science
In Southern California, many are skipping healthcare out of fear of ICE operations

Missed childhood vaccinations. Skipped blood sugar checks. Medications abandoned at the pharmacy.
These are among the healthcare disruptions providers have noticed since Immigration and Customs Enforcement operations began in Southern California earlier this month.
Across the region, once-busy parks, shops and businesses have emptied as undocumented residents and their families hole up at home in fear. As rumors of immigration arrests have swirled around clinics and hospitals, many patients are also opting to skip chronic-care management visits as well as routine childhood check-ups.
In response, local federally qualified health centers — institutions that receive federal funds and are required by law to provide primary care regardless of ability to pay — have been scrambling to organize virtual appointments, house calls and pharmacy deliveries to patients who no longer feel safe going out in public.
“We’re just seeing a very frightening and chaotic environment that’s making it extremely difficult to provide for the healthcare needs of our patients,” said Jim Mangia, president of St. John’s Community Health, which offers medical, dental and mental health care to more than 100,000 low-income patients annually in Southern California.
Prior to the raids, the system’s network of clinics logged about a 9% no-show rate, Mangia said. In recent weeks, more than 30% of patients have canceled or failed to show. In response, the organization has launched a program called Healthcare Without Fear to provide virtual and home visits to patients concerned about the prospect of arrest.
“When we call patients back who missed their appointment and didn’t call in, overwhelmingly, they’re telling us they’re not coming out because of ICE,” said Mangia, who estimates that 25% of the clinic’s patient population is undocumented. “People are missing some pretty substantial healthcare appointments.”
A recent survey of patient no-shows at nonprofit health clinics across Los Angeles County found no universal trends across the 118 members of the Community Clinic Assn. of L.A. County, President Louise McCarthy said. Some clinics have seen a jump in missed appointments, while others have observed no change. The data do not indicate how many patients opted to convert scheduled in-person visits to telehealth so they wouldn’t have to leave home, she noted.
Patients have also expressed concerns that any usage of health services could make them targets. Earlier this month, the Associated Press reported that the U.S. Department of Health and Human Services shared the personal data of Medicaid enrollees with the U.S. Department of Homeland Security, including their immigration status. No specific enforcement actions have been directly linked to the data.
“The level of uncertainty and anxiety that is happening now is beyond the pale,” McCarthy said, for patients and staff alike.
County-run L.A. General Medical Center issued a statement on Thursday refuting reports that federal authorities had carried out enforcement operations at the downtown trauma center. While no immigration-related arrests have been reported at county health facilities, “the mere threat of immigration enforcement near any medical facility undermines public trust and jeopardizes community health,” the department said in a statement.
Los Angeles County is among the providers working to extend in-home care options such as medication delivery and a nurse advice line for people reluctant to come in person.
“However, not all medical appointments or conditions can be addressed remotely,” a spokesperson said. “We urge anyone in need of care not to delay.”
Providers expressed concern that missing preventative care appointments could lead to emergencies that both threaten patients’ lives and further stress public resources. Preventative care “keeps our community at large healthy and benefits really everyone in Los Angeles,” said a staff member at a group of L.A. area clinics. He asked that his employer not be named for fear of drawing attention to their patient population.
Neglecting care now, he said, “is going to cost everybody more money in the long run.”
A patient with hypertension who skips blood pressure monitoring appointments now may be more likely to be brought into an emergency room with a heart attack in the future, said Dr. Bukola Olusanya, a medical director at St. John’s.
“If [people] can’t get their medications, they can’t do follow-ups. That means a chronic condition that has been managed and well-controlled is just going to deteriorate,” she said. “We will see patients going to the ER more than they should be, rather than coming to primary care.”
Providers are already seeing that shift. When a health team visited one diabetic patient recently at home, they found her blood sugar levels sky-high, Mangia said. She told the team she’d consumed nothing but tortillas and coffee in the previous five days rather than risk a trip to the grocery store.
-

 Arizona4 days ago
Arizona4 days agoSuspect in Arizona Rangers' death killed by Missouri troopers
-

 News1 week ago
News1 week agoAt Least 4 Dead and 4 Missing in West Virginia Flash Flooding
-
 Movie Reviews1 week ago
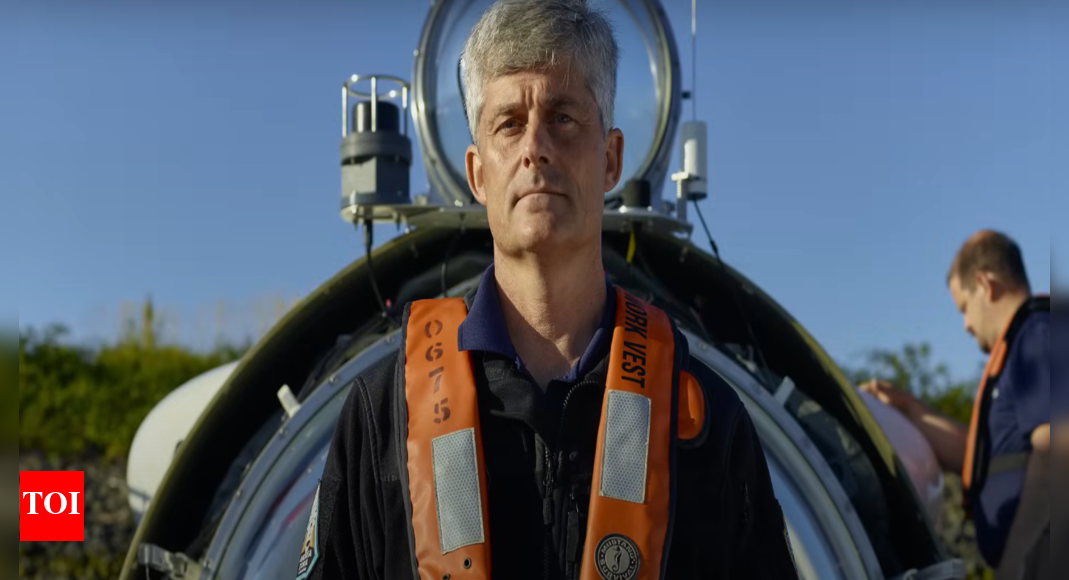
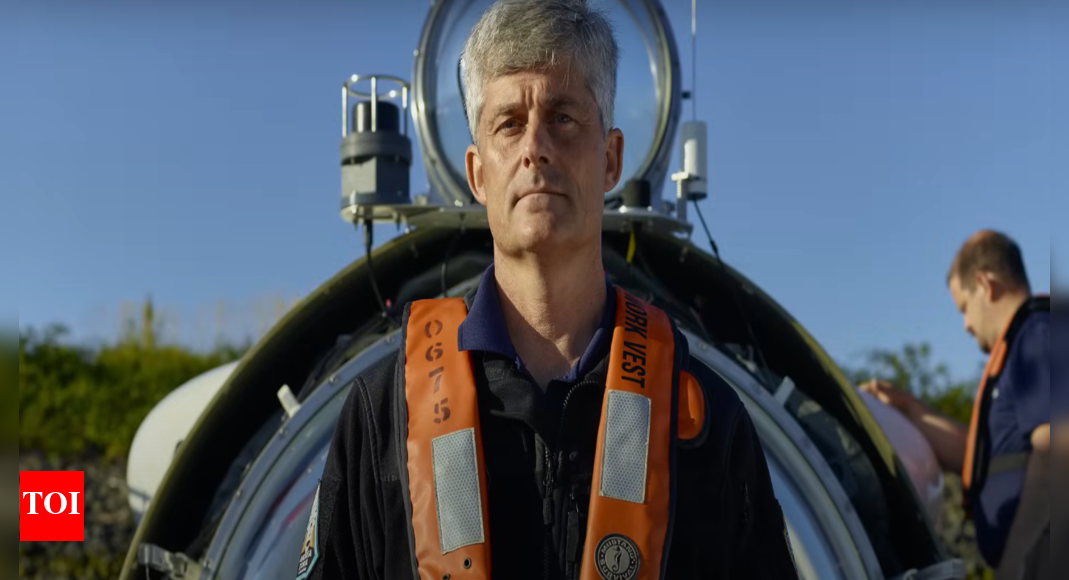
Movie Reviews1 week agoTitan: The OceanGate Disaster Movie Review: A sobering deep dive into ambition, negligence, and tragedy
-

 News1 week ago
News1 week ago‘No Kings’ demonstrators to gather across Greater Cincinnati in opposition to Trump
-

 News1 week ago
News1 week agoOakland County sheriff urging vigilance after shootings of 2 Minnesota lawmakers
-

 Culture1 week ago
Culture1 week agoBook Review: “The Möbius Book, by Catherine Lacey
-

 News1 week ago
News1 week agoHow Many Law Enforcement Agencies Are Involved in LA Immigration Protests?
-

 Health1 week ago
Health1 week agoHairstylists and medical expert confirm temporary hair loss affecting Ozempic users














