Science
It’s OK to mix and match COVID-19 booster shoots. Which one should I get?

Topping up your safety in opposition to extreme COVID-19 whereas avoiding the danger of uncommon vaccine unwanted effects shouldn’t be rocket science.
However simply ask the consultants who suggested federal regulators to authorize extra photographs: There’s no easy system to information People’ choices about booster photographs.
Whether or not you need to get a booster shot and which one you need to get is dependent upon who you might be, what medical vulnerabilities you’ve, and what vaccine you bought first. The folks you reside with or the type of work you do may additionally affect your selection.
After which there’s the deeply private matter of how a lot danger — of COVID-19 or of vaccine unwanted effects — you’re keen to just accept.
E-newsletter
Get our free Coronavirus Immediately e-newsletter
Join the newest information, greatest tales and what they imply for you, plus solutions to your questions.
You might often obtain promotional content material from the Los Angeles Instances.
Even when a vaccine’s safety has slipped with time, many absolutely vaccinated younger folks, or those that’ve had an an infection earlier than or after being vaccinated, can fairly determine that their chance of changing into very sick stays low.
The consultants who suggested the Facilities for Illness Management and Prevention this week made clear they weren’t recommending boosters for all; they had been recommending that thousands and thousands of people who find themselves absolutely vaccinated have entry to a booster shot if they need one.
A brand new authorities examine on mixing and matching vaccines has added extra choices — and thus extra complexity — to the difficulty of boosters.
The outcomes to this point are preliminary, and the individuals are nonetheless being tracked. However after a minimum of 12 weeks of follow-up, researchers haven’t detected any in poor health results in individuals who had been first inoculated with one COVID-19 vaccine after which received a booster shot of one other.
These reassuring findings led Dr. Rochelle Walensky, the CDC director, to go away the selection in sufferers’ arms.
“Some folks might have a choice for the vaccine kind that they initially acquired and others might want to get a distinct booster,” the company stated in new steering issued late Thursday. “CDC’s suggestions now permit for the sort of combine and match dosing for booster photographs.”
Now, along with asking your self whether or not you in reality want a booster, there’s the query of whether or not you need to hunt down a shot that’s totally different from the one you bought the primary time round. Right here’s what you need to be mindful as you determine.
Maximizing your increase
If you happen to’re seeking to maximize your immunity increase, you’re out of luck: The information are usually not but in to information your quest.
The brand new examine consists of three teams of 150 absolutely immunized folks — one which received the Pfizer-BioNTech vaccine, one which received the Moderna vaccine, and one which received the Johnson & Johnson shot. Researchers took every group and additional divided it into three arms, with 50 folks in every. Individuals in a single arm of every group received boosted with the identical product that they had initially gotten. Every group’s second and third arm received boosted with one or the opposite of the remaining vaccines approved to be used in the US.
It’s a novel and intelligent design. However at this level, not sufficient folks have been tracked for an extended sufficient time period for scientists to make significant comparisons between teams.
The examine’s early efforts to measure jumps in coronavirus-fighting antibodies confirmed that mixing was usually no worse than matching, and that it was typically higher.
With regard to the Johnson & Johnson vaccine particularly, the info recommend that those that received an preliminary J&J shot noticed their antibody ranges rise a bit extra after 15 days in the event that they had been boosted with the Pfizer-BioNTech or Moderna vaccine than in the event that they received a second dose of J&J.
When both the Pfizer or Moderna boosters had been used after any of the three major programs of vaccine, the increase in antibodies was about the identical.
Security issues, then, provide the most effective information for who ought to take into account mixing and matching.
Girls contemplating a J&J booster
By way of Oct. 13, vaccine security displays have detected 47 circumstances of a uncommon blood clotting dysfunction in individuals who received the single-dose J&J vaccine.
That’s a tiny fraction of 15.3 million doses of J&J vaccine administered. However the dysfunction — known as thrombosis with thrombocytopenia syndrome, or TTS — is life-threatening. 5 folks have died of the situation, which causes runaway clotting that could be very troublesome to deal with.
Three-quarters of J&J vaccine recipients who developed TTS had been ladies ages 18-49. 4 of the 5 who died had been ladies.
Exams which may predict an individual’s danger of creating TTS aren’t available. So ladies beneath 50 who need extra safety may take into account looking for out the Moderna or Pfizer-BioNTech vaccine for his or her booster shot.
Younger males who received a shot of Moderna or Pfizer-BioNTech
For each million younger males between 18 and 24 who received a second dose of one of many mRNA vaccines, security displays detected someplace between 37 and 39 circumstances of myocarditis or pericarditis — basically an irritation of the center muscle or its surrounding tissue.
The speed was highest amongst males beneath 21, however it was seen with reducing frequency in males as much as 29. (It was additionally seen in ladies, although far much less incessantly.) And it was barely greater in younger males who had been initially inoculated with the Moderna vaccine than in those that received Pfizer-BioNTech.
The situations had been way more frequent after the second dose than the primary. Some consultants concern a 3rd dose might additional escalate the danger.
Myocarditis and pericarditis are fairly uncommon unwanted effects, and in additional than three-quarters of circumstances, their signs — tightness, squeezing or ache within the chest — went away with time and over-the-counter medicine. However coronary heart irregularities have to be taken severely, and nobody actually is aware of if a bout of irritation can have long-term results.
To be secure, cardiologists usually advocate the cessation of strenuous train for 3 to 6 months after a case of both situation. If a younger male athlete who’d gotten one of many mRNA vaccines felt he wanted a 3rd shot, he may take into account getting the J&J booster, or possibly switching from Moderna to Pfizer-BioNTech.
These with a historical past of Guillain-Barré syndrome
Guillain-Barré syndrome, or GBS, is a response to an infection or vaccine by which the immune system assaults the nerves, typically inflicting paralysis that may final months.
The FDA’s hostile occasion monitoring system has picked up a minimum of 130 experiences of individuals throughout the age spectrum creating GBS after getting the J&J vaccine, however no rise amongst those that received mRNA vaccines. This week, the British authorities added a warning about uncommon circumstances of GBS following use of the COVID-19 vaccine made by AstraZeneca, which isn’t approved to be used within the U.S. however is comparable in design to the J&J vaccine.
Anybody with a private or household historical past of GBS who received the J&J vaccine ought to take into account switching to one of many mRNA vaccines as a booster, and may in all probability keep away from the J&J vaccine as a booster to an preliminary course of Pfizer or Moderna.

Science
FDA sets limits for lead in many baby foods as California disclosure law takes effect

The U.S. Food and Drug Administration this week set maximum levels for lead in baby foods such as jarred fruits and vegetables, yogurts and dry cereal, part of an effort to cut young kids’ exposure to the toxic metal that causes developmental and neurological problems.
The agency issued final guidance that it estimated could reduce lead exposure from processed baby foods by about 20% to 30%. The limits are voluntary, not mandatory, for food manufacturers, but they allow the FDA to take enforcement action if foods exceed the levels.
It’s part of the FDA’s ongoing effort to “reduce dietary exposure to contaminants, including lead, in foods to as low as possible over time, while maintaining access to nutritious foods,” the agency said in a statement.
Consumer advocates, who have long sought limits on lead in children’s foods, welcomed the guidance first proposed two years ago, but said it didn’t go far enough.
“FDA’s actions today are a step forward and will help protect children,” said Thomas Galligan, a scientist with the Center for Science in the Public Interest. “However, the agency took too long to act and ignored important public input that could have strengthened these standards.”
The new limits on lead for children younger than 2 don’t cover grain-based snacks such as puffs and teething biscuits, which some research has shown contain higher levels of lead. And they don’t limit other metals such as cadmium that have been detected in baby foods.
The FDA’s announcement comes just one week after a new California law took effect that requires baby food makers selling products in California to provide a QR code on their packaging to take consumers to monthly test results for the presence in their product of four heavy metals: lead, mercury, arsenic and cadmium.
The change, required under a law passed by the California Legislature in 2023, will affect consumers nationwide. Because companies are unlikely to create separate packaging for the California market, QR codes are likely to appear on products sold across the country, and consumers everywhere will be able to view the heavy metal concentrations.
Although companies are required to start printing new packaging and publishing test results of products manufactured beginning in January, it may take time for the products to hit grocery shelves.
The law was inspired by a 2021 congressional investigation that found dangerously high levels of heavy metals in packaged foods marketed for babies and toddlers. Baby foods and their ingredients had up to 91 times the arsenic level, up to 177 times the lead level, up to 69 times the cadmium level, and up to five times the mercury level that the U.S. allows to be present in bottled or drinking water, the investigation found.
There’s no safe level of lead exposure for children, according to the U.S. Centers for Disease Control and Prevention. The metal causes “well-documented health effects,” including brain and nervous system damage and slowed growth and development. However, lead occurs naturally in some foods and comes from pollutants in air, water and soil, which can make it impossible to eliminate entirely.
The FDA guidance sets a lead limit of 10 parts per billion for fruits, most vegetables, grain and meat mixtures, yogurts, custards and puddings and single-ingredient meats. It sets a limit of 20 parts per billion for single-ingredient root vegetables and for dry infant cereals. The guidance covers packaged processed foods sold in jars, pouches, tubs or boxes.
Jaclyn Bowen, executive director of the Clean Label Project, an organization that certifies baby foods as having low levels of toxic substances, said consumers can use the new FDA guidance in tandem with the new California law: The FDA, she said, has provided parents a “hard and fast number” to consider a benchmark when looking at the new monthly test results.
But Brian Ronholm, director of food policy for Consumer Reports, called the FDA limits “virtually meaningless because they’re based more on industry feasibility and not on what would best protect public health.” A product with a lead level of 10 parts per billion is “still too high for baby food. What we’ve heard from a lot of these manufacturers is they are testing well below that number.”
The new FDA guidance comes more than a year after lead-tainted pouches of apple cinnamon puree sickened more than 560 children in the U.S. between October 2023 and April 2024, according to the CDC.
The levels of lead detected in those products were more than 2,000 times higher than the FDA’s maximum. Officials stressed that the agency doesn’t need guidance to take action on foods that violate the law.
Aleccia writes for the Associated Press. Gold reports for The Times’ early childhood education initiative, focusing on the learning and development of California children from birth to age 5. For more information about the initiative and its philanthropic funders, go to latimes.com/earlyed.
Science
NASA punts Mars Sample Return decision to the next administration
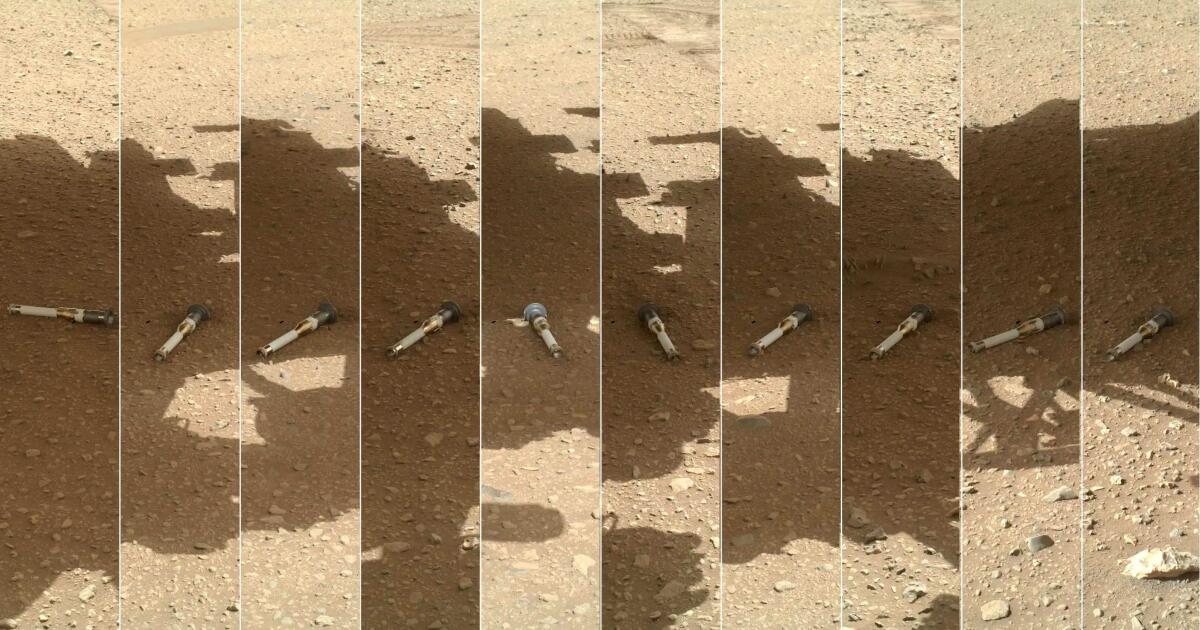
Anyone hoping for a clear path forward this year for NASA’s imperiled Mars Sample Return mission will have to wait a little longer.
The agency has settled on two potential strategies for the first effort to bring rock and soil from another planet back to Earth for study, NASA Administrator Bill Nelson said Tuesday: It can either leverage existing technology into a simpler, cheaper craft or turn to a commercial partner for a new design.
But the final decision on the mission’s structure — or whether it should proceed at all — “is going to be a function of the new administration,” Nelson said. President-elect Donald Trump will take office Jan. 20.
“I don’t think we want the only [Mars] sample return coming back on a Chinese spacecraft,” Nelson said, referencing a rival mission that Beijing has in the works. “I think that the [Trump] administration will certainly conclude that they want to proceed. So what we wanted to do was to give them the best possible options so that they can go from there.”
The call also contained words of encouragement for NASA’s Jet Propulsion Laboratory in La Cañada Flintridge, which leads the embattled mission’s engineering efforts.
“To put it really bluntly, JPL is our Mars center in NASA science,” said Nicky Fox, associate administrator of the Science Mission Directorate. “They are the people who landed us on Mars, together with our industry partners. So they will be moving forward, regardless of which path, with a key role in the Mars Sample Return.”
In April, after an independent review found “near zero probability” of Mars Sample Return making its proposed 2028 launch date, NASA put out a request for alternative proposals to all of its centers and the private sector. JPL was forced to compete for what had been its own project.
The independent review board determined that the original design would probably cost up to $11 billion and not return samples to Earth until at least 2040.
“That was just simply unacceptable,” said Nelson, who paused the mission in late 2023 to review its chances of success.
Ensuing cuts to the mission’s budget forced a series of layoffs at JPL, which let go of 855 employees and 100 on-site contractors in 2024.
The NASA-led option that Nelson suggested Tuesday includes several elements from the JPL proposal, according to a person who reviewed the documents. This leaner, simpler alternative will cost between $6.6 billion and $7.7 billion, and will return the samples by 2039, he said. A commercial alternative would probably cost $5.8 billion to $7.1 billion.
Nelson, a former Democratic U.S. senator from Florida, will step down as head of the space agency when Trump takes office. Trump has nominated as his successor Jared Isaacman, a tech billionaire who performed the first private space walk, who must be confirmed by the Senate.
NASA has not had any conversations with Trump’s transition team about Mars Sample Return, Nelson said. How the new administration will prioritize the project is not yet clear.
“It’s very uncertain how the new administration will go forward,” said Casey Dreier, chief of space policy for the Planetary Society, a Pasadena nonprofit that promotes space research. “Cancellation is obviously still on the table. … It’s hard to game this out.”
Planetary scientists have identified Mars Sample Return as their field’s highest priority in the last three decadal surveys, reports that the National Academies of Sciences, Engineering, and Medicine prepare every 10 years in order to advise NASA.
Successfully completing the mission is “key for the nation’s leadership in space science,” said Bethany L. Ehlmann, a planetary scientist at Caltech in Pasadena. “I hope the incoming administrator moves forward decisively to select a plan and execute. There are extraordinary engineers at JPL and NASA industry partners eager and able to get to work to make it happen.”
Science
Panama Canal’s Expansion Opened Routes for Fish to Relocate

Night fell as the two scientists got to work, unfurling long nets off the end of their boat. The jungle struck up its evening symphony: the sweet chittering of insects, the distant bellowing of monkeys, the occasional screech of a kite. Crocodiles lounged in the shallows, their eyes glinting when headlamps were shined their way.
Across the water, cargo ships made dark shapes as they slid between the seas.
The Panama Canal has for more than a century connected far-flung peoples and economies, making it an essential artery for global trade — and, in recent weeks, a target of President-elect Donald J. Trump’s expansionist designs.
But of late the canal has been linking something else, too: the immense ecosystems of the Atlantic and the Pacific.
The two oceans have been separated for some three million years, ever since the isthmus of Panama rose out of the water and split them. The canal cut a path through the continent, yet for decades only a handful of marine fish species managed to migrate through the waterway and the freshwater reservoir, Lake Gatún, that feeds its locks.
Then, in 2016, Panama expanded the canal to allow supersize ships, and all that started to change.
In less than a decade, fish from both oceans — snooks, jacks, snappers and more — have almost entirely displaced the freshwater species that were in the canal system before, scientists with the Smithsonian Tropical Research Institute in Panama have found. Fishermen around Lake Gatún who rely on those species, chiefly peacock bass and tilapia, say their catches are growing scarce.
Researchers now worry that more fish could start making their way through from one ocean to the other. And no potential invader causes more concern than the venomous, candy-striped lionfish. They are known to inhabit Panama’s Caribbean coast, but not the eastern Pacific. If they made it there through the canal, they could ravage the defenseless local fish, just as they’ve done in the Gulf of Mexico and the Caribbean.
Already, marine species are more than occasional visitors in Lake Gatún, said Phillip Sanchez, a fisheries ecologist with the Smithsonian. They’re “becoming the dominant community,” he said. They’re “pushing everything else out.”
-

 Business1 week ago
Business1 week agoThese are the top 7 issues facing the struggling restaurant industry in 2025
-

 Culture1 week ago
Culture1 week agoThe 25 worst losses in college football history, including Baylor’s 2024 entry at Colorado
-

 Sports1 week ago
Sports1 week agoThe top out-of-contract players available as free transfers: Kimmich, De Bruyne, Van Dijk…
-

 Politics6 days ago
Politics6 days agoNew Orleans attacker had 'remote detonator' for explosives in French Quarter, Biden says
-

 Politics5 days ago
Politics5 days agoCarter's judicial picks reshaped the federal bench across the country
-

 Politics4 days ago
Politics4 days agoWho Are the Recipients of the Presidential Medal of Freedom?
-

 Health3 days ago
Health3 days agoOzempic ‘microdosing’ is the new weight-loss trend: Should you try it?
-

 World1 week ago
World1 week agoIvory Coast says French troops to leave country after decades