Science
As fentanyl overdose deaths keep rising, efforts to reverse trend meet liability fears

As fentanyl overdose deaths rise unabated, California is on the forefront of the struggle to reverse the grim development. However organizations that distribute overdose reversal medicine fear that their more and more daring efforts to save lots of lives may land them in authorized hassle.
Some, reminiscent of an outside middle in San Francisco that opened in January, have generated broad consideration. The power — which along with distributing naloxone to opioid customers helped join them with social companies — drew criticism from residents who claimed it inspired drug abuse by permitting individuals to make use of on website. It closed earlier this month.
Different pioneering approaches have stayed principally out of the highlight. In a handful of main cities from Oakland to Los Angeles, plans are underway to increase how the reversal drug is distributed: outfitting residential buildings that home giant populations of opioid customers with bins of Narcan, the model title of the extensively used nasal spray model, along with making it obtainable in faculties, libraries and jails.
Elsewhere, service suppliers need authorized cowl to distribute naloxone to individuals who might in flip share it with others who haven’t been educated to manage it.
Homeless fentanyl person Brandice Josey, left, makes use of a straw to blow a puff of fentanyl smoke into the mouth of Ryan Smith, additionally homeless, in Los Angeles.
(Jae C. Hong / Related Press)
The initiatives are an indication of this determined second in America’s long-running overdose epidemic. The loss of life toll has spiked lately, largely because of the rising ubiquity of the highly effective opioid fentanyl.
The legally prescribed painkiller has change into a preferred illicit road drug over the past decade. It has additionally killed hundreds of people that unknowingly consumed different medicine reminiscent of cocaine or heroin that had been surreptitiously laced with fentanyl.
The U.S. Facilities for Illness Management and Prevention has described fentanyl as as much as 50 occasions as potent as heroin and 100 occasions as potent as morphine.
Greater than 71,000 individuals died within the U.S. of overdoses brought on by artificial opioids — primarily fentanyl — in 2021, a rise of greater than 23% from the earlier yr. In 2012, the CDC recorded simply 1,615 overdose deaths involving fentanyl within the U.S.
Within the face of such distressing failure to cut back deaths from opioids, strategies for addressing the disaster that many as soon as thought-about too dangerous and even unthinkable at the moment are being debated by state and native officers and rolled out in communities devastated by overdoses.
***
In San Luis Obispo County, a stretch of coastal California that’s residence to fewer than 300,000 individuals, the quantity who died yearly of opioid-related overdoses jumped from 21 to 55 between 2019 and 2020.

The overdose-reversal drug Narcan.
(Matt Rourke / Related Press)
At this time, each sheriff’s deputy within the county carries Narcan whereas on patrol. Anybody with a San Luis Obispo handle can get naloxone mailed to their residence free of charge by filling out a web-based kind and checking a field stating that they’ve accomplished a fundamental coaching course on easy methods to use the remedy.
However some advocates and officers say naloxone remains to be not prevalent sufficient within the communities that want it most. Many drug customers and their family members don’t know there are so few obstacles to acquiring opioid reversal medicine in California, and others merely haven’t sought it out.
Homeless individuals usually can’t receive naloxone by way of mail as a result of they don’t have any mounted handle. Language obstacles and worry of authority figures and legislation enforcement hold some individuals from searching for it out.
As government director of a San Luis Obispo County nonprofit known as the 5Cities Homeless Coalition, Janna Nichols has witnessed the lifesaving advantages of naloxone.
Earlier than her group saved Narcan available and she or he and her workers had been educated to manage it, Nichols stated, that they had no choice however to name 911 when shoppers exhibited overdose signs.
Nobody has died of an overdose on the nonprofit’s workplace in Grover Seashore, about 15 miles southeast of downtown San Luis Obispo. Nichols needs to maintain it that approach.
So now, when “someone is sitting within the foyer and clearly underneath the affect who’s torpid and nonresponsive,” she stated, 5Cities staffers administer Narcan as an alternative of ready for emergency responders.
Nonetheless, Nichols and her staffers aren’t there when individuals overdose at 3 a.m. in a darkish car parking zone, or at residence with mates or relations. So she’s searching for methods to assist.
She’d like to have the ability to give naloxone on to drug customers and encourage them to share it with others who could also be untrained. In an ideal world, she’d erect stands or bins containing naloxone — she likened them to “Little Free Library” bins, however with opioid reversal remedy as an alternative of tattered paperbacks — in homeless encampments and different locations the place drug customers congregate.

Forensic assistant Laurentiu Bigu, left, and investigator Ryan Parraz from the Los Angeles County coroner’s workplace cowl the physique of a homeless man discovered lifeless on a sidewalk in Los Angeles on April 18. The 60-year-old man died from the results of methamphetamine, based on his post-mortem report. Almost 2,000 homeless individuals died in Los Angeles from April 2020 to March 2021, with overdoses killing greater than 700.
(Jae C. Hong / Related Press)
Tutorial analysis helps the concept that overdoses might be considerably diminished by way of secondary distribution, a time period for the follow of giving naloxone to individuals who then move it on to others who’re comparatively more likely to witness an overdose. A 2018 research by researchers on the College of Pittsburgh discovered “including secondary distribution by means of social networks to a single website resulted in 42.5% fewer overdose deaths.”
A spokesperson for the California Division of Public Well being stated the U.S. Meals and Drug Administration is pursuing assessment of over-the-counter distribution as a result of “naloxone saves lives.”
“The general public well being advantage of administering naloxone throughout an overdose far outweighs any potential dangers associated to naloxone unwanted effects or danger of overdose loss of life within the absence of naloxone,” the spokesperson stated in an e mail.
5Cities isn’t the primary group to take an curiosity in providing naloxone to untrained individuals.
Bins containing free doses have been put in in a handful of places throughout California. However the few which were put in are principally at prisons and repair suppliers’ places of work, they usually signify little greater than a drop within the ocean of want.
For advocates and repair suppliers throughout the state, considerations about legal responsibility stand in the way in which of their imaginative and prescient of a society with broad, quick access.
California legislation protects licensed healthcare suppliers and folks with correct coaching from legal responsibility in the event that they administer an opioid reversal drug in good religion to somebody who’s overdosing.
However there may be much less readability about whether or not a person, group or company might be held liable or sued if they provide a naloxone package to somebody who has not been educated in its use — or who passes it on to an untrained individual — who then administers it to somebody who finally ends up struggling a unfavorable response or dying.
Requested in an e mail about potential legal responsibility, the state Division of Public Well being didn’t present steering past suggesting entities seek the advice of with their attorneys.
“I haven’t actually gotten to the purpose of figuring that out,” stated Nichols, of 5Cities. “Our workers are educated, and we supply it with us. If we see [an overdose] taking place, we’re coated to manage it. However the query is what if our workers fingers it to someone … and that individual then makes use of it to assist someone else?”
***

Anthony Delio, 36, falls asleep standing up in an alley after smoking fentanyl on Aug. 23 in Los Angeles. For too many individuals strung out on the drug, the sleep that follows a fentanyl hit is everlasting. The extremely addictive and probably deadly drug has change into a scourge throughout America and is taking a toll on the rising variety of individuals residing on the streets of Los Angeles.
(Jae C. Hong / Related Press)
There have been an estimated 6,843 overdose deaths associated to opioids in California in 2021, based on preliminary information from the state Division of Public Well being. Of these, 5,722 had been fentanyl-related.
San Francisco made a daring push in January to deliver down the loss of life toll when it opened a “linkage middle” within the metropolis’s drug-laden Tenderloin neighborhood. The open-air website was pitched as a progressive effort to attach drug customers with rehabilitative, overdose prevention and psychological well being companies, in addition to to assist them discover housing and supply meals, showers and different requirements.
Days after it opened, information retailers confirmed that use of unlawful medicine was being allowed on the middle. The stories raised considerations about whether or not it was a de facto “protected consumption” website, relatively than a spot for drug customers to acquire companies and sources.
Earlier this month, Mayor London Breed’s workplace stated greater than 100,000 individuals had visited the middle, which offered hundreds of meals and showers and helped receive shelter or housing for greater than 1,000 individuals, the San Francisco Chronicle reported.
Greater than 300 overdoses had been reversed on the middle. However fewer than 1% of visits to the location linked individuals with habit or psychological well being remedy.

An individual smokes an unlawful substance at UN Plaza in San Francisco on Dec. 17. Dozens of individuals eat fentanyl, meth and different unlawful substances in public close to the location of a just lately closed protected consumption website.
(Josh Edelson / For The Instances)
On Dec. 4, the middle shut down, leaving drug customers, service suppliers and different observers questioning what, if something, will exchange it and the assistance it offered in San Francisco. Related questions face different communities throughout California seeing skyrocketing numbers of opioid overdose deaths.
Eleven days earlier than he vetoed a protected consumption website pilot program, Gov. Gavin Newsom signed a invoice permitting pharmacists to distribute new, extra highly effective and faster-acting opioid reversal brokers as soon as they’ve been permitted by the FDA. The legislation makes it so such medicine wouldn’t should be individually permitted on the state degree earlier than pharmacists may distribute them.
The legislation is a vital step towards guaranteeing that any new opioid-reversal medicine might be extra rapidly made obtainable statewide, state Sen. John Laird (D-Santa Cruz) stated final week. It may have an actual impression on the struggle to cease overdoses from killing individuals, he stated, and it may incentivize pharmaceutical firms to develop opioid-reversal medicine.
“Within the face of such an enormous disaster, we’ve got to have each device we will have obtainable,” Laird stated.
***
In Oakland, a pilot undertaking will make naloxone obtainable in transitional housing for homeless individuals who use medicine or have substance use issues. Every of the constructing’s a number of flooring can have a field containing Narcan that its roughly 120 residents can be free to take and use within the occasion of an overdose.
Jared Bunde is a registered nurse with Alameda County Well being Look after the Homeless, one of many three service suppliers heading up the initiative. He stated that although the undertaking “hasn’t launched but, we’ve got the Narcan, we’ve got the bins. We’ve got to put in the bins. And we’ve got to see what the uptake is and if individuals truly use the bins and take the naloxone.”
It’s a easy thought — making lifesaving medicine available to the individuals who want it most. However even Bunde stated he’s not completely positive whether or not his group or others may open themselves as much as legal responsibility by distributing naloxone on to individuals who is probably not educated in its use, or who might give it to others.

Jenn Bennett, who’s excessive on fentanyl, sits on her skateboard with a visual black eye as her pal Jesse Williams smokes the drug on Aug. 9 in Los Angeles.
(Jae C. Hong / Related Press)
“One thing I’d be searching for could be elevated readability round secondary distribution, as a result of I don’t truly know. I don’t suppose anyone would get in hassle for it, however I wouldn’t need to give something lower than concrete recommendation,” he stated.
Anthony Cava, a spokesperson for the California Division of Well being Care Providers, didn’t present a direct reply to a query about whether or not suppliers may face legal responsibility for giving the medication to untrained individuals.
“By way of the DHCS Naloxone Distribution Undertaking (NDP), certified organizations and entities are capable of request free naloxone and have it instantly shipped,” Cava stated in an e mail. “They’re additionally required to obtain coaching in opioid overdose prevention and remedy, and supply coaching to people who obtain naloxone from them.”
In Los Angeles, the Homeless Outreach Program Built-in Care System, or HOPICS, is working to distribute extra naloxone to unhoused individuals.
“We’re taking hurt discount to the streets to begin saving lives,” stated Veronica Lewis, the company’s director. “From about April 2021 till now, we’ve reversed, based mostly on our naloxone distribution to individuals residing outside, virtually 200 overdoses. We give out the naloxone to people who find themselves in all probability utilizing alongside the people who find themselves overdosing.”

Two drug customers sleep in an alley on Sept. 21 in Los Angeles.
(Jae C. Hong / Related Press)
In Los Angeles County, attitudes about entry to naloxone are altering quick. In the summertime of 2021, the L.A. County Division of Well being Providers rolled out a program handy out tens of hundreds of bins of Narcan.
Lewis stated the remedy can even be obtainable in two everlasting supportive housing tasks underneath improvement in L.A. County.
However getting so far wasn’t a fast course of. Lewis stated it took “a few yr” to get the required approvals from the town of L.A. handy out naloxone on the road. HOPICS additionally labored with the county to assist it replace its insurance policies to permit service suppliers to distribute naloxone on to homeless people and prepare them on easy methods to administer it, she added.
But even now HOPICS doesn’t “move it out to individuals to move it out to different individuals,” she stated. “We move it out to individuals to make use of it.”
“There’s been a widespread push to get naloxone in additional individuals’s fingers. … I believe we’re on our approach there, we’re simply not fairly there but.”

Science
Column: Democrats show that they're no better than Trump in allowing politics to interfere with science

Anyone who cares about the importance of science in the making of government policy had to be deeply dispirited by the hearing into the origins of COVID-19 staged by a Republican-led House subcommittee on May 1.
The sole witness at the hearing, and its target, was Peter Daszak, the head of EcoHealth Alliance, a nongovernmental organization tasked with overseeing international virus research funded by federal agencies.
It wasn’t just that the GOP majority used the occasion to promote the ignorant, imbecilic and 100% evidence-free notion that SARS-CoV-2, the virus that caused the COVID pandemic, originated in a Chinese laboratory, through work funded by the U.S. government, and overseen by EcoHealth.
Science is a myth-buster…Because of this, science has become a nuisance, even an enemy to some industries and many of the most powerful actors in the new attention economy.
— Science blogger Philipp Markolin
It was that the Democratic minority showed itself to be complicit with the GOP attack on EcoHealth.
As I wrote at the time, the Democrats threw Daszak and by extension science itself under the bus: “Perhaps they hoped that by allowing Daszak to be drawn and quartered, they might persuade the Republicans to climb down from their evidence-free claims about government complicity in the pandemic’s origins.”
The Democrats’ craven and shameful performance hinted that EcoHealth’s government funding, which had been blocked by the Trump administration and restored, though delayed, under Biden, was pretty much doomed.
On Wednesday, the bell tolled. EcoHealth received a notice from the Department of Health and Human Services, the parent agency of the NIH, that it was immediately suspending all funding to the organization and moving to “debar” it from federal funding going forward.
It’s impossible to overstate what a serious blow this is for EcoHealth and research into the origins of pathogens that could cause illness and death on a global scale — the central purpose of EcoHealth’s work.
The organization, which has operated with a budget of about $16 million, cannot receive a contract from any federal agency or even serve as a subcontractor of another awardee. All organizations with federal contracts that have affiliated with EcoHealth will be “carefully examined.”
EcoHealth says it will appeal the proposed debarment, as is its right. But that process could take years. In the meantime, the organization will be effectively out of money, and very likely out of business. The HHS action effectively turns one of the leading organizations in the quest to protect humankind from the next pandemic into a pariah, completely unjustifiably.
The debarment threat “will mean the demise of EcoHealth, one of the most scientifically productive and internationally respected groups conducting field surveillance for potential pandemic viruses,” says Gerald T. Keusch, a former associate director of international research at the NIH. “And that means our national security will be compromised.”
Let’s be clear about what has happened here. EcoHealth has been made a scapegoat for the pandemic for partisan reasons. The process started with President Trump. At a news conference on April 17, 2020, a reporter from a right-wing organization mentioned that the NIH had given a $3.7-million grant to the Wuhan Institute of Virology. (Actually, the WIV grant, which was channeled from a larger EcoHealth grant, was only $600,000.)
Trump, sensing an opportunity to show a strong hand against China and advance his effort to blame the Chinese for the pandemic, responded: “We will end that grant very quickly.” The NIH terminated the grant one week later, prompting a backlash from the scientific community, including an open letter signed by 77 Nobel laureates who saw the action as a flagrantly partisan interference in government funding of scientific research.
The HHS inspector general found the termination to be “improper.” The NIH reinstated the grant, but immediately suspended it until EcoHealth met several conditions that were manifestly beyond its capability, as they involved its demanding information from the Chinese government that it had no right to receive. The grant was reinstated last year under Biden, but NIH bureaucrats, perhaps worried about their careers in a new Trump administration, continued to put administrative obstacles in the way of EcoHealth’s work.
The attacks on Daszak and his organization are simply instruments of the GOP project to pin blame for the pandemic on Anthony Fauci, one of the world’s most respected public health figures.
The context is a battle for the minds of uninformed and misinformed Americans over the origin of COVID-19. The hypothesis favored by most qualified virologists and epidemiologists is that the virus reached humans the way most viruses do — as spillovers from wildlife. The alternative hypothesis, for which absolutely not a speck of evidence has ever been presented, is that the virus emerged from a laboratory—specifically the Wuhan Institute of Virology in China, whether deliberately or through sloppy lab practices.
The latter hypothesis was initially promoted by an anti-China cabal in the Trump-era State Department. Although they never produced any grounds for the conspiracy theory, it remains favored by anti-vaccine agitators and in the Republican anti-science camp. It has a certain appeal for uninformed people susceptible to sinister explanations of complicated, troubling events; but it’s not science.
Daszak calls the government actions “fundamentally unfair” and “based on a set of false assumptions about COVID-19 origins and on persistent mischaracterizations and misunderstandings of our research…Our work has been at the forefront of understanding pandemic risk for over two decades, and it’s a very cruel irony that because we knew that China was a potential hotspot for the next coronavirus pandemic, we’re now being targeted in a political backlash caused by exactly the type of pandemic we were concerned about preventing.”
An outgrowth of the lab-leak fantasy is the asinine claim that as head of the National Institute of Allergy and Infectious Diseases, Fauci funded research in China that created the pandemic virus and let it loose on the world, and then concealed his complicity. This is a favorite meme among lab-leak fanatics. Among the research bodies that received NIAID funding to conduct field work in China was EcoHealth. (Fauci retired last year as director of NIAID, which is part of the National Institutes of Health.)
On May 1, the GOP-led Select Subcommittee on the Coronavirus Pandemic brought things to a head with its grilling of Daszak. It was a circus featuring posturing politicians intent on smearing Daszak and EcoHealth on the pretext of getting to the bottom of the pandemic’s cause. The committee Democrats participated fully, hammering Daszak as a “poor steward of the taxpayers’ dollars,” based on transparent trivialities.
During a follow-up subcommittee hearing Thursday, ranking member Raul Ruiz (D-Indio) alluded to the dishonestly of the GOP attack on Fauci. But, perhaps inadvertently, he also exposed the dishonesty of his caucus’ attack on Daszak.
The committee Republicans, Ruiz said, “still have not succeeded in substantiating their allegations that NIH and NIAID through a grant to EcoHealth Alliance created SARS-CoV-2 and conspired to cover it up. … No evidence demonstrates that work performed under the EcoHealth grants, including at the Wuhan Institute of Virology, led to the creation of SARS-CoV-2.”
Does Ruiz ever listen to the words coming out of his mouth? The very goal of the GOP’s dragging Daszak and EcoHealth into this controversy was to fabricate a link in the chain between Fauci and COVID-19; by rejecting the GOP position, Ruiz demolished the case against EcoHealth.
Yet Ruiz didn’t walk the last mile. “EcoHealth has defied its obligations to be a transparent steward of taxpayer dollars,” he said, repeated the lame case against the organization that he first aired, in connivance with the Republicans, during the public interrogation of Daszak on May 1.
Legitimate scientists, such as virology experts uninfected by the conspiratorial fantasy that the virus originated in the lab, are aghast at the suspension of EcoHealth’s funding and the organization’s likely debarment, as well as the Democrats’ supine behavior.
The Democrats, as Stuart Neil, a professor of virology at Kings College London, wrote on X, “have made some shoddy back room deal to allow them to look tough to the conspiracy theorists.” Neil is right. There is no rational explanation for the Democrats’ behavior than some sort of deal with the Republican majority to give them cover to challenge the lab leak theory.
Put it all together, and it looks like HHS started with a politically driven impulse to cut off EcoHealth’s funding, followed by an effort to assemble every justification for doing so, no matter how trivial. The absurdity of its action drips from the closing words of the notice issued by H. Katrina Brisbon, an HHS “suspension and debarment official.” She wrote that “the immediate suspension of EHA is necessary to protect the public interest and due to a cause of so serious or compelling a nature that it affects EHA’s present responsibility.”
The notice was accompanied by an 11-page bill of particulars, but they all boil down to two key purported offenses — that EcoHealth had missed a 2019 deadline for an annual report of its activities to NIH, and that work EcoHealth had funded in China had produced a recombinant version of a virus that grew fast enough to trigger a safety halt in the work.
The first was tantamount to a traffic violation. EcoHealth maintained that it hadn’t been able to file the report on time because it had been locked out of NIH’s onlline reporting portal, which NIH denies. On the second, there were legitimate disagreements over whether the subject virus’ growth actually did trigger the halt requirement; in any case, the virus wasn’t a threat to human health. The work at issue took place in 2018.
HHS cited several other supposed offenses, including EcoHealth’s failure to submit lab notebooks from the Wuhan institute that NIH has requested in November 2021. But since NIH had ordered EcoHealth to stop funding the institute as of April 2020, those notebooks were plainly out of its reach.
Daszak says EcoHealth will respond to the HHS and the subcommittee “with documentary evidence…refuting every single allegation that’s been levied against us.”
The roots of anti-science slant of Trump and others on the far right isn’t hard to discern. It’s aimed at protecting the economic establishment from new ideas and realities such as global warming, while providing financial and personal opportunities for grifters and charlatans.
Swiss scientist and science blogger Philipp Markolin has put his finger on this phenomenon.
“Science is a myth-buster,” he writes. “Its debunking activity reduces the value of information products that too many media manipulators rely on for their business. Because of this, science has become a nuisance, even an enemy to some industries and many of the most powerful actors in the new attention economy.”
Why did the Democrats agree to participate in this charade? In joining the Daszak smear, they have shredded their credibility as of scientific truth, at the very moment when science is most in need of their protection.
The time has come to ask this question of Ruiz, his Democratic colleagues on the coronavirus subcommittee — Debbie Dingell of Michigan, Kwesi Mfume of Maryland, Deborah Ross of North Carolina, Robert Garcia of Long Beach, Ami Bera of Sacramento and Jill Tokuda of Hawaii — along with Health and Human Services Secretary Xavier Becerra: How can you live with yourselves?
Science
Star USC scientist faces scrutiny — retracted papers and a paused drug trial

Late last year, a group of whistleblowers submitted a report to the National Institutes of Health that questioned the integrity of a celebrated USC neuroscientist’s research and the safety of an experimental stroke treatment his company was developing.
NIH has since paused clinical trials for 3K3A-APC, a stroke drug sponsored by ZZ Biotech, a Houston-based company co-founded by Berislav V. Zlokovic, professor and chair of the department of physiology and neuroscience at the Keck School of Medicine of USC.
Three of Zlokovic’s research papers have been retracted by the journal that published them because of problems with their data or images. Journals have issued corrections for seven more papers in which Zlokovic is the only common author, with one receiving a second correction after the new supplied data were found to have problems as well.
For an 11th paper co-authored by Zlokovic the journal Nature Medicine issued an expression of concern, a note journals append to articles when they have reason to believe there may be a problem with the paper but have not conclusively proven so. Since Zlokovic and his co-authors no longer had the original data for one of the questioned figures, the editors wrote, “[r]eaders are therefore alerted to interpret these results with caution.”
“It’s quite unusual to see this volume of retractions, corrections and expressions of concern, especially in high-tier influential papers,” said Dr. Matthew Schrag, an assistant professor of neurology at Vanderbilt who co-authored the whistleblower report independently of his work at the university.
Both Zlokovic and representatives for USC declined to comment, citing an ongoing review initiated in the wake of the allegations, which were first reported in the journal Science.
“USC takes any allegations of research integrity very seriously,” the university said in a statement. “Consistent with federal regulations and USC policies, this review must be kept confidential.”
Zlokovic “remains committed to cooperating with and respecting that process, although it is unfortunately required due to allegations that are based on incorrect information and faulty premises,” his attorney Alfredo X. Jarrin wrote in an email.
Regarding the articles, “corrections and retractions are a normal and necessary part of the scientific post-publication process,” Jarrin wrote.
Authors of the whistleblower report and academic integrity experts challenged that assertion.
“If these are honest errors, then the authors should be able to show the actual original data,” said Elisabeth Bik, a microbiologist and scientific integrity consultant who co-wrote the whistleblower report. “It is totally human to make errors, but there are a lot of errors found in these papers. And some of the findings are suggestive of image manipulation.”
Given the staid pace of academic publishing, publishing this many corrections and retractions only a few months after the initial concerns were raised “is, bizarrely, pretty quick,” said Ivan Oransky, co-founder of Retraction Watch.
The whistleblower report submitted to NIH identified allegedly doctored images and data in 35 research papers in which Zlokovic was the sole common author.
“There had been rumblings about things not being reproducible [in Zlokovic’s research] for quite some time,” Schrag said. “The real motivation to speak publicly is that some of his work reached a stage where it was being used to justify clinical trials. And I think that when you have data that may be unreliable as the foundation for that kind of an experiment, the stakes are just so much higher. You’re talking about patients who are often at the most vulnerable medical moment of their life.”
Over the years, Zlokovic has created several biotech companies aimed at commercializing his scientific work. In 2007, he co-founded ZZ Biotech, which has been working to gain federal approval of 3K3A-APC.
The drug is intended to minimize the bleeding and subsequent brain damage that can occur after an ischemic stroke, in which a blood clot forms in an artery leading to the brain.
In 2022, USC’s Keck School of Medicine received from NIH the first $4 million of a planned $30-million grant to conduct Phase III trials of the experimental stroke treatment on 1,400 people.
In Phase II of the trial, which was published in 2018 and called Rhapsody, six of the 66 patients who received 3K3A-APC died in the first week after their stroke, compared to one person among the 44 patients who got a placebo. Patients who received the drug also tended to report more disability 90 days after their stroke than those who got the placebo. The differences between the two groups were not statistically significant and could have been due to chance, and the death rate for patients in both groups evened out one month after the initial stroke.
“The statements that there is a risk in this trial is false,” said Patrick Lyden, a USC neurologist and stroke expert who was employed by Cedars-Sinai at the time of the trial. Zlokovic worked with Lyden as a co-investigator on the study.
One correction has been issued to the paper describing the Phase II results, fixing an extra line in a data table that shifted some numbers to the wrong columns. “This mistake is mine. It’s not anybody else’s. I didn’t catch it in multiple readings,” Lyden said, adding that he noticed the error and was already working on the correction when the journal contacted him about it.
He disputed that the trial represented any undue risk to patients.
“I believe it’s safe, especially when you consider that the purpose of Rhapsody was to find a dose — the maximum dose — that was tolerated by the patients without risk, and the Rhapsody trial succeeded in doing that. We did not find any dose that was too high to limit proceeding to Phase III. It’s time to proceed with Phase III.”
Schrag stressed that the whistleblowers did not find evidence of manipulated data in the report from the Phase II trial. But given the errors and alleged data manipulation in Zlokovic’s earlier work, he said, it’s appropriate to scrutinize a clinical trial that would administer the product of his research to people in life-threatening situations.
In the Phase II data, “there’s a coherent pattern of [patient] outcomes trending in the wrong direction. There’s a signal in early mortality … there’s a trend toward worse disability numbers” for patients who received the drug instead of a placebo, he said.
None are “conclusive proof of harm,” he said. But “when you’re seeing a red flag or a trend in the clinical trial, I would tend to give that more weight in the setting of serious ethical concerns around the pre-clinical data.”
The NIH paused the clinical trial in November, and it remains on hold, said Dr. Pooja Khatr, principal investigator of the NIH StrokeNet National Coordinating Center. Khatr declined to comment on the pause or the trial’s future, referring further questions to USC and NIH.
The NIH Office of Extramural Research declined to discuss Rhapsody or Zlokovic, citing confidentiality regarding grant deliberations.
ZZ Biotech Chief Executive Kent Pryor, who in 2022 called the drug “a potential game-changer,” said he had no comment or information on the halted trial.
Zlokovic is a leading researcher on the blood-brain barrier, with particular interest in its role in stroke and dementia. He received his medical degree and doctorate in physiology at the University of Belgrade and joined the faculty at USC’s Keck School of Medicine after several fellowships in London. A polyglot and amateur opera singer, Zlokovic left USC and spent 11 years at the University of Rochester before returning in 2011. He was appointed director of USC’s Zilkha Neurogenetic Institute the following year.
A USC spokesperson confirmed that Zlokovic has retained his titles as department chair and director of the Zilkha institute.
Science
What military doctors can teach us about power in the United States

Power is invisible, but its effects can be seen everywhere — especially in the health records of active duty military personnel.
By examining details of 1.5 million emergency room visits at U.S. military hospitals nationwide, researchers found that doctors invested significantly more resources in patients who outranked them than in patients of equal or lesser rank. The additional clinical effort devoted to powerful patients came at the expense of junior patients, who received worse care and were more likely to become seriously ill.
Military rank wasn’t the only form of power that translated into inequitable treatment. The researchers documented that patients fared better when they shared the same race or gender as their doctor, a pattern that tended to favor white men and caused Black patients in particular to be shortchanged by their physicians.
The results were published Thursday in the journal Science.
The findings have implications far beyond the realm of the military, said Manasvini Singh, a health and behavioral economist at Carnegie Mellon University who conducted the research with Stephen D. Schwab, an organizational health economist at the University of Texas at San Antonio.
For instance, they can help explain why Black students do better in school when they are taught by Black teachers, and why Black defendants get more even-handed treatment from Black judges.
“We think our results speak to many settings,” Singh said.
The disparities wrought by power imbalances are easy to spot but difficult to study in real-world scenarios.
“It’s just hard to measure power,” Singh said. “It’s abstract, it’s complicated.”
That’s where the military health records come in.
The Military Health System operates 51 hospitals across the country. The doctors who staff them are active-duty personnel, as are many of the patients they treat. Comparing their ranks gave Singh and Schwab a handy way to gauge the power differential between physicians and the people in their care.
The researchers restricted their analysis to patients who sought treatment in emergency departments, where patients are randomly assigned to doctors. That randomness made it easier to measure how power influenced the treatment patients received.
To further isolate the effects of power, the researchers made comparisons between patients of the same rank. If they happened to outrank their doctor, they were considered a “high-power” patient. If not, they were classified as a “low-power” patient.
The medical records showed that doctors put 3.6% more effort into treating high-power patients than low-power ones. They also utilized significantly more resources such as clinical tests, scans and procedures, according to the study.
Those extra resources translated into better care: High-power patients were 15% less likely to become sick enough to be admitted to the hospital over the next 30 days.
To see if they could replicate their results, Singh and Schwab narrowed their focus to doctors who treated patients within a one-year period before or after the patients were promoted to a higher rank. The researchers found that doctors devoted 1% more effort to patients post-promotion, as well as more medical resources. Those differences may have been small, but they were statistically significant, Schwab said.
Next, the pair considered what happened to low-power patients while high-power patients were getting extra attention. One hypothesis was that ordering additional tests for one patient might prompt doctors to order the same tests for everyone they treated that day. It was also possible that the decisions doctors made for their high-power patients had no bearing on their other patients.
Neither turned out to be the case. Instead, the added effort spent on high-power patients was siphoned away from low-power patients, who got 1.9% less effort from their doctors. On top of that, their risk of needing to return to the ER or be admitted to the hospital over the following 30 days increased by 3.4%, the researchers found.
“The powerful unwittingly ‘steal’ resources from less-powerful individuals,” Schwab and Singh wrote.
Outside the military, doctors and patients can’t use official rank to measure their power relative to each other, but they do contend with the effects of race and gender. That led the researchers to investigate whether the physicians in their study treated patients differently if they shared these attributes.
White doctors devoted more effort to white patients than to Black patients across the board, the researchers found. The gap was the same regardless of whether the doctor had a higher or lower rank than the patient.
However, white doctors increased their effort for high-power patients by the same amount regardless of race. As a result, white doctors treated high-power Black patients the same, on average, as low-power white patients.
The story was different for Black doctors. When they outranked their patients, they gave essentially the same amount of effort to everyone. But on the rare occasions when they encountered a higher-ranked Black patient, the amount by which they dialed up their efforts was more than 17 times greater than it was when they treated a higher-ranked white patient.
It’s not clear what accounted for this “off-the-charts effort,” the researchers wrote. They speculated that since Black service members were underrepresented among the pool of high-power patients, Black doctors were particularly attuned to their status.
The effects of gender were more difficult to ascertain, since biology dictates that men and women require different kinds of care.
Both male and female doctors invested the most effort in female patients who outranked them. But male doctors upgraded their care for high-power patients of both genders to a much greater extent than female doctors. And unlike female doctors, male doctors devoted more effort to female patients across the board.
Finally, the researchers wondered whether doctors gave preferential treatment to high-power patients because of their elevated status or because those patients had the authority to make trouble if they were unsatisfied with their care. To make inferences about this, they compared the treatment of retirees (who retained their status but had given up their authority) to the treatment of active-duty patients (who still had both).
Schwab and Singh found that high-power patients continued to elicit extra effort from doctors for up to five years after they retired, suggesting that status was an important factor.
“I think it’s really, really cool that even after retirement, you still have these effects,” said Joe C. Magee, a professor of management and organization at the NYU Stern School of Business who studies the role of hierarchy. He sees that as a strong sign that status was driving doctors’ decisions all along.
“What these folks are able to show is that it has real health consequences,” Magee said.
Eric Anicich, a professor of management and organization at the USC Marshall School of Business, called the study “impressive” and the findings “important.”
Although a 3.5% increase or a 1.9% decrease in physician effort may seem small, their cumulative impact is meaningful, especially when it comes to something as critically important as healthcare, he said.
The inequities documented in the study aren’t unique to doctors or to the armed forces, Schwab and Singh said. The mathematical model they developed to describe the behavior in military emergency rooms also helps explain why people in all kinds of situations give preferential treatment to people who look like them: It may help minimize the effects of societal disparities.
In a commentary that accompanies the study, Laura Nimmon of the University of British Columbia’s Centre for Health Education Scholarship wrote that “the ephemeral and unobservable nature of power has made it profoundly difficult to study.” But she said it’s worth the effort to make sure doctors wield their power more fairly.
The disparities reported by Schwab and Singh are “of serious concern to society at large,” she wrote.
-

 World1 week ago
World1 week agoPentagon chief confirms US pause on weapons shipment to Israel
-

 Politics1 week ago
Politics1 week agoRFK Jr said a worm ate part of his brain and died in his head
-

 Politics1 week ago
Politics1 week agoOhio AG defends letter warning 'woke' masked anti-Israel protesters they face prison time: 'We have a society'
-

 Education1 week ago
Education1 week agoVideo: Police Use Pepper Spray on Protesters on G.W.U.’s Campus
-

 News1 week ago
News1 week agoNine Things We Learned From TikTok’s Lawsuit Against The US Government
-
 Politics1 week ago
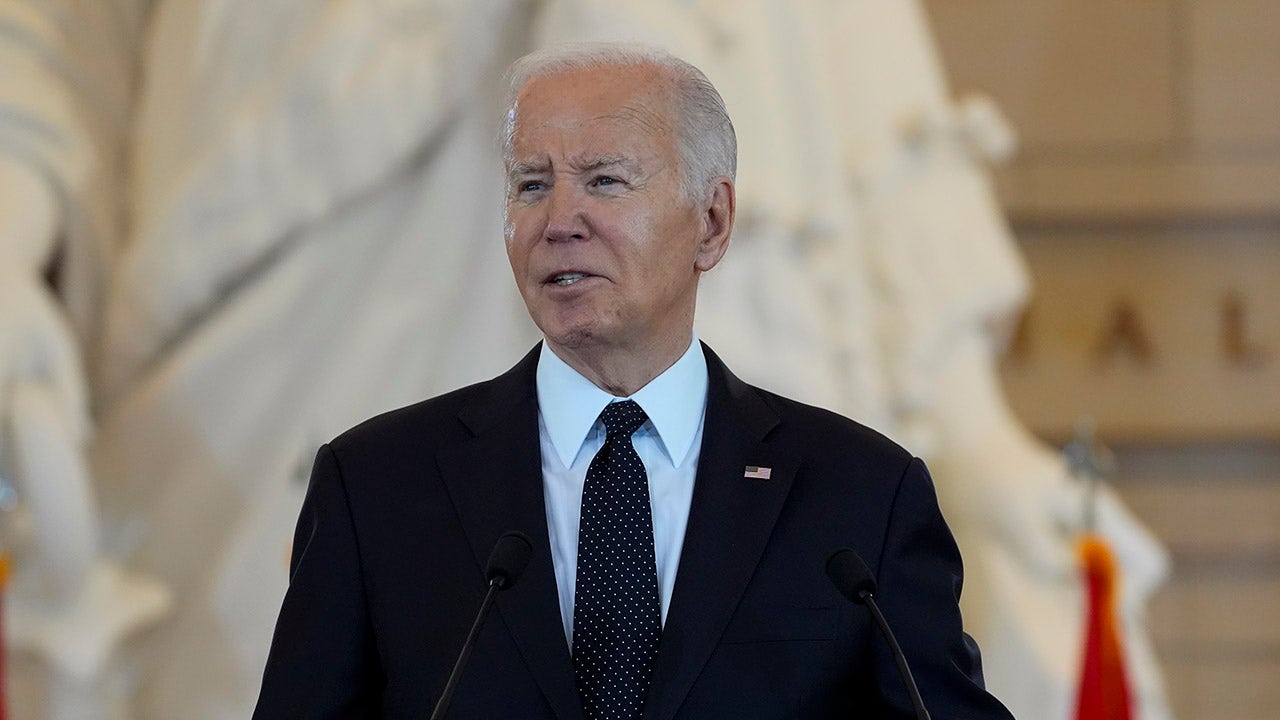
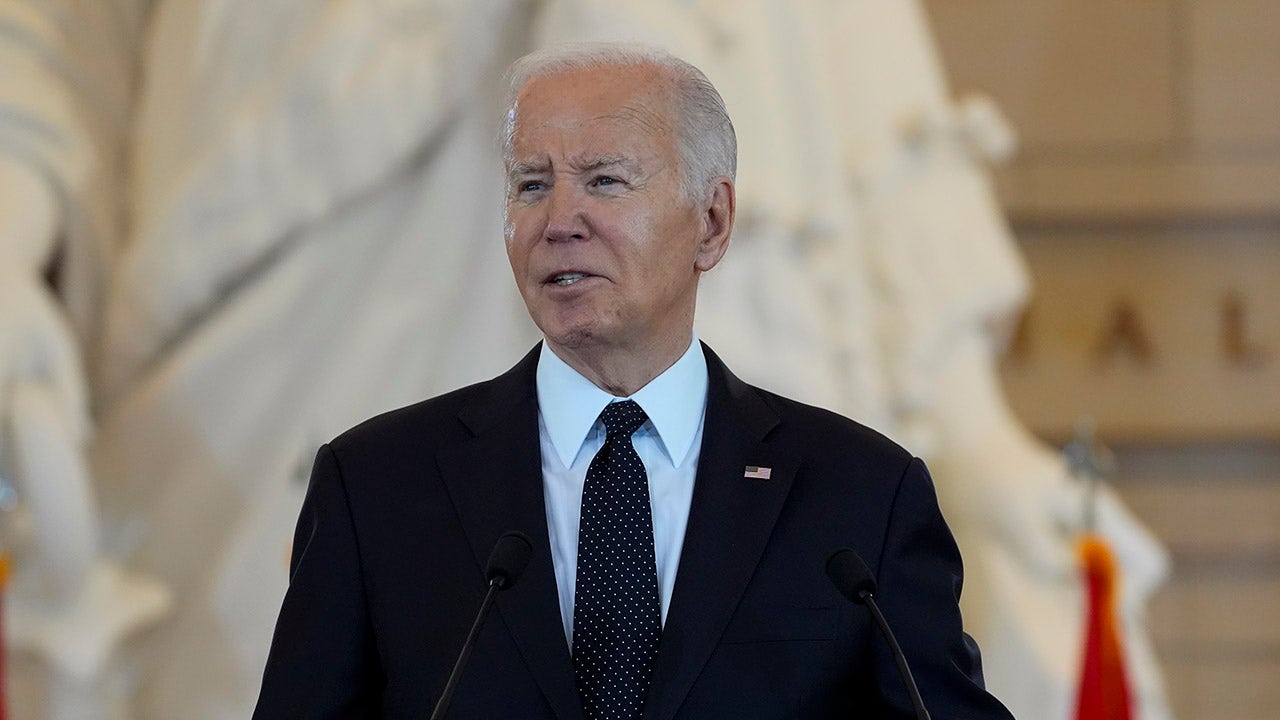
Politics1 week agoBiden’s decision to pull Israel weapons shipment kept quiet until after Holocaust remembrance address: report
-

 World1 week ago
World1 week agoA look at Chinese investment within Hungary
-

 News1 week ago
News1 week agoThe Major Supreme Court Cases of 2024















