Health
Will monkeypox become an ‘established STD’? Why one infectious disease expert thinks so
NEWNow you can hearken to Fox Information articles!
The Nigerian physician who handled the 2017 monkeypox outbreak in Nigeria advised Fox Information in an interview that the virus now “exhibits the entire indicators of changing into a longtime STD,” as extra U.S. instances come up and the Biden administration has known as the outbreak a public well being emergency.
Infectious illness doctor Dr. Dimie Ogoina handled the primary monkeypox case in Nigeria in almost 40 years. That 12 months of 2017, an 11-year-old boy got here to him with a chickenpox-like rash.
The physician mentioned he had “by no means seen a monkeypox case in my life — I [had] solely seen footage,” Ogoina advised Fox Information.
MONKEYPOX VACCINE AUTHORIZATION EXPANDED BY FDA TO INCREASE DOSE SUPPLY
Docs found the primary documented instances of monkeypox in people within the Nineteen Seventies amongst kids from Congo, Liberia and Sierra Leone. Previous to that, scientists detected the primary instances amongst monkeys in an animal facility in Copenhagen, Denmark, in 1958 — giving the illness the identify “monkeypox.”
However in 2017, Dr. Ogoina — a professor of medication and infectious illnesses at Niger Delta College in Nigeria — seen that the 11-year-old boy didn’t have contact with animals. The virus unfold amongst his household, first infecting his uncle, then spreading to his mom, father and youthful brother.
A registered nurse prepares a dose of a monkeypox vaccine on the Salt Lake County Well being Division on July 28, 2022, in Salt Lake Metropolis. On Aug. 9, 2022, U.S. well being officers approved a brand new monkeypox vaccination technique designed to stretch restricted provides by permitting well being professionals to vaccinate as much as 5 folks — as a substitute of 1 — with every vial.
(AP Picture/Rick Bowmer, File)
After sending samples of the boy’s lesions to a lab in Senegal, Dr. Ogoina confirmed his suspicions: The boy had contracted the primary case of monkeypox in Nigeria in 38 years.
The outbreak in 2017 grew to 200 confirmed instances in Nigeria. Since then, the monkeypox virus went from a uncommon illness to an endemic standing in Africa — with instances spreading primarily amongst younger, homosexual and bisexual males.
Whereas the virus is just not an endemic within the U.S., Dr. Ogoina advised Fox Information that in his opinion, it does present indicators of changing into “a longtime STD” — that means it’s spreading among the many U.S. inhabitants like different illnesses comparable to chlamydia, gonorrhea or HIV.
The CDC advised Fox Information that whereas the virus will be sexually transmitted, it has not reached sexually transmitted an infection (STI) standing.
In 2021, the U.S. confirmed two instances of monkeypox from vacationers coming from Nigeria.
The CDC cited contract tracing efforts and “sturdy collaboration between CDC, state and native well being departments, airline and airport companions” as causes for holding the unfold.
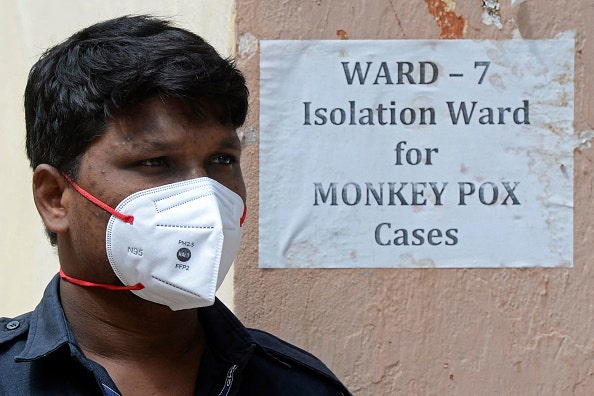
A person is proven within the “isolation ward” for monkeypox instances at a clinic in India.
Now, lower than one 12 months later, monkeypox instances are rising.
There are 14,115 confirmed monkeypox (orthopoxvirus) instances within the U.S. as of Thursday afternoon, Aug. 18, 2022, in keeping with the CDC.
In response to a question, the CDC advised Fox Information that whereas the virus will be sexually transmitted, it has not reached sexually transmitted an infection (STI) standing.
“It exhibits us that the virus is evolving and adapting extra to the human host,” mentioned Dr. Dimie Ogoina.
“[The] present outbreak has led to questions on whether or not monkeypox is a sexually transmitted an infection (STI). Monkeypox can extra precisely be described as ‘sexually transmissible.’ In different phrases, intercourse is likely one of the ways in which monkeypox will be unfold, however not the one manner,” the company mentioned.
“Within the present monkeypox outbreak,” it added, “the virus is spreading primarily by means of shut contact with somebody who has monkeypox. This consists of contact with monkeypox sores or respiratory secretions by way of shut, sustained skin-to-skin contact that happens throughout intercourse.”

Healthcare employees at Anna Worldwide Airport terminal in Chennai, India, display passengers for monkeypox signs, taken on June 3, 2022.
(ARUN SANKAR/AFP by way of Getty Photos)
With instances on the rise, states have scrambled to distribute vaccines and increase testing efforts as HHS expands the monkeypox vaccine to greater than 1.1 million doses.
The Biden administration is trying to decrease doses, making the vaccine one-fifth as potent.
WHAT TO DO IF YOU GET MONKEYPOX: SYMPTIONS, VACCINATIONS AND TREATMENTS
On August 9, 2022, the White Home launched the next assertion, partly, about it.
“The Division of Well being and Human Providers (HHS) introduced a Part 564 declaration, permitting FDA to make use of its authority to permit well being care suppliers to manage as much as 5 instances the variety of vaccine doses per vial of JYNNEOS vaccine.”
It went on, “Following final week’s public well being emergency declaration, right this moment HHS Secretary Xavier Becerra issued a dedication underneath the Part 564 declaration of the Meals, Drug, and Beauty Act that enables for emergency use authorization of vaccines to forestall monkeypox and forestall extreme illness from the virus. This motion paves the way in which for the federal authorities to stand up to 5 instances the quantity of doses administered out of a single vial of the JYNNEOS vaccine.”
“The easiest way to comprise this danger is just not by means of vaccination,” mentioned Dr. Robert Malone. “It’s by means of contact tracing, abstinence and isolation till these individuals are now not infectious.”
It went on, “The EUA now permits for 0.1ml of the JYNNEOS vaccine to be administered between layers of the pores and skin (intradermally), versus 0.5ml of the vaccine that’s administered underneath the pores and skin (subcutaneously).”
Vaccine distribution is one think about halting the monkeypox outbreak. Different consultants level to different measures.
Dr. Robert Malone, co-inventor of the mRNA vaccine, advised Fox Information that in his view, vaccination shouldn’t be the primary line of protection.
“The easiest way to comprise this danger is just not by means of vaccination,” mentioned Malone. “It’s by means of contact tracing, abstinence and isolation till these individuals are now not infectious.”

Well being care employees with New York Metropolis Division of Well being and Psychological Hygiene assist folks register for the monkeypox vaccine at one of many Metropolis’s vaccination websites, on Tuesday, July 26, 2022, in New York.
(AP Picture/Mary Altaffer)
He additionally mentioned, “We do not even have any concept how efficient this vaccine actually is. It was not designed for monkeypox … What’s being achieved proper now may be very, very analogous to what occurred early within the coronavirus disaster.”
Public well being officers are additionally trying to battle the stigma surrounding the identify of the illness and the inhabitants affected.
“Newly recognized viruses, associated illness and virus variants ought to be given names with the purpose to keep away from inflicting offense to any cultural, social, nationwide, regional, skilled or ethnic teams …”
The WHO is trying to rename monkeypox, releasing an announcement that mentioned, “Present finest observe is that newly recognized viruses, associated illness and virus variants ought to be given names with the purpose to keep away from inflicting offense to any cultural, social, nationwide, regional, skilled or ethnic teams, and reduce any damaging affect on commerce, journey, tourism or animal welfare.”
WHO TO RENAME MONKEYPOX TO AVOID DISCRIMINATION AND STIGMATIZATION
Concerning the unfold of monkeypox, Dr. Malone additionally advised Fox Information, “It is a very small international cohort … and it is a sexually transmitted illness inside that international cohort of individuals that usually have very a number of intercourse companions.”
He additionally mentioned, “In public well being, I believe that now we have to be actually cautious about conditions by which we’re limiting our potential to speak successfully to the folks which can be on the highest danger.”
Regardless of the surge in instances, American voters will not be involved about monkeypox, in keeping with Fox Information polling. Fifty-four % of registered voters polled between August 6-9 mentioned they weren’t involved about monkeypox.
There’s an urgency, nonetheless, among the many international neighborhood to comprise the virus.
“It’s an an infection that has unfold so quick in additional than 50 international locations in lower than two months and continues to be spreading,” mentioned Dr. Ogoina.

Health
How Lagging Vaccination Could Lead to a Polio Resurgence

Most American parents hardly give thought to polio beyond the instant their child is immunized against the disease. But there was a time in this country when polio paralyzed 20,000 people in a year, killing many of them.
Vaccines turned the tide against the virus. Over the past decade, there has been only one case in the United States, related to international travel.
That could change very quickly if polio vaccination rates dropped or the vaccine were to become less accessible.
Robert F. Kennedy Jr., a longtime vaccine skeptic who may become the secretary of health and human services, has said the idea that vaccination has nearly eradicated polio is “a mythology.”
And while Mr. Kennedy has said he’s not planning to take vaccines away from Americans, he has long contended that they are not as safe and effective as claimed.
As recently as 2023, he said batches of an early version of the polio vaccine, contaminated with a virus, caused cancers “that killed many, many, many, many, many more people than polio ever did.” The contamination was real, but research never bore out a link to cancer.
Aaron Siri, a lawyer and adviser to Mr. Kennedy, has represented a client seeking to challenge the approval or distribution of some polio vaccines on the grounds that they might be unsafe.
Those efforts appear unlikely to succeed. And there is widespread support for vaccination among prominent Republicans, including President-elect Donald J. Trump and Senator Mitch McConnell, who had polio as a child.
But the secretary of health and human services has the authority to discourage vaccination in less direct ways. He or she could withdraw federal funds for childhood vaccination programs, hasten the end of school mandates in states already disinclined toward vaccines or fuel doubts about the shots, exacerbating a decline in immunization rates.
If polio vaccination rates were to fall, scientists say, the virus could slip into pockets of the country where significant numbers of people are unvaccinated, wreaking havoc once more. The virus may be nearly eradicated in its original form, but resurgence remains a constant threat.
Any decision the Trump administration makes regarding the polio vaccine is likely to ripple across the globe, said Dr. David Heymann, an infectious disease physician at the London School of Hygiene and Tropical Medicine and former leader of polio eradication at the World Health Organization.
“If the U.S. takes away the license, then many other countries will do the same thing,” he said. To have polio resurge when it is so close to eradication “would be very, very, very, very sad.”
Before 1955, when the vaccine was introduced, polio disabled more than 15,000 Americans each year and hundreds of thousands more worldwide. In 1952 alone, it killed 3,000 Americans after paralysis left them unable to breathe.
Many of those who survived still live with the consequences.
“People really underestimate how horrific polio was,” said Dr. Karen Kowalske, a physician and polio specialist at University of Texas Southwestern Medical Center in Dallas.
Many who recovered now suffer “post-polio syndrome”: Some of the original symptoms, including muscle weakness and respiratory problems, return.
Dr. Kowalske tends to about 100 post-polio patients who need braces, wheelchairs or other devices to cope with progressive weakness. Some are older adults who became infected before the vaccine was available; others are middle-aged immigrants from countries where polio remained a problem for much longer than in the United States.
To some survivors, the idea of polio’s return is unfathomable.
Carol Paulk contracted the disease in 1943, when she was just 3. Her right leg never recovered, and for the rest of her life she has walked with a pronounced limp and has been in near-constant pain.
Ms. Paulk is among the luckier ones. Until recently, she did not suffer the breathing, swallowing or digestive problems that often torment polio survivors.
She has had “a wonderful, wonderful life” with a husband and three daughters, a law degree and extensive travel abroad.
But always, everywhere, she is calculating how far away the next seat is, how long her energy will hold out and whether a given activity is worth debilitating pain the next day.
She didn’t participate in the 1963 March on Washington or play sports, as she desperately wanted to, or go hiking, skiing and bicycling with her husband.
If there were a public hearing about the polio vaccine now, “I would go, and I would take off my brace, and I would let them see my leg and ask them, is that what they want for their children?” she said.
Polio disables many fewer children now. Vaccination has scrubbed the virus from most of the planet, slashing the number of cases by more than 99.9 percent and preventing an estimated 20 million cases of paralysis.
Still, the virus has turned out to be a stubborn enemy, and eradication has been set back over and over again.
In 2024, 20 countries reported polio cases, and the virus was detected in wastewater in five European countries, decades after its official elimination from the region, and in Australia.
“Any reduction in coverage rates increases the risk of polio anywhere,” said Oliver Rosenbauer, a spokesman for the World Health Organization’s polio eradication program.
There are three types of polioviruses, and eradication requires that all three disappear. For years, the goal has been tantalizingly close.
Type 2 was declared vanquished in 2015, and Type 3 in 2019. Type 1 now circulates only in Afghanistan and Pakistan. In 2021, the two countries together had just five cases; in 2024, they had 93.
But those figures tell only part of the story. In a surprising twist, an oral vaccine used in some parts of the world has kept poliovirus circulating long after it should have died out.
In most low- and middle-income countries, health officials still rely on an oral vaccine given as two drops on the tongue. It is inexpensive and easy to administer, and it prevents transmission of the virus.
But it contains weakened virus, which vaccinated children can shed into the environment through their feces. When there are enough unvaccinated children to infect, the pathogen slowly spreads, regaining its virulence and eventually causing paralysis.
The problem is this: Since 2016, the oral vaccine used for routine immunization has not protected against Type 2 virus. Global health authorities made a deliberate decision to reformulate the vaccine on the grounds that naturally occurring Type 2 virus had disappeared.
That turned out to be premature. More Type 2 virus had been shed by orally vaccinated children in some parts of the world than officials had anticipated. When some nonimmunized children, or those given the newer oral vaccine, encountered this “vaccine-derived” Type 2 virus, they became infected and paralyzed.
Vaccine-derived poliovirus now paralyzes more children than naturally occurring virus does. For example, Nigeria eliminated all so-called wild-type polio in 2020. But in 2024, the country saw 93 cases of Type 2 vaccine-derived virus, more than one-third the global total.
None of this is a problem for Americans — as long as they are vaccinated.
The inactivated polio vaccine (I.P.V.) used for routine immunization of American children protects against all three types of polio. These formulations contain dead virus, and so cannot cause disease or revert to a dangerous form.
But like some other vaccines for infectious diseases, they do not fully prevent infection or transmission of the virus. This aspect is among the criticisms of Mr. Siri, Mr. Kennedy’s adviser.
Still, it is less important than the vaccines’ near-perfect power to prevent paralysis, experts said.
“Yeah, yeah, it’s true, I.P.V. doesn’t prevent transmission,” said Dr. William Petri, an infectious diseases physician and past president of the W.H.O.’s polio research committee. “But, boy, that’s the best thing since sliced bread at preventing paralysis.”
It does mean, however, that people vaccinated with I.P.V. can keep the virus circulating, even when they themselves are protected against illness and paralysis.
So here’s a realistic scenario that worries researchers: Someone who was vaccinated with the oral polio vaccine in another country might bring the virus into the United States and then shed it, in its weakened form. This has already happened in other countries.
So long as most of the population remains vaccinated, this is not likely to set off an epidemic. But if the virus makes its way into communities with low vaccination rates, it may spread, and then revert to a virulent form that can cause paralysis.
That is what happened in New York in 2022, when polio struck a 20-year-old unvaccinated member of an ultra-Orthodox Jewish community in Rockland County.
The vaccination rate in that county was just over 60 percent, compared with the national average of 93 percent.
The virus that paralyzed the young man had been circulating for months, and it was later detected in the sewage of multiple New York counties with vaccination rates hovering around 60 percent, prompting the state to declare an emergency.
Genetically related polioviruses were detected in wastewater samples in Britain, Israel and Canada, suggesting widespread transmission. The authorities later found two distinct vaccine-derived Type 2 polioviruses in New York wastewater, suggesting two separate importations.
If polio were to re-emerge in the United States, it is unlikely to be as horrific as it was in the pre-vaccine decades. Many older adults still remember that as children they were not permitted to swim in rivers or pools, or anywhere the virus might lurk.
“The reason we weren’t allowed to play in rivers in the ’50s is because raw sewage was dumped into the rivers,” Dr. Heymann said.
That is no longer the case, so there “wouldn’t be massive transmission immediately in the U.S.,” he added.
But even if just a few children were to become paralyzed, “it would be awful.”
Health
RFK Jr.’s MAHA Movement Obscures America’s Unhealthy Past

“We will make Americans healthy again,” Robert F. Kennedy Jr. has declared. A political action committee that has promoted Mr. Kennedy, President-elect Donald J. Trump’s pick for health and human services secretary, says his movement is “igniting a health revolution in America.”
But the word “again” presumes a time in the country’s past when Americans were in better health. Was there ever really a time when America was healthier?
For historians of medicine, there is a short answer.
“No,” said Nancy Tomes, a historian at Stony Brook University.
John Harley Warner, a historian at Yale, said, “It’s hard for me to think of a time when America, with all the real health disparities that characterize our system, was healthier.”
Dr. Jeremy Greene, a historian at Johns Hopkins University, asked: “Which particular era does R.F.K. want to take us back to?”
Probably not the 19th and early 20th century.
Rich men smoked cigarettes and cigars, the poor chewed tobacco. Heavy drinking was the norm.
“It was definitely a drinking culture,” said Dora Costa, an economic historian at the University of California, Los Angeles. “Drinking was a huge problem, saloons were a huge concern. Men were drinking away their paychecks. That is the reason we had Prohibition.”
And, Dr. Costa notes, American diets for most of the 19th century were monotonous.
It’s true that agriculture at the time was organic, food was locally produced and there were no ultraprocessed foods. But fresh fruits and vegetables were in short supply because they were difficult to ship and because growing seasons were so short. For the most part, Dr. Costa said, until the 1930s, “Americans were living off of dried fruits and vegetables.”
As for protein, Americans were relying on salted pork, she said, because meat was difficult to preserve. Only after the Civil War did meatpackers in Chicago begin to process meat and ship fresh beef across the country. At that point, Dr. Costa said, beef “became a large part of the American diet.”
But even though the availability of beef helped diversify diets, people did not become healthier.
Dr. Costa worked with Robert Fogel, the University of Chicago economic historian and Nobel laureate, to understand the health of a population of Americans living in the North around this period by examining the medical records of Union Army soldiers. Common conditions, like hernias, were untreatable — men had hernias as big as grapefruits, held in by trusses. Nineteen percent of those soldiers had heart valve problems by the time they were 60, compared with about 8.5 percent today.
Poor nutrition led to poor health. People were thin, often too thin. In 1900, 6.1 percent of Union Army veterans were underweight — a risk factor for various illnesses and often a marker of ill health — compared with 1.6 percent of U.S. adults today. In 1850, males at age 20 could expect to live to around 61 years. Today it is 74 years.
The start of the 20th century saw public health improvements (cleaner water, for example, and posters advising parents not to give their babies beer), but disease was rampant. There were no antibiotics and very few vaccines. When the 1918 flu struck the nation, no one knew the cause — the flu virus had not been discovered and strange folk remedies were rampant. About 675,000 Americans died. In 1929, the Great Depression began, and its economic toll over the next decade led to severe nutritional and health problems.
Health improved in the second half of the 20th century but was poor compared with that today.
Many people are nostalgic for the 1950s and 1960s, seeing those decades as a time of prosperity, when the American pharmaceutical industry pumped out new medical advances: antibiotics, antipsychotics, drugs for high blood pressure and vaccines for tetanus, diphtheria, measles and polio.
Despite that progress, those years were terrible for health, Dr. Greene said, with “a tremendous amount of heart attacks and strokes.”
Heart disease was rampant in 1950, with 322 deaths per 100,000 Americans annually from cardiovascular disease, double the rate today. By 1960, Dr. Greene said, heart disease, was responsible for one-third of all deaths in America.
In part, that was because nearly everyone smoked.
“We were among the heaviest smoking countries,” said Samuel Preston, an emeritus professor of sociology at the University of Pennsylvania.
Dr. David F. Musto, a medical historian at Yale, who died in 2010, once said in an interview that although he never enjoyed smoking, the social pressure to smoke when he was in college in the 1950s was so great that “I felt it was my duty to find my brand.”
Smoking greatly increases the risk for heart disease, the leading killer in the 1950s and 1960s.
Heart disease death rates plummeted in recent decades because smoking is much less common now, and treatment for heart disease is much more effective. Cholesterol-lowering statins, introduced in 1987, reduced the risk of heart disease. Other new medications as well as bypass surgery and stents also saved lives.
Cancer was the second leading killer in the 1950s, as it is today. But in 1950, there were 194 cancer deaths per 100,000 people. Now there are 142 cancer deaths per 100,000 people.
A decline in smoking is a leading reason, but there also has been a revolution in cancer treatment.
Until the 1990s, cancer was treated with brute force: surgery, radiation and chemotherapy. Now an array of targeted therapies are turning some cancers, once deadly, into treatable chronic diseases or even curing them.
Dr. Greene said he was not surprised by the idea of a halcyon past when people were healthier.
“There’s a long history in America of nostalgia for a past that was better than the present,” he said. “History is all about erasure — the things we don’t choose to remember.”
Today is not a sort of health utopia, of course.
Researchers are quick to acknowledge that Americans’ health is not as good as it can be. And they bemoan the huge disparities in health care in this country.
Yet the U.S. spends more on medical care than other countries — an average of $12,555 per capita, which is about twice what other wealthy countries spend.
But, historians say, the past was actually much worse.
And so, they say, the phrase “Make America Healthy Again” makes no sense.
“As a historian of health, I don’t know what ‘again’ Kennedy is imagining,” Dr. Tomes said. “The idea that once upon a time all Americans were healthy is a fantasy.”
Health
Childhood Vaccination Rates Were Falling Even Before the Rise of R.F.K. Jr.

After years of holding steady, American vaccination rates against once-common childhood diseases have been dropping.
Source: Centers for Disease Control and Prevention
Share of U.S. kindergartners
vaccinated against …
Nationwide, the rate of kindergartners with complete records for the measles vaccine declined from around 95 percent before the pandemic to under 93 percent last year, according to the Centers for Disease Control and Prevention. Immunization rates against polio, whooping cough and chickenpox fell similarly.
Average rates remain high, but those national figures mask far more precipitous drops in some states, counties and school districts.
In those areas, falling vaccination rates are creating new pockets of students no longer protected by herd immunity, the range considered high enough to stop an outbreak. For a community, an outbreak can be extremely disruptive. For children, measles and other once-common childhood diseases can lead to hospitalization and life-threatening complications.
Prepandemic is the average of 2017-18, 2018-19 and 2019-20 data, though not all years were available for all states. Alabama, Florida, Georgia, Iowa, Mississippi, New Hampshire, New Jersey and Delaware (in 2024) report the rate of students who have completed all required vaccines, not just the measles series. Source: Centers for Disease Control and Prevention
Change in kindergarten measles vaccination rates
Immunization rates fell in most states early in the pandemic, and continued to fall in the years that followed.
States, not the federal government, create and enforce their own vaccine mandates, but the incoming Trump administration could encourage anti-vaccine sentiment and undermine state programs. The president-elect’s nominee for health secretary, Robert F. Kennedy Jr., has spread the false theory that vaccines cause autism, among other misinformation.
But immunization rates had been falling for years before Mr. Kennedy’s recent political rise.
There are now an estimated 280,000 kindergartners without documented vaccination against measles, an increase of some 100,000 children from before the pandemic.
“These pockets are just waiting for an introduction of measles,” said Dr. William Schaffner, an infectious disease specialist at Vanderbilt University Medical Center. “It’s trouble waiting to happen.”
Why rates are falling
As the pandemic strained trust in the country’s public health system, more families of kindergartners formally opted out of routine vaccines, citing medical, philosophical or religious reasons. Others simply didn’t submit proof of a complete vaccination series, for any number of reasons, falling into noncompliance.
The shifts in exemptions mostly fall along political lines. In states that supported Mr. Trump for president in November, the number of students with official exemptions have increased on average (rising everywhere but West Virginia). Exemption rates rose in a few states that supported Vice President Kamala Harris — including Oregon, New Jersey and Minnesota — but stayed relatively flat or fell in most.
Includes medical and nonmedical exemptions. Montana was excluded due to lack of data. Wyoming is missing data for 2017-18. Delaware is missing data for 2019-20. West Virginia and Illinois are missing data for 2020-21. Source: Centers for Disease Control and Prevention.Share of kindergartners with a vaccine exemption
The pattern for noncompliance looks different: The rate of children with no vaccination record shot up in both red and blue states.
Not all children with missing records are unvaccinated. Some are in the process of getting their shots, delayed because of the pandemic, and others just never submitted documentation. Schools are supposed to bar out-of-compliance students from attending, but whether they do varies from state to state and school to school.
Montana was excluded due to lack of data. Wyoming is missing data for 2017-18. Delaware is missing data for 2019-20. West Virginia and Illinois are missing data for 2020-21. Alaska is missing data for 2018-19, 2019-20 and 2020-21. Source: Centers for Disease Control and Prevention.Share of kindergartners with no recorded vaccination, and no exemption
Surveys reveal a new and deep partisan division on this issue. In 2019, 67 percent of Democrats and Democratic leaners told Gallup that childhood immunizations were “extremely important,” compared with 52 percent of their Republican counterparts. Five years later, the enthusiasm among the Democratic grouping had fallen slightly to 63 percent. For Republicans and G.O.P. leaners it had plunged to 26 percent.
Today, 31 percent of Republicans say “vaccines are more dangerous than the diseases they were designed to protect.” Just 5 percent of Democrats say the same.
“There seems to be a divide in terms of people’s feelings about science and skepticism towards the government,” said Dr. Natasha Bagdasarian, chief medical executive for Michigan. “I think some of those divisions are becoming apparent in vaccination rates.”
Lawmakers in numerous states have tried to roll back school vaccine mandates, but most changes have been minor: Louisiana required schools to pair any mandate notifications with information about exemption laws; Idaho allowed 18-year-old students to exempt themselves; and Montana stopped collecting data from schools on immunizations.
But there are a few places where state-level policy changes, or lack thereof, appear to have had a direct effect on rates.
In Mississippi, which had long held the country’s highest kindergarten measles vaccination rate, a federal judge ordered the state to allow religious objections; the state’s vaccination rate fell. In contrast, West Virginia’s governor vetoed a bill that would have loosened school vaccine policy; the state now has the highest rate.
Rates rose in Maine and Connecticut, two states that eliminated nonmedical exemptions during the pandemic. They also rose in Alabama, according to C.D.C. data, though the state declined to comment on why.
Vulnerable pockets
Epidemiologists say that when vaccination rates slip under 90 percent for measles, outbreaks become significantly harder to contain. At some point below that, spread becomes almost inevitable if measles is introduced.
There are thousands more schools with vaccination rates below 90 percent compared with just five years ago, according to a New York Times analysis of detailed data from 22 states.
*Texas counts districts, not individual schools.
Most states publish measles, mumps and rubella (MMR) vaccine rates, but several publish only how many students complete all mandated shots. Most states exclude schools with small numbers of students. Most states publish rates for kindergartners only; for several states, however, these rates represent entire schools. New York data excludes N.Y.C. public schools. Source: state governments.
Change in share of schools with vaccination rates below 90 percent
Schools with falling rates can be found in red and blue states, in large urban districts and in small rural ones.
Measles vaccination rates dropped from 83 percent to 75 percent in Yavapai County in Arizona; from 93 percent to 78 percent in Pacific County on the coastline of Washington; from 97 percent to 93 percent in Union County, N.J., just outside New York City — places that span the political spectrum.
These numbers capture vaccination rates only for kindergartners, often partway through the school year, so they include students who may have finished their vaccine series later or will go on to finish it. And across the U.S., most students remain protected against childhood diseases.
But high rates nationally don’t help places no longer protected by herd immunity, as evidenced by recent outbreaks of childhood diseases. Measles and whooping cough cases both climbed last year; polio partly paralyzed a man in New York in 2022.
Growing anti-vaccine sentiment is only part of the public health challenge. In the Minneapolis public schools, completion rates for the measles, mumps and rubella vaccine among kindergartners dropped from around 90 percent to 75 percent. The district’s exemption rate barely moved; instead, far more students had incomplete vaccination records.
Few of those students’ families are strongly anti-vaccine, said Luisa Pessoa-Brandao, director of public health initiatives with the Minneapolis Health Department. Some are immigrants who moved into the district recently, missing either shots or records. Others missed regular doctor visits during the pandemic and got out of the habit of preventative care.
“I think we’re going to be catching up for a while,” Ms. Pessoa-Brandao said.
While vaccination rates were dropping in Minneapolis, they climbed in neighboring St. Paul Public Schools, from around 91.4 percent to around 93 percent, according to state data.
The district attributed the rise to strict new procedures started in 2021, including letters and phone calls to families in their native languages; more vaccines available on district grounds; and monthly compliance reports — an extra mile that not every district is able or willing to go.
There are still parents who opt out. But during a measles outbreak last year, a few changed their mind, said Rebecca Schmidt, the St. Paul district’s director of health and wellness.
“The fear of measles,” she said, “is sometimes greater than the ease” of getting an exemption.
Data for all 50 states
Kindergarten measles vaccination rate
Source: Centers for Disease Control and Prevention. For some years in some states, the rate represents a complete vaccine series, not just the measles vaccine.
-

 Politics1 week ago
Politics1 week agoWho Are the Recipients of the Presidential Medal of Freedom?
-

 Health1 week ago
Health1 week agoOzempic ‘microdosing’ is the new weight-loss trend: Should you try it?
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25822586/STK169_ZUCKERBERG_MAGA_STKS491_CVIRGINIA_A.jpg) Technology5 days ago
Technology5 days agoMeta is highlighting a splintering global approach to online speech
-

 Science3 days ago
Science3 days agoMetro will offer free rides in L.A. through Sunday due to fires
-

 News1 week ago
News1 week agoSeeking to heal the country, Jimmy Carter pardoned men who evaded the Vietnam War draft
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25821992/videoframe_720397.png) Technology6 days ago
Technology6 days agoLas Vegas police release ChatGPT logs from the suspect in the Cybertruck explosion
-

 Movie Reviews1 week ago
Movie Reviews1 week ago‘How to Make Millions Before Grandma Dies’ Review: Thai Oscar Entry Is a Disarmingly Sentimental Tear-Jerker
-

 News1 week ago
News1 week agoTrump Has Reeled in More Than $200 Million Since Election Day















