Northeast
Judge quickly denies request to discard $38 million verdict in New Hampshire youth center abuse case

The judge who oversaw a landmark trial about New Hampshire’s youth detention center has refused to discard the $38 million verdict, saying the facility’s leadership “either knew and didn’t care or didn’t care to learn the truth” about endemic physical and sexual abuse.
A jury earlier this month sided with David Meehan, who alleged he was repeatedly raped, beaten and held in solitary confinement at the Youth Development Center in the 1990s. The attorney general’s office is seeking to drastically reduce the award. While that issue remains unsettled, the state also asked Judge Andrew Schulman to nullify the verdict and issue a judgment in its favor.
CLOSING ARGUMENTS HEARD IN NH YOUTH DETENTION CENTER ABUSE SUIT
In a motion filed Monday, attorneys for the state again argued that Meehan waited too long to sue and that he failed to prove that the state’s negligence led to abuse. Schulman swiftly denied the motion, ruling in less than 24 hours that Meehan’s claims were timely under an exception to the statute of limitations, and that Meehan had proven “beyond doubt” that the state breached its duty of care with respect to staff training, supervision and discipline.
The Sununu Youth Services Center in Manchester, N.H., stands among trees, Jan. 28, 2020. A New Hampshire jury awarded $38 million to the man who blew the lid off abuse allegations at the state’s youth detention center Friday, May 3, 2024, in a landmark case finding the state’s negligence allowed him to be beaten, raped and held in solitary confinement as a teen. (AP Photo/Charles Krupa)
According to Schulman, a jury could easily have found that the facility’s leadership “was, at best, willfully blind to entrenched and endemic customs and practices” that included frequent sexual and physical assaults as well as “constant emotional abuse of residents.”
“Maybe there is more to the story, but based on the trial record liability for negligence and breach of fiduciary duty was proven to a geometric certainty,” he wrote.
Meehan, 42, went to police in 2017 and sued the state three years later. Since then, 11 former state workers have been arrested and more than 1,100 other former residents of what is now called the Sununu Youth Services Center have filed lawsuits alleging physical, sexual and emotional abuse spanning six decades. Charges against one former worker, Frank Davis, were dropped earlier this month after the 82-year-old was found incompetent to stand trial.
Meehan’s lawsuit was the first to go to trial. Over four weeks, his attorneys contended that the state encouraged a culture of abuse marked by pervasive brutality, corruption and a code of silence. The state portrayed Meehan as a violent child, troublemaking teenager and delusional adult lying to get money.
Jurors awarded him $18 million in compensatory damages and $20 million in enhanced damages, but when asked the number of incidents for which the state was liable, they wrote “one.” That trigged the state’s request to reduce the award under a state law that allows claimants against the state to get a maximum of $475,000 per incident.
Meehan’s lawyers say multiple emails they’ve received from distraught jurors showed the jury misunderstood that question on the jury form. They filed a motion Monday asking Schulman to set aside just the portion of the verdict where jurors wrote “one” incident, allowing the $38 million to stand. As an alternative, the judge could order a new trial only on the number of incidents, or could offer the state the option of agreeing to an increase in the number of incidents, they wrote.
Last week, Schulman denied a request from Meehan’s lawyers to reconvene and poll the jury, but said he was open to other options to address the disputed verdict. A hearing is scheduled for June 24.
Read the full article from Here

Northeast
New York AG orders Manhattan hospital to resume gender-transition treatment for transgender youth
NEWYou can now listen to Fox News articles!
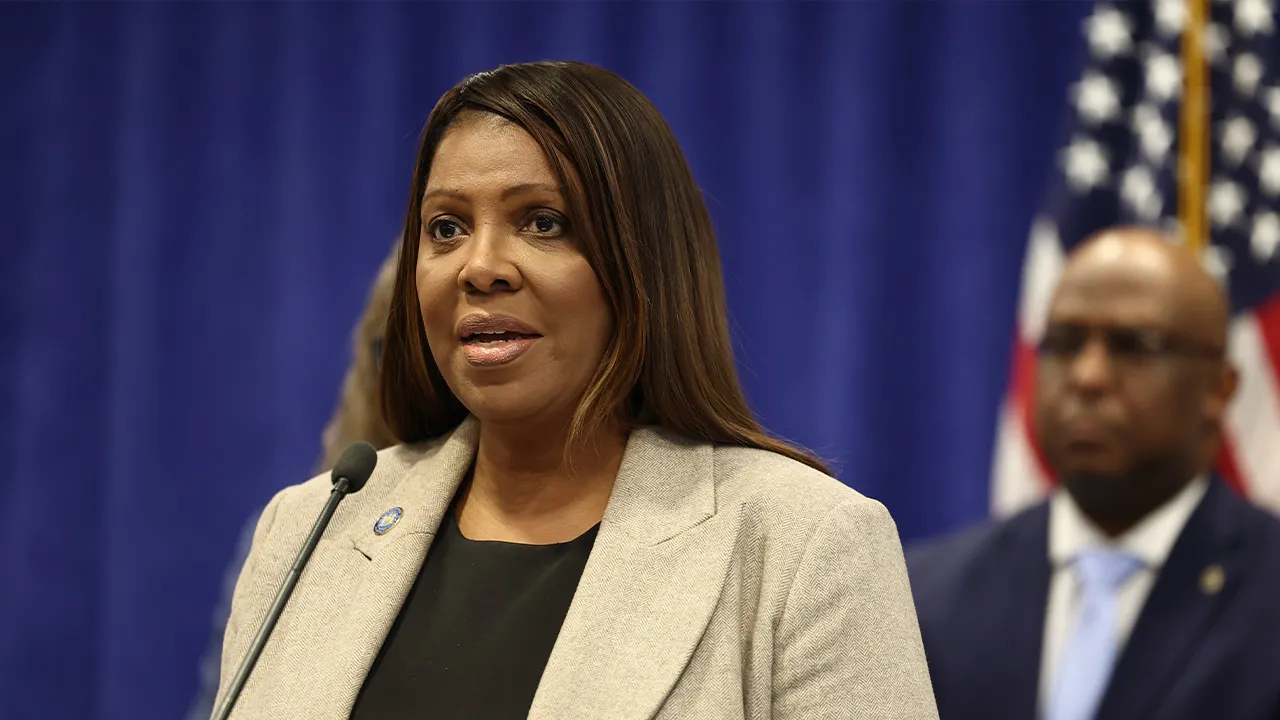
New York Attorney General Letitia James is instructing a Manhattan hospital to resume offering gender-transition treatment to transgender youth after it ended such treatments last month over funding threats from the Trump administration.
NYU Langone’s decision to close its Transgender Youth Health Program violated the state’s anti-discrimination laws by “jeopardizing access to medically necessary healthcare for some of the most vulnerable New Yorkers,” James wrote in a Feb. 25 letter first made public this week.
James’ office threatened “further action” if the hospital does not immediately resume offering hormone therapies, puberty blockers and other treatment to transgender youth.
New York Attorney General Letitia James is instructing a Manhattan hospital to resume offering gender-transition treatment to transgender young people. (Michael M. Santiago/Getty Images)
NYU Langone, one of the city’s largest hospital systems, said last month it would stop providing certain gender-transition treatments for patients under the age of 19.
“Given the recent departure of our medical director, coupled with the current regulatory environment, we made the difficult decision to discontinue our Transgender Youth Health Program,” NYU Langone spokesman Steve Ritea said in a statement at the time. “We are committed to helping patients in our care manage this change. This does not impact our pediatric mental health care programs, which will continue.”
The hospital ceased admitting new patients into its transgender youth program last year after President Donald Trump signed an executive order entitled “Protecting Children from Chemical and Surgical Mutilation,” which aims to restrict gender-transition treatment for people under 19.
The U.S. Department of Health and Human Services has announced a proposal to cut federal Medicaid and Medicare funding to hospitals that provide these treatments to transgender young people. (Andrew Harnik/Getty Images)
Referencing Trump’s order, the U.S. Department of Health and Human Services later announced a proposal to cut federal Medicaid and Medicare funding to hospitals that provide these treatments to transgender youth.
But the Feb. 25 letter signed by the attorney general’s health care bureau chief, Darsana Srinivasan, said the proposal did not officially change federal law and did not affect a “medical institution’s existing duties and obligations under New York law.”
“The sudden discontinuation of medically necessary transgender healthcare can have severe, negative health outcomes,” Srinivasan wrote. “Accordingly, the Attorney General is extremely concerned by your institution’s decision to cease the provision of care to this vulnerable, minority population.”
LETITIA JAMES SUES HHS OVER TYING FEDERAL FUNDS TO TRANSGENDER POLICY
NYU Langone said last month it would stop providing certain gender-transition treatments for patients under the age of 19. (Stephanie Keith/Bloomberg via Getty Images)
CLICK HERE TO DOWNLOAD THE FOX NEWS APP
The letter gives the hospital until March 11 to show its compliance, although it is unclear what steps would be taken if it fails to resume the treatments.
Several other hospitals across the country have also halted transgender youth treatments following Trump’s executive order and funding threats.
The Associated Press contributed to this report.
Read the full article from Here
Boston, MA
Charlotte plays Boston on 5-game win streak

Charlotte Hornets (31-31, ninth in the Eastern Conference) vs. Boston Celtics (41-20, second in the Eastern Conference)
Boston; Wednesday, 7:30 p.m. EST
BETMGM SPORTSBOOK LINE: Celtics -6.5; over/under is 214.5
BOTTOM LINE: Charlotte is looking to keep its five-game win streak alive when the Hornets take on Boston.
The Celtics are 27-13 against Eastern Conference opponents. Boston is sixth in the NBA with 46.2 rebounds led by Nikola Vucevic averaging 8.8.
The Hornets are 19-21 in conference matchups. Charlotte is 7-8 when it turns the ball over less than its opponents and averages 15.0 turnovers per game.
The Celtics average 15.5 made 3-pointers per game this season, 2.7 more made shots on average than the 12.8 per game the Hornets allow. The Hornets average 16.0 made 3-pointers per game this season, 2.1 more made shots on average than the 13.9 per game the Celtics allow.
TOP PERFORMERS: Jaylen Brown is averaging 29 points, 7.1 rebounds and five assists for the Celtics. Payton Pritchard is averaging 17 points and 5.8 assists over the past 10 games.
Kon Knueppel is averaging 19.2 points, 5.5 rebounds and 3.5 assists for the Hornets. Brandon Miller is averaging 22.7 points, 5.3 rebounds and 3.6 assists over the past 10 games.
LAST 10 GAMES: Celtics: 8-2, averaging 109.4 points, 50.7 rebounds, 27.1 assists, 6.1 steals and 6.4 blocks per game while shooting 45.7% from the field. Their opponents have averaged 98.5 points per game.
Hornets: 7-3, averaging 117.3 points, 47.8 rebounds, 27.4 assists, 8.5 steals and 4.2 blocks per game while shooting 45.6% from the field. Their opponents have averaged 106.2 points.
INJURIES: Celtics: Jayson Tatum: out (achilles), Neemias Queta: day to day (rest).
Hornets: Coby White: day to day (injury management).
___
The Associated Press created this story using technology provided by Data Skrive and data from Sportradar.
Pittsburg, PA
2 young girls found dead in suitcases in Cleveland, police say

The bodies of two young girls were found inside suitcases in Cleveland, Ohio, police said on Tuesday.
In a press conference, Cleveland Police Chief Dorothy Todd said on Tuesday that the bodies of the two girls were found in suitcases buried in shallow graves on Monday evening. One of the girls was believed to be between the ages of 8 and 13 years old, while the other was believed to be 10 to 14 years old. Neither girl was identified as of Tuesday night.
“This is a priority,” Todd said during Tuesday’s press conference. “This is a traumatic event for our officers, for the community, and this is just such a tragic incident, but we are trying to develop any leads we can.”
Police said there are no active missing persons reports in Cleveland that match the two victims.
Officials said someone walking their dog near East 162nd Street and Midland Avenue found what appeared to be a body inside a suitcase around 6 p.m. on Monday. When officers responded to the scene near Ginn Academy, they found one of the bodies stuffed in a suitcase in a shallow grave. The second shallow grave with the body stuffed in a suitcase was found after officers searched the area.
“This is a field close to the school over there,” Todd said. “This is just a residential neighborhood that I’m sure a lot of people do frequent.”
The Cuyahoga County Medical Examiner’s Office has custody of the bodies and will identify the girls. Todd said there is no clear indication of possible causes of death for the girls or how long the girls were there.
“It was some time, so it’s not something that was recent,” Todd said.
There is no suspect, Todd added. Anyone with information can contact the Cleveland police at 216-623-5464.
“Usually in residential areas, you know what’s happening in your neighborhood, something just seems a little bit off,” Todd said. “That’s why we’re asking that anyone who has anything that they believe to be information directly related to or suspicious, that they give us a call.”
-

 World6 days ago
World6 days agoExclusive: DeepSeek withholds latest AI model from US chipmakers including Nvidia, sources say
-

 Massachusetts7 days ago
Massachusetts7 days agoMother and daughter injured in Taunton house explosion
-

 Denver, CO7 days ago
Denver, CO7 days ago10 acres charred, 5 injured in Thornton grass fire, evacuation orders lifted
-

 Louisiana1 week ago
Louisiana1 week agoWildfire near Gum Swamp Road in Livingston Parish now under control; more than 200 acres burned
-

 Oregon5 days ago
Oregon5 days ago2026 OSAA Oregon Wrestling State Championship Results And Brackets – FloWrestling
-

 Florida3 days ago
Florida3 days agoFlorida man rescued after being stuck in shoulder-deep mud for days
-

 Maryland3 days ago
Maryland3 days agoAM showers Sunday in Maryland
-

 Culture1 week ago
Culture1 week agoTry This Quiz on Thrilling Books That Became Popular Movies












