Science
If you take an at-home coronavirus test, who keeps track of the results? Probably no one
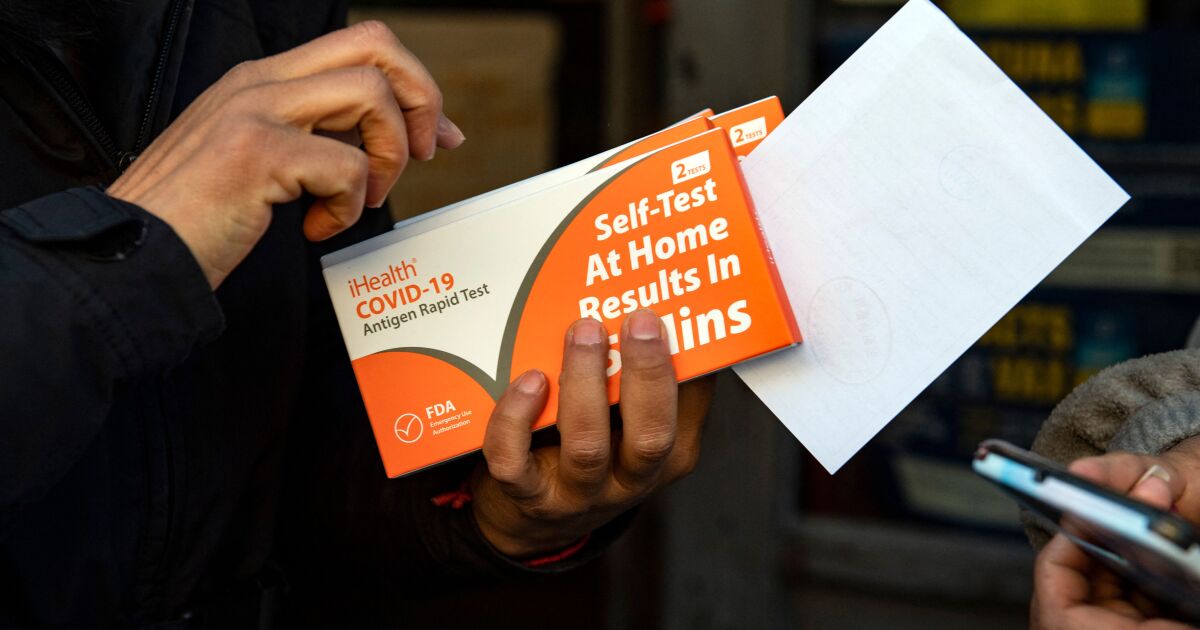
The wildfire-like unfold of the Omicron variant could have impressed you, like many Californians, to snap up a couple of speedy coronavirus check kits — for those who might discover them, that’s.
And whenever you began worrying that you just’d caught the coronavirus, you could have put a kind of kits to make use of. You rigorously swabbed the insides of each nostrils, blended your pattern with a couple of drops of reagent, positioned it on a check strip and waited quarter-hour to see your outcomes.
However after doing all that — and gasping with both aid or dismay — you could have missed the package’s final instruction: to report your outcomes.
Some check kits advise you to name your healthcare supplier. Others need you to make use of the check maker’s app.
Publication
Get our free Coronavirus Right now e-newsletter
Join the newest information, finest tales and what they imply for you, plus solutions to your questions.
You could sometimes obtain promotional content material from the Los Angeles Occasions.
“Dwelling testing results in marked underestimates of case numbers,” Dr. Robert Wachter, chair of UC San Francisco’s Division of Medication, mentioned in an e-mail. “Clearly many lots of of 1000’s of individuals are actually diagnosing themselves with constructive house exams (usually plus signs) and these usually are not reported.”
Even for those who do attempt to report your outcomes, the data isn’t more likely to transfer the needle on the general public’s understanding of the virus. That’s as a result of they’re not included within the knowledge well being officers use to provide their reviews and insurance policies.
So the extra individuals check themselves at house, the much less the official numbers about new infections and positivity charges (that’s, the proportion of exams that detect the virus) will present an correct image of the general public’s well being.
That’s not essentially a foul factor — it’s only a cautionary observe in regards to the knowledge we depend on as we chart a path by means of the pandemic.
Consultants say there’s at all times been a disconnect between the reported coronavirus case counts and the reality. As a result of many individuals who catch the virus expertise few or no signs, many infections go unreported.
Equally, check positivity charges are usually inflated as a result of the individuals probably to indicate up at a testing heart are those with COVID-19-like signs. Giant organizations that require all their members to be examined commonly invariably have decrease positivity charges than websites that check solely individuals who suppose they is perhaps sick.
Testing extra individuals extra typically, as a lot of different developed nations do, might assist establish outbreaks and restrict their unfold. However for a wide range of causes, a rising reliance on at-home speedy exams kits could not assist public well being officers of their battle to trace and perceive the pandemic.
There are a selection of conditions that may immediate individuals to check themselves. The Facilities for Illness Management and Prevention suggests taking a self-test “you probably have COVID-19 signs or have been uncovered or probably uncovered to a person with COVID-19.” (The signs to look out for, the CDC says, embrace fever or chills, cough, shortness of breath, fatigue and sore throat.)
One other good self-test time, the company advises, is earlier than gathering with people who find themselves at better threat of being contaminated, akin to those that are unvaccinated, aged or have weakened immune techniques. Or perhaps you wish to attend an occasion that requires proof of a adverse check.
What do you do after you are taking the check? If it comes again constructive, well being officers say you need to isolate at house, alert the individuals with whom you’ve been in shut contact, and inform your healthcare supplier. The L.A. County Division of Public Well being additionally has a hotline so that you can name — (833) 540-0473 — you probably have questions, want referrals or want assist in notifying your shut contacts.
A division spokeswoman mentioned that “we can be documenting and interviewing those who do name us with constructive outcomes.” However the division doesn’t wish to be contacted about adverse check outcomes.
Nor are well being officers usually together with the house check ends in the confirmed case counts. One cause is that the low-cost speedy exams are antigen exams, whereas clinics and county check facilities use polymerase chain response exams, that are higher at detecting infections of their early phases. Then there’s the query of whether or not individuals taking exams at house are utilizing them appropriately or reporting the outcomes precisely.
“Verification of outcomes is a big problem” for speedy at-home exams, mentioned Gigi Kwik Gronvall, a senior scholar on the Johns Hopkins Middle for Well being Safety. That’s why for those who want a coronavirus check outcome to board a aircraft, she mentioned, “you both have to have a PCR check that was carried out in a lab or you might go to a web site that might provide you with [an antigen] check however it’s verified — any person’s doing it for you and so they see it’s carried out appropriately.”
After some preliminary mix-ups, states are actually reporting any antigen check outcomes they acquire individually from PCR outcomes, Gronvall mentioned.
Dr. Sara H. Cody, Santa Clara County’s well being officer and public well being director, agreed with Wachter that the brand new infections reported by well being officers every day are “an undercount.” However that is probably not as massive a downside as it might have been at first of the pandemic.
Again then, Cody mentioned, well being officers “adopted each case so rigorously” as a result of “it actually, actually mattered in our understanding of the pandemic and informing our coverage selections.” However now, she mentioned, “we’re in a spot within the pandemic that’s fairly completely different.”
Even with restricted testing, officers know that case counts will improve quickly due to the Omicron variant. “What’s most vital to us now,” she mentioned, “is that we measure our hospital assets” to verify individuals who want acute care can get it. And with vaccination and booster charges excessive in her county, Cody added, it’s exhausting to inform at this level how most of the newly contaminated there’ll finally want a hospital mattress.
Wachter, Cody and different well being specialists mentioned policymakers’ focus is shifting away from the reported case counts to different measures, akin to hospitalizations and positivity charges. Granted, positivity charges are thrown off by the exclusion of at-home check outcomes. However Cody mentioned it’s nonetheless significant to have an apples-to-apples comparability of constructive check charges over time.
Santa Clara County has been doing round 20,000 exams a day, and its positivity price was round 1.5% in early December, Cody mentioned. As of Tuesday, she mentioned, it was practically 10.5%.
Regardless of the information points they create, at-home antigen exams are nonetheless an vital complement to PCR exams, Cody mentioned. They alert individuals who have to isolate and “scale back the probabilities that they’re going to go on and infect others, which is vital broadly to public well being.”
In addition to, the L.A. County well being division says, coronavirus case counts aren’t as significant because the developments they reveal.
“As is true with many reportable ailments, the reported numbers have by no means captured all circumstances,” a division spokeswoman mentioned. “However they’ve supplied trendlines for us to raised perceive what is occurring and to contribute to modeling what’s more likely to be probably the most correct numbers.”

Science
Cluster of farmworkers diagnosed with rare animal-borne disease in Ventura County

A cluster of workers at Ventura County berry farms have been diagnosed with a rare disease often transmitted through sick animals’ urine, according to a public health advisory distributed to local doctors by county health officials Tuesday.
The bacterial infection, leptospirosis, has resulted in severe symptoms for some workers, including meningitis, an inflammation of the brain lining and spinal cord. Symptoms for mild cases included headaches and fevers.
The disease, which can be fatal, rarely spreads from human to human, according to the U.S. Centers for Disease Control and Prevention.
Ventura County Public Health has not given an official case count but said it had not identified any cases outside of the agriculture sector. The county’s agriculture commissioner was aware of 18 cases, the Ventura County Star reported.
The health department said it was first contacted by a local physician in October, who reported an unusual trend in symptoms among hospital patients.
After launching an investigation, the department identified leptospirosis as a probable cause of the illness and found most patients worked on caneberry farms that utilize hoop houses — greenhouse structures to shelter the crops.
As the investigation to identify any additional cases and the exact sources of exposure continues, Ventura County Public Health has asked healthcare providers to consider a leptospirosis diagnosis for sick agricultural workers, particularly berry harvesters.
Rodents are a common source and transmitter of disease, though other mammals — including livestock, cats and dogs — can transmit it as well.
The disease is spread through bodily fluids, such as urine, and is often contracted through cuts and abrasions that contact contaminated water and soil, where the bacteria can survive for months.
Humans can also contract the illness through contaminated food; however, the county health agency has found no known health risks to the general public, including through the contact or consumption of caneberries such as raspberries and blackberries.
Symptom onset typically occurs between two and 30 days after exposure, and symptoms can last for months if untreated, according to the CDC.
The illness often begins with mild symptoms, with fevers, chills, vomiting and headaches. Some cases can then enter a second, more severe phase that can result in kidney or liver failure.
Ventura County Public Health recommends agriculture and berry harvesters regularly rinse any cuts with soap and water and cover them with bandages. They also recommend wearing waterproof clothing and protection while working outdoors, including gloves and long-sleeve shirts and pants.
While there is no evidence of spread to the larger community, according to the department, residents should wash hands frequently and work to control rodents around their property if possible.
Pet owners can consult a veterinarian about leptospirosis vaccinations and should keep pets away from ponds, lakes and other natural bodies of water.
Science
Political stress: Can you stay engaged without sacrificing your mental health?

It’s been two weeks since Donald Trump won the presidential election, but Stacey Lamirand’s brain hasn’t stopped churning.
“I still think about the election all the time,” said the 60-year-old Bay Area resident, who wanted a Kamala Harris victory so badly that she flew to Pennsylvania and knocked on voters’ doors in the final days of the campaign. “I honestly don’t know what to do about that.”
Neither do the psychologists and political scientists who have been tracking the country’s slide toward toxic levels of partisanship.
Fully 69% of U.S. adults found the presidential election a significant source of stress in their lives, the American Psychological Assn. said in its latest Stress in America report.
The distress was present across the political spectrum, with 80% of Republicans, 79% of Democrats and 73% of independents surveyed saying they were stressed about the country’s future.
That’s unhealthy for the body politic — and for voters themselves. Stress can cause muscle tension, headaches, sleep problems and loss of appetite. Chronic stress can inflict more serious damage to the immune system and make people more vulnerable to heart attacks, strokes, diabetes, infertility, clinical anxiety, depression and other ailments.
In most circumstances, the sound medical advice is to disengage from the source of stress, therapists said. But when stress is coming from politics, that prescription pits the health of the individual against the health of the nation.
“I’m worried about people totally withdrawing from politics because it’s unpleasant,” said Aaron Weinschenk, a political scientist at the University of Wisconsin–Green Bay who studies political behavior and elections. “We don’t want them to do that. But we also don’t want them to feel sick.”
Modern life is full of stressors of all kinds: paying bills, pleasing difficult bosses, getting along with frenemies, caring for children or aging parents (or both).
The stress that stems from politics isn’t fundamentally different from other kinds of stress. What’s unique about it is the way it encompasses and enhances other sources of stress, said Brett Ford, a social psychologist at the University of Toronto who studies the link between emotions and political engagement.
For instance, she said, elections have the potential to make everyday stressors like money and health concerns more difficult to manage as candidates debate policies that could raise the price of gas or cut off access to certain kinds of medical care.
Layered on top of that is the fact that political disagreements have morphed into moral conflicts that are perceived as pitting good against evil.
“When someone comes into power who is not on the same page as you morally, that can hit very deeply,” Ford said.
Partisanship and polarization have raised the stakes as well. Voters who feel a strong connection to a political party become more invested in its success. That can make a loss at the ballot box feel like a personal defeat, she said.
There’s also the fact that we have limited control over the outcome of an election. A patient with heart disease can improve their prognosis by taking medicine, changing their diet, getting more exercise or quitting smoking. But a person with political stress is largely at the mercy of others.
“Politics is many forms of stress all rolled into one,” Ford said.
Weinschenk observed this firsthand the day after the election.
“I could feel it when I went into my classroom,” said the professor, whose research has found that people with political anxiety aren’t necessarily anxious in general. “I have a student who’s transgender and a couple of students who are gay. Their emotional state was so closed down.”
That’s almost to be expected in a place like Wisconsin, whose swing-state status caused residents to be bombarded with political messages. The more campaign ads a person is exposed to, the greater the risk of being diagnosed with anxiety, depression or another psychological ailment, according to a 2022 study in the journal PLOS One.
Political messages seem designed to keep voters “emotionally on edge,” said Vaile Wright, a licensed psychologist in Villa Park, Ill., and a member of the APA’s Stress in America team.
“It encourages emotion to drive our decision-making behavior, as opposed to logic,” Wright said. “When we’re really emotionally stimulated, it makes it so much more challenging to have civil conversation. For politicians, I think that’s powerful, because emotions can be very easily manipulated.”
Making voters feel anxious is a tried-and-true way to grab their attention, said Christopher Ojeda, a political scientist at UC Merced who studies mental health and politics.
“Feelings of anxiety can be mobilizing, definitely,” he said. “That’s why politicians make fear appeals — they want people to get engaged.”
On the other hand, “feelings of depression are demobilizing and take you out of the political system,” said Ojeda, author of “The Sad Citizen: How Politics is Depressing and Why it Matters.”
“What [these feelings] can tell you is, ‘Things aren’t going the way I want them to. Maybe I need to step back,’” he said.
Genessa Krasnow has been seeing a lot of that since the election.
The Seattle entrepreneur, who also campaigned for Harris, said it grates on her to see people laughing in restaurants “as if nothing had happened.” At a recent book club meeting, her fellow group members were willing to let her vent about politics for five minutes, but they weren’t interested in discussing ways they could counteract the incoming president.
“They’re in a state of disengagement,” said Krasnow, who is 56. She, meanwhile, is looking for new ways to reach young voters.
“I am exhausted. I am so sad,” she said. “But I don’t believe that disengaging is the answer.”
That’s the fundamental trade-off, Ojeda said, and there’s no one-size-fits-all solution.
“Everyone has to make a decision about how much engagement they can tolerate without undermining their psychological well-being,” he said.
Lamirand took steps to protect her mental health by cutting social media ties with people whose values aren’t aligned with hers. But she will remain politically active and expects to volunteer for phone-banking duty soon.
“Doing something is the only thing that allows me to feel better,” Lamirand said. “It allows me to feel some level of control.”
Ideally, Ford said, people would not have to choose between being politically active and preserving their mental health. She is investigating ways to help people feel hopeful, inspired and compassionate about political challenges, since these emotions can motivate action without triggering stress and anxiety.
“We want to counteract this pattern where the more involved you are, the worse you are,” Ford said.
The benefits would be felt across the political spectrum. In the APA survey, similar shares of Democrats, Republicans and independents agreed with statements like, “It causes me stress that politicians aren’t talking about the things that are most important to me,” and, “The political climate has caused strain between my family members and me.”
“Both sides are very invested in this country, and that is a good thing,” Wright said. “Antipathy and hopelessness really doesn’t serve us in the long run.”
Science
Video: SpaceX Unable to Recover Booster Stage During Sixth Test Flight

President-elect Donald Trump joined Elon Musk in Texas and watched the launch from a nearby location on Tuesday. While the Starship’s giant booster stage was unable to repeat a “chopsticks” landing, the vehicle’s upper stage successfully splashed down in the Indian Ocean.
-
Business1 week ago
Column: OpenAI just scored a huge victory in a copyright case … or did it?
-

 Health1 week ago
Health1 week agoBird flu leaves teen in critical condition after country's first reported case
-

 Business6 days ago
Business6 days agoColumn: Molly White's message for journalists going freelance — be ready for the pitfalls
-

 Science3 days ago
Science3 days agoTrump nominates Dr. Oz to head Medicare and Medicaid and help take on 'illness industrial complex'
-

 Politics5 days ago
Politics5 days agoTrump taps FCC member Brendan Carr to lead agency: 'Warrior for Free Speech'
-
/cdn.vox-cdn.com/uploads/chorus_asset/file/25739950/247386_Elon_Musk_Open_AI_CVirginia.jpg)
/cdn.vox-cdn.com/uploads/chorus_asset/file/25739950/247386_Elon_Musk_Open_AI_CVirginia.jpg) Technology5 days ago
Technology5 days agoInside Elon Musk’s messy breakup with OpenAI
-

 Lifestyle6 days ago
Lifestyle6 days agoSome in the U.S. farm industry are alarmed by Trump's embrace of RFK Jr. and tariffs
-

 World5 days ago
World5 days agoProtesters in Slovakia rally against Robert Fico’s populist government